Tumour Flashcards
Describe this XRay? 15yo boy with painful mass. Differential? Top Diagnosis? Prognosis and Prognostic factors?

EWING SARCOMA
-
Differential
- ewing
- osteosarcoma
- less likely
- leukemia
- rhabdomyosarcoma
- neuroblastoma (<5yo)
- Ewing Sarcoma
- 5-25 years of age
- second most common bone tumor in children
- ~50% are found in the diaphysis of long bones
-
t(11:22) translocation
- found in all cases
- leads to the formation of a fusion protein (EWS-FLI1)
- can be identified with PCR and useful to differentitate Ewing sarcoma from other round cell lesions
-
Prognosis
-
survival
- 60-70% long term survival with isolated extremity disease at presentation and appropriate treatment/tumor response to chemotherapy
- 40% long term survival with pelvis lesions
- 15% long term survival if patient presents with metastatic disease
-
poor prognostic factors
- spine and pelvic tumors
- tumors greater than 100cm3
- < 90% necrosis with chemotherapy
- elevated lactic dehydrogenase levels
- p53 mutation in addition to t(11:22) translocation
-
survival
16yo female with painful thigh. Top Diagnosis? How will she present to you? Radiographic findings typical of this?

Ewing Sarcoma
-
Presentation
- pain often accompanied by fever
- often mimics an infection
-
Physical exam
- swelling and local tenderness
-
Radiographs
- large destructive lesion in the diaphysis or metaphysis with a moth-eaten appearance
- Most common diaphyseal lesion
- Common in pelvis
- lesion may be purely lytic or have variable amounts of reactive new bone formation
- periosteal reaction may give “onion skin” or “sunburst” appearance
- Codman’s triangle
- associated soft tissue mass
-
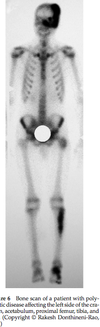
Bone scan
- required as part of staging workup - will show very “hot” lesion
-
MRI
- neccessary to identify soft-tissue extension and marrow involvement
- often shows a large soft tissue component
-
CT chest
- is required for appropriate staging to look for pulmonary metastasis
12 yo male comes in with fever, and painful left hip. Below is his XR. Diagnosis? Managment? Treatment?

Ewing Sarcoma
-
Differential
- infection
- leukemia
- osteosarcoma
- neuroblastoma (if young)
-
Radiology
- permative, moth eatten appearance
- diffuse, aggressive, lytic lesion with periosteal reaction
- may be evidence of onion skinning or sunburst
- ill defined margins, associated soft tissue mass
-
Further work-up
-
Labs - ESR, CRP, WBC, CBC and smear, LDH
- ESR is elevated
- WBC is elevated
- anemia is common
- lactic dehydrogenase (LDH)
-
Bone marrow biopsy
- required as part of workup for Ewing’s to rule out metastasis to the marrow
- also assesses for translocation; translocation in normal marrow has increased risk of relapse
-
Molecular Analysis
- CD99
- PCR can confirm - 11, 22 translocation
-
Bone scan - hot
- __assess mets
-
MRI - assess soft tissue mass
- __marrow involvement
-
CT chest - assess pulmonary mets
- __can help to plan radiation
-
Labs - ESR, CRP, WBC, CBC and smear, LDH
- Consult pediatric oncology and rad onc to discuss imaging
-
Treatment is multi-modal
- preoperative chemotherapy given for 8-12 weeks (3 drugs)
- doxyrubicin (cardiotoxicity)
- vincristine
- cyclophosphamide
- isophosphamide
- etoposide
- Restage with MRI to assess response
- >90% necrosis is good prognosis
- Wide surgical resection with limb salvage or amputation
- Positive margins - re-resection and consider radiation
- OR Radiation if difficult area, but this is falling out of favour due to long term complications
- nonresectable tumor
- wide metastatic disease
- maintenance chemotherapy for 6-12 months
- Monitor for recurrent disease every three months for 2 years, then reduce intervals
- preoperative chemotherapy given for 8-12 weeks (3 drugs)

