MCQ Flashcards
What is true about the sesamoids?
the tibial sesamoid is larger
Blood supply - medial plantar artery and plantar arch
Sesamoid complex transmits 50% of the body weight
What are the surgical options for a burst fracture?
Anterior decompression with stabilization
Retropulsion with need for decompression
corepectomy with strut grafting
Posterior decompression with fusion
Instrumentation with distraction, get indirect decompression of the canal
Posterior fusion
Progressive kyphotic deformity
Compare two incision distal biceps
both can get PIN
same HO
better flexion with two incision
less LABCN with two incision
What are approapriate antibiotics for open wounds
- Gustilo 1
- cefazolin
- clinda if allergy
- Gustilo 2/3
- cefazolin
- gentamycin
- Farm wounds - penicillin or flagyl
- Freshwater (A hydrophilia)
- cipro or ceftazidime
- Salt water (vibrio)
- Doxycycline
- ceftaxidime or cipro
What is true about NF2?
- less common
- bilateral acoustic neuroma
- no scoliosis
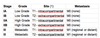
What are the indications for treatment of a pediatric proxiaml humerus fracture?

- Neer-Horowitz classification
- type I is minimally displaced (< 5mm)
- type II is displaced less than 1/3 of the shaft width
- type III is displaced greater than 1/3 and less than 2/3 the shaft width
- type IV is displaced greater than 2/3 the shaft width
-
> 6 with the following displacement
- >50% displaced
- > 45 deg angulated
- open
- dysvascular
Sites of compression of the ulnar nerve at the cubital tunnel
Arcade of struthers
Medial intermuscular septum
Medial epicondyle
Osborne’s ligament
Between heads of FCU (fasica)
Aponeurosis of FDS
What structure causes retrograde ejaculation in the anterior approach to the lumbar spine?
Superior hypogastric plexus
What are the releases for a valgus knee?
osteophytes
Capsule
IT (extension)
popliteus (flexion)
LCL
What is your approach to factor replacement in a hemophiliac
- 2 hours pre op infuse with clotting factor calculated to attain 100% activity of normal
- Then maintained on continuous infusion of factor to maintain levels at >60% throughout the procedure
- Thereafter, levels are checked every 1 or 2 days.
- A 60% level is maintained by continuous infusion until the patient is discharged.
- Home infusion of bolus doses is used to maintain levels of 30% to 60% for at least 2 weeks postoperatively.
- If vigorous physical therapy is needed the patient is infused to a 30% level just before therapy
-
Complications
- hemarthorosis at 4-7 days if it occurs
- infection slightly higher
- risk of stiffness so no concern for instability
Complications of talar neck fractures
- Subtalar OA
- AVN
- malunion
- In that order, no matter the Hawkins classification, but the risk of each one will go up with subsequent grade
- Nonunion is a very low risk
What is the incidence of bilateral slip in a SCFE?
General population - 20%
Renal osteodystrophy - 80%
What injury pattern has the lowest rate of ligament injury in a tibial plateau fracture?
lateral split
Which dwarfism does not have an ustable c-spine?
achondroplasia
What is the most common cause of heel pain in the pediatric population?
Sever’s
Acceptable alignment of a humeral shaft fracture
< 20° anterior angulation
< 30° varus/valgus angulation
< 3 cm shortening
What is true about the genetics and etiology of achondroplasia?
-
FGFR3 point mutation G380R
- AD
-
80% are spontaneous
- associated with higher paternal age
- Leads to abnormal chondroid production in the proliferative zone
- short long bones
- endosteal ossification
- proximal > distal (?why)
- Spine
- narrow interpedicular distance (L1-5)
- narrow foramen magnum
- mortality, apnea, UMN
- screen all with MRI who have positive sleep study
- thoracolumbar kyphosis
- brace when young
- usually will resolve
- lumbosarcral hyperlordosis
- spinal stensosis
- narrow pedicles
- hyperplastic discs
- MSK
- genu varum
- rhizomelic shortening
- trident hand
What structures are released during plantar fascial release
- divide supericial fascia of the abductor hallucis
- fascia between abductor hallucis and plantar quadratus is released
- releases the nerve between the two
- a portion of the plantar fascia is incised
- medial heel spur is resected if present
Treatment of unstable PIP fracture-dislocations
-
Extension block pinning (transarticular)
- reducible joint with tenuous stability
- flex the joint slightly and pin the proximal phalax
-
CRPP
- reducible joint with tenous stability
- larger fragment ammenable to pinning
- not superior to extension pinning
-
Dynamic distraction and Ex-fix
- unstable pilon or > 50% (B type fracture)
- off-loads the joint and permits early ROM
-
Volar Plate arthroplasty
- augmented with button
- proected with k-wire
-
Hemihamate reconstruction arthroplasty (more for volar fractures)
- section of hamate if measured and transplated
- B type fractures can use hemiH or dynamic ex-fix; no studies to compare the two
- 2 week extension splint then ROMAT
- no long term studies
- easier to do in a more chronic situation where you can’t do a DynEx

What is the most common complication of a talar neck fracture?
subtalar OA
What are the indications for epiphyseodesis in congential scoliosis
- Age <5 years
- Site of anomaly in lumbar as opposed to thoracic spine
- A curve of five segments or less
- A progressive curve <40°
- Anomalies consisting of hemivertebrae instead of unsegmented bars
- Absence of excessive kyphosis
- Absence of neurological deficits, including syrinx, diastomatomyelia and tethered spinal cord
What are the MRI characteristics and treatment of an ABC?
- MRI - cystic, fluid-fluid levels showing blood and solid components
- curettage and grafting with cryotherapy
Approach to adolescent bunions
- best to wait until skeletal maturity to operate
- can not perform metatarsal osteotomies if physis is open (cuneiform osteotomy OK)
- surgery indicated in symptomatic patients with an IMA > 10° and HVA of > 20°
- severe deformity with a DMAA > 20 perform a double MT osteotomy
- technique
- soft tissue procedure alone not successful
- similar to adults if physis is closed (except in severe deformity)
What is the most sensitive test to detect OM?
MRI