Poor prognostic factors associated with Ewings
-
The most important factor is clincially evident metastatic disease
- mets to lungs is better than distant boney mets
- skip lesions better than distant boney mets
-
Location
- spine and pelvic tumors (distal tumors have a better prognosis)
-
Size
- tumors greater than 100cm3
- or >8cm
- Age >14 yo
- Male
-
LDH >200IU
- CRP/WBC elevation may be associted with mets and higher tumor burden
- < 95% necrosis with chemotherapy
- p53 mutation in addition to t(11:22) translocation
- Relapse at < 2years
What is important for staging Ewings?
- All present as stage IIb or III
- plain radiographs and MRI of the primary site
- CT chest - pulmonary mets
- Bone Scan - skip lesions, boney mets
- Bone marrow biopsy
- ESR, CRP, LDH
Treatment of Ewings
- preoperative chemotherapy given for 8-12 weeks (3 drugs)
- doxyrubicin (cardiotoxicity)
- vincristine
- cyclophosphamide
- isophosphamide
- etoposide
- Restage with MRI to assess response
- Wide surgical resection with limb salvage or amputation
- Send to pathology to assess for margins and amount of necrosis
- >90% necrosis good prognosis
- positive margins = RT
- OR Radiation if difficult area, but this is falling out of favour due to long term complications
- nonresectable tumor
- wide metastatic disease - should irradiate lungs even when improves with chemo
- technique
- 2-3 cm margin
- 60 grey
- maintenance chemotherapy for 6-12 months
- Monitor for recurrent disease every three months for 2 years, then reduce intervals
- Relapse is common
- treatment associated AML (5 years)
- treatment associated myelosysplasia
- sarcoma 2nd to radiation (10 years); 20%
- carcinoma
Complications associated with radiotherapy in children
- limb length discrepany
- joint contracture
- muscle atrophy
- pathological fractures
- secondary malignancy
Two class of criteria you can use to decide wether to prophylactically fix this?

Harington Critera
- > 50% destruction of diaphyseal cortices
- > 50-75% destruction of metaphysis (> 2.5 cm)
- Permeative destruction of the subtrochanteric femoral region
- Persistent pain following irradiation
Mirel’s Criteria

What is the most common site of metastatic cancer?
thoracic spine
Always make sure to ask about neurological symptoms in any lesion that could be mets
A patient with metastatic disease present with confusion, lethary, polyuria, N/V and are severaly dehydrated. What is the diagnosis? What is the treatment?
Hypercalcemia
- Loop diuretics
- fluid resussitation
Principles of tumor biopsy
-
Prerequisites
- CBC, INR, PTT
- Imaging
- XR, CT
- MRI - to look at most appropriate site of lesion
-
Indications
- bone tumor
- Where multiple sites need biospy (because of tumor heterogeneity)
- Call your nearest tumor specialist to confirm you are dong appropriate biopsy, or ask if they would like referal
-
Incision
- Keep the incision as small as possible
- use longitudinal incision in the extremities
- allows for extension of the incision for definitive management
-
Approach
- do not expose neurovascular structures
- all tissue exposed during the biopsy is considered contaminated with tumor
- maintain meticulous hemostasis
- release tourniquet prior to wound closure
-
Biopsy
- perform thru the involved compartment of the tumor, if possible threw one muscle
- for bone lesions with a soft tissue mass, it is ok to perform the biopsy using the soft tissue mass
- Make a circular or longitudinal hole, <10% bone diameter
- Confirm with your pathologist that you have adequate specimen
-
Closure
- if using a drain, bring drain out of the skin in line with surgical incision
- layered tension-free closure

Prognosis and characteristics of common metastatic cancer?
Thyroid (lytic) - 48 months
Prostate (blastic) - 40
Breast (mixed) - 24
Kidney (lytic) - variable
Lung (lytic) - 6 months
myeloma (lytic) - 2-5 years
Work-up of this patient

-
History
- Pain, qualify the pain, other sites of pain
- This is the most common presenting symptoms
- Constitutional symptoms or specific symptoms to any carcinoma
- Chest pain, abdominal bloating, intolerance to hot and cold
- Neurological symptoms
- Myelopathy, weankness, walking aids, bowel/bladder
- Risk factors - smoking, family history
- Last pap smear, mammogram, colonoscope
- Pain, qualify the pain, other sites of pain
-
Physical
- Look for evidence of primary
- Breast exam, thyroid mass, prostate (rectal)
- Costovertebral tenderness = renal call
- Look for evidence of mets
- Ascultate the lungs, palpate the abdomen
- Abdomenal exam
- Full neurological exam including gait, ASIA
- Look for evidence of primary
-
Workup for older patient with unknown primary
- Plain radiographs
- Full length films of lesion, chest
- CT chest/abdo/pelvis
- Can consider head
- Technetium bone scan - rule out other lesions
- Skeletal survery - Myeloma and thyroid cancer - cold bone scan
- Plain radiographs
-
Blood
- CBC and differential, ESR/CRP, INR, PTT
- LFT, Cr/Urea
- Ca, Phos, Alk Pho, LDH
- ***Hypercalcemia can be fatal to patient
- Helps to rule out metabolic bone disease (hyperparathyroid)
- Immunoelectrophoresis - SPEP, UPEP
- PSA, TSH
-
Imaging
- Radiographs - full length films of affected area
- Blastic - Prostate > breast > lung
- Lytic - renal, lung, thyroid, uterine, adrenal, melanoma, GI
- Not responsive to rads/chemo
- Usually need to treat operatively
- Elbow or knee = lung or renal
- Cortical = lung
-
Biopsy
-
Indications to rule out primary
- No history of cancer
- History of cancer with no evidence of mets
- When there is history of cancer and evidence of mets, ok to send reamings for path
- See the principles of biopsy section
- Use the easiest site to biopsy
- Can do a frozen section intra-op and if the pathologist confirms carcinoma you can proceed with fixation
-
Indications to rule out primary
-
Histology
- Mets - epithelial cells in clumps or glands in a fibrous stroma
- Immunohistochemical stains positive
- Keratin
- CK7 - breast, lung
- TTF1 - lung
-
Once you have the primary
- Med Onc - chemo
- Rad Onc - post-op radiation
- Radiology - if you want them to be embolized pre-op
Treatment prinicples of metastatic lesion
-
Non-op
- Indications
- Small lesions with little disability
- Upper extremity
- Sensitive tumors
- Blastic lesions
- Short expected survival or short condition
- Bisphosphanate - have been shown to decrease secondary skeletal events (SSE) - funded fr breast, myeloma and prostate
-
Radiation
- All require post-op unless death is imminent - otherwise you risk reoperation
- Begin radiation after surgery - 3 weeks
- Make sure you close your wounds well and can leave in the sutures
- Radiation needs to include the entire fixation device
-
Chemo
- Lymphoma/leukemia are very sensitive to rads/chemo so you usually don’t need to do sx
- Indications
-
Operative
- Get imaging of the full bone including joint above and below
- CT may be necessary
- Embolization - renal cell, thyroid
- Post-op RADS - helps to minimize recurrence and for pain control
-
Indications
- Femur fractures
- >2.5cm
- >50% cortical lesion
- Pain refractory to rads
- Mirel’s criteria
-
Hemiarthroplasy or tumor prosthesis
- Required when there in an intra-articular, uncontained lesion
- Can also be done for a proximal femoral neck fracture
- Cemented
- Considerations
- Soft tissue deficient and instability
- Adequate closure of capsule, abductors and ER’s
- High risk of infection
- Soft tissue deficient and instability
-
Prophylactic nailing
- Statically locked
- Recon nail has a higher failure rate for both intertroch and subtroch
- Can augment with PMMA
- Don’t forget to vent the femur if there is no fracture when reaming
- *Doing more than one intramedullary device for multiple lesions can put a lot of stress on the pulmonary system - might be better to stage multiple lesions and allow the patient to recover from each nail
-
ORIF with PMMA
- Indications
- Humerus diaphyseal or metaphyseal with uncontained defect
- Tibia - metaphyseal defect that is extra-articular
- Impending and complete fractures
- Curettage, cement, screw into cement
- Indications
- Get imaging of the full bone including joint above and below
- Spinal neurologic decompression, surgical stabilization, post-op radiation therapy
- Met lesions to spine with compression of neuro elements
Treatment of humeral lesions

Treatment of tibial lesions

Tumors that require chemo
-
Indications
- osteosarcoma (intramedullary and periosteal)
- Ewing’s sarcoma/primative neuroectodermal tumor
- malignant fibrous histiocytoma
- mesenchymal chondrosarcoma
- Rhabdomyosarcoma
- Synovical cell
-
Timing
- pre-op 8-12 weeks
- post-op 6-12 months
-
Common Drug
-
Doxorubicin
- anthracycline antibiotic
- functions as a cytostatic agent
- side effects
- cardiac toxicity
-
Doxorubicin
Describe the lesion. Differential? Diagnosis? Associated conditions?
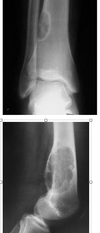
Non-ossifying fibroma
-
Differential for larger NOF
- ABC
- Chondromyxoid fibroma
- Fibrous dysplasia
- Desmoplastic fibroma
-
Associated conditions
-
Jaffe-Campanacci syndrome
- congenital syndrome of multiple non-ossifying fibromas and
- cafe au lait pigmentation
- mental retardation
- heart, eyes, gonads involved
- neurofibromatosis
- familial multifocal NOF
- ABC
-
Jaffe-Campanacci syndrome
Describe this XR. Differential? Diagnosis?

Differential for metaphyseal fibrous defect
Osteoid osteoma
Intracortical abcess
Stress fracture
Intracortical osteosarcoma
Describe this XR? Differential? Diagnosis? Treatment?

Non-ossifying Fibroma
-
Radiographs
- diagnostic
- metaphyseal, eccentric, “bubbly” lytic lesion surrounded by sclerotic rim
- cortex expansion and thinning
- as bone grows
- migrates to diaphysis
- lesions enlarge (1-7cm)
- lesions become sclerotic as patient approaches skeletal maturity
- avulsion of adductor magnus insertion in the posteromedial aspect of the distal femur may produce a similar looking lesion.
-
CT
- quantitative CT shown to be useful in predicting fracture risk
-
observation
- first line of treatment
- most lesions resolve spontaneously and observation alone is the treatment for most cases
-
casting
- pathologic fracture
- can be treated as per the fracture alone (long leg casting for distal femur pathologic fx)
- Once fracture heals treat with curettage and bone grafting
-
intralesional curettage and bone grafting
- symptomatic and large lesion
- increased risk of fracture shown on quantitative CT
Describe the XR. Differential? Managment?

Malignant Fibrous Histiocytoma
- 20-30% arise from infection or implant
- usually >50yo
-
Presentation
- pain, swelling, pathological fracture
-
Imaging
-
lytic
- no evidence of cortical reaction; too fast for bone to respond
- destructive
- metaphyseal
-
lytic
-
Mangement
- requires a complete WU of solitary bone lesion
- ensure no hypercalcemia
- MRI to look at soft tissue invovlement
- biopsy to confirm
-
Treatment
-
multi-agent chemotherapy and limb salvage resection
-
chemotherapy
- preoperative 8-12 weeks
- maintenance 6-12 months
-
surgical resection
- trend towards limb salvage whenever possible
-
chemotherapy
-
multi-agent chemotherapy and limb salvage resection
Differential for multiple lesions in a young adult
EG
Fibrous dysplasia
Leukemia
Lymphoma
Hemangioendothelioma
Enchondroma / Olliers / Marfucci’s
Osteochondroma / MHE
NOF / Jaffe-Campanacci syndrome
Differential for multiple lesions in an older adult
Paget’s
Metastatic bone disease
Multiple myeloma
Lymphoma
Hyperparathyroidism
Bone infarcts
Lesions that have a cold bone scan
multiple myeloma
melanoma
Sacral lesions < 40
Giant cell tumor
ABC
Ewing’s
Osteosarcoma
Sacral lesions 40-80
Chordoma
Metastasis
Myeloma
Lymphoma
Chondrosarcoma
MFH
How to assess an XR for a tumour
- Age
-
Location
- Epiphyseal vs metaphyseal vs disphyseal
- Medullary vs cortical
- Geographic vs Permative - geographic will stay with-in the lesion
-
What is the tumor doing to the bone?
- Lytic vs blastic
- infiltrative - moth eatten, permeative
-
What is the bone doing to the tumour?
- Cortical reaction - expansile, sclerotic rimming, lysis
- Periosteal reaction
- Onion skinning, sunburst, spiculated
-
Mineralization/Matrix
- Ground glass
- calcification
- Size and number
- Associated soft tissue mass
Differential diagnosis by location
-
Surface lesions
- Osteochondroma
- Periosteal chondroma
- Surface ABC
- Parosteal osteosarcoma
- Surface chondrosarcoma
-
Epiphyseal
- chondroblastoma
- Chondrosarcoma
- OM
-
Epiphyseal-Metaphyseal
- GCT
- ABC
-
Metaphyseal
- Unicameral bone cyst
- Osteosarcoma
- Enchondroma
- Chondrosarcoma
- Chondromyxoid fibroma
- Non-ossifying fibroma
-
Diaphyseal
- Osteoid osteoma
- Osteoblastoma
- Stress fracture
- OM
- Fibrous dysplasia
- Adamatinoma
- Ewings
-
Periarticular
- Synovial chonromatosis
- PVNS
- NOT synovial sarcoma

Most common tumour of the sacrum?
chordoma
What is the most common malignant spinal tumour in adults?
chordoma
Differential? How can you confirm you diagnosis?

Chordoma
-
Differential
- Plasmacytoma
- Cold on bone scan
- OM, Lymphoma
- More acute onset with systemic features
- Chondrosarcoma, mets
- Will have associated soft tissue mass
- Plasmacytoma
- Histology
- characterized by foamy, vacuolated, physaliforous cells
- grows in distinct nodules
-
histochemical staining
-
keratin positive
- important to distinguish from chondrosarcoma which is not keratin positive
-
weakly S100 positive
- can distinguish from adenocarcinoma
-
keratin positive
- characterized by foamy, vacuolated, physaliforous cells
Differential? Diagnosis? Typical Presentation? Treatment/Managment?

Chordoma
-
Differential
- Chordoma
-
Plasmacytoma
- Cold on bone scan
-
OM, Lymphoma
- More acute onset with systemic features
-
Chondrosarcoma, mets
- Will have associated soft tissue mass
-
Presentation
- insidious onset of pain
- often complain of bowel or bladder changes
- sensory deficits rare due to distal nature of tumor
- gastrointestinal - constipation, fecal incontinence
-
Physical exam
- neurologic
- motor deficits rare because most lesions at S1 or distal
- bowel and bladder changes are common
-
rectal exam
- more than 50% of sacral chordomas are palpable on rectal exam
-
Work up
- CBC and diff, lytes, Cr, Urea, INR, PTT, SPEP, UPEP
- Radiographs
- often difficult to see lesion due to overlying bowel gas
- CXR for staging
- CT - chest/abdo/pelvis
- local staging
- will show midline bone destruction and soft tissue mass
- calcifications often present within the soft tissue lesion
- MRI
- bright on T2
- useful to evaluate soft tissue extension
- Bone scan
- other bony sites of metastasis
- Hot on bone scan, which is different from plasmacytoma
-
Biospsy
- physoliferous cells
- postivie keratin staining
- S100 positive
- Consult orthopedic oncology team, radiation oncology
-
radiation treatment
- inoperable tumors
-
wide margin surgical resection +/- radiation
- standard of care in most patients
- technique
- must be willing to sacrifice sacral nerve roots to obtain adequate surgical margins
- add radiation if margin not achieved
- outcomes
- long-term survival 25-50%

What is the most important factor in the prognosis of chordoma
local recurrence
reduced by en bloq excision
Diagnosis? Differential? Treatment?

UBC with path#
-
Differential
- UBC, ABC
- ABC is usually wider then the epiphysis
- Fibrous dysplasia
- Enchondroma
- telanectaticosteosarcoma
- Intraosseous ganglia
- UBC, ABC
- Classification is important as it impacts treatment
- active - if cyst is adjacent to the physis
- latent - if normal bone separates cyst from physis
- 50% present with pathological fracture, otherwise painless
-
Observation
- If the patient is assymptomatic and the fracture is not in a weight bearing bone you may be able to observe the cyst every 2-3 months. As the patient approaches skeletal maturity it may resolve
-
Immobilization alone
- proximal humerus lesions with pathologic fracture (15% of lesions fill in with native bone after acute fracture)
- Healing is defined as >95% opacification of the cyst with cortical thickening
- Incomplete is <80% with no cortical thickening
- proximal humerus lesions with pathologic fracture (15% of lesions fill in with native bone after acute fracture)
-
Aspiration and methylprednisolone acetate injection
- active cysts (communicates with physis) in the proximal humerus
- technique
- usually requires several injections, especially in very young children
- bone marrow injections have recently been reported to be effective, but have not yet been proven to be superior to steroid injections
- Recurrence rate is 15-88%
-
curettage and bone grafting +/- internal fixation based on tumor location
- contraindications
- active lesion next to physis as will cause growth arrest
- indications
- symptomatic latent cysts that have not responded to steroid injections
- latent cysts in the proximal femur that are a structural concern and at risk for fracture and osteonecrosis
- proximal femoral lesions with a pathologic fracture have a high rate of refracture and malunion when treated nonoperatively
- Technique
- Approach the bone, drain the cyst and currette out the fibrous lesion
- Pack with graft
- Allograft versus autograft versus simulated is dealers choice
- Structural support often necessary, this is usually done with plates
- Consider open physes
- contraindications
-
Recent innovations
- There is some recent literature to support decompression with a flexible nail that has had good results
- A second procedure is needed to remove the nail
- Some have combined this with calcium sulphate graft with good outcomes
- Helps with follow-up because it is radio-opaque, so easier to assess for recurrence
- There is some recent literature to support decompression with a flexible nail that has had good results
-
Recurrence rate
- reported to be as high as 45%
- >90% in patients >10 heal, only 60% patients <10
- Lesions <2cm from physis have a higher risk of injury
- reported to be as high as 45%
-
Complications
- Local reaction to material used to fill the cavity
- Pathological fracture
- Growth disturbance

Recurrence rate of UBC
- <10% fill in with fracture (15% in orthobullets)
-
Recurrence rate
- reported to be as high as 45%
- >90% in patients >10 heal, only 60% patients <10
- Lesions <2cm from physis have a higher risk of injury
Complications associated with UBC
-
Complications with femur fractures
- Varus malunion
- Growth arrest
- Femoral head osteonecrosis
-
Complications
- Local reaction to material used to fill the cavity
- Pathological fracture
- Growth disturbance
- recurrence
Diagnosis? Differential? Common presentation?

- A non-neoplastic, serous fluid-filled bone lesion thought to result from temporary failure of medullary bone formation near the physis
- usually found in patients <20 years of age
- usually found in the proximal humerus
- can be found in other locations including proximal femur, distal tibia, ilium, calcaneus, and occasionally metacarpals, phalanges, or distal radius
- arises in the metaphysis adjacent to physis and progresses toward the diaphysis with bone growth
-
Prognosis
- as a patient approaches skeletal maturity, a UBC will often decrease in size and may heal after growth is complete
- fracture healing usually does not lead to cyst resolution (<10%)
-
Pathoanatomy
- Unknown etiology
- Due to fluid build up with-in the bone that causes resorption
- May be due to vascular occlusion secondary to high pressure
- Some research to suggest that lowering interstitial pressure will cause involution
-
Differential
- UBC, ABC
- ABC is usually wider then the epiphysis
- Fibrous dysplasia
- Enchondroma
- Occurs more in the tubular bones of the hands and feet
- Intraosseous ganglia
- telangectatic osteosarcoma
- UBC, ABC
-
Typical XR findings
- central, lytic, well-demarcated metaphyseal lesion (2-3% cross physis)
- cystic expansion with mild symmetric thinning of cortices
- “fallen leaf” sign (pathologic fracture with fallen cortical fragment in base of empty cyst is pathognomonic)
- trabeculated appearance after multiple fractures
- MRI shows rim enhancement of the sclerotic rim
Treatment?

UBC of proximal femur
-
Cutettage, bone grafting and fixation for proximal femur fractures
- Classified and treated based on the amount of bone deficit
- Should be immbolized with a hip spica for younger patients
- In type IA, a cyst of moderate size present in the middle of the femoral neck. The lateral buttress is intact, and sufficient bone is available in the femoral neck and lateral proximal femur to allow fixation with cannulated screws.
- In type 1B, a large cyst is present at the base of the femoral neck. The lateral buttress is compromised; therefore, the use of a pediatric hip screw and side plate should be considered
- Types IIA (C) and 11B (D) are characterized by a krge bsion in the femoral neck.
- In type IllA, the lateral buttress is present, and cannulated screws can be used to stabilize the fracture.
- In type 111B, the loss of the lateral buttress requires the use of a pediatric hip screw and a side plate for fixation following curettage and bone grafting.
-
Complications with femur fractures
- Varus malunion
- Growth arrest
- Femoral head osteonecrosis

Differntial. Diagnosis? Common presentation and findings on imgaing

ABC
-
Differential
- Radiographic differential includes
- UBC
-
telangiectatic osteosarcoma
- Will usually have thicker, nodular rimming on MRI
- Histologic differential includes
- telangiectatic osteosarcoma
- Will have evidence of peiomorphism
- giant cell tumor
- telangiectatic osteosarcoma
- Radiographic differential includes
- A benign and non-neoplastic reactive bone lesion filled with multiple blood-filled cavities
- can be locally destructive to normal bone and may extend to soft tissue
- 75% of patients are < 20 yrs.
-
Radiographs
- expansive, eccentric and lytic lesion with bony septae (“soap-bubble appearance”)
- usually in metaphyseal
- Proximal tibia and distal femur
- most common tumor of the posterior elements of the spine
- classic cases have thin rim of periosteal new bone surrounding lesion
- no matrix mineralization
-
MRI or CT scan
- will show multiple fluid lines
- Characteristic but not pathognomonic
- Also see with GCT, Telangectatic osteosarcoma
- lesion can expand into soft tissue
-
Histology
-
Incisional biopsy is the standard
- FNAB does not provide adequate specimen, especially considering the high incidence with other neoplasms
- Characteristic findings
- cavernous space
- blood-filled spaces without endothelial lining
- cavity lining
- numerous benign giant cells
- spindle cells
- thin strands of woven (new) bone present
- ***Important do diff from telangectatic osteosarc - which will see peliomorphism
-
Incisional biopsy is the standard

Differential ABC from TSO
-
Aneurysmal Bone Cyst
- 10–20
- Femur, tibia, fibula, humerus
- Blood-filled spaces separated by thin fibrous septa with benign-appearing spindle cells Osteoid with or without osteoblastic rimming
- Inflammatory cells and giant cells may be present
- Curettage with adjuvant sclerotherapy, emobo- lization, or en bloc resection
-
Telangectatic osteosarcoma
- 10–20
- Distal femur, proximal tibia, proximal humerus
- Blood-filled spaces separated by thicker fibrous septa, with malignant-appearing cells more easily noted at higher magnification
- Pleomorphism, atypical mitotic figures, and possible osteoid formation
- Neoadjuvant chemotherapy, wide surgical resection and reconstruction, postoperative chemotherapy
Diagnosis? Treatment?

ABC
- Discuss with an experienced MSK radiologist and pathologist to ensure this is not TOS before proceeding
-
nonoperative fracture management
- ABC with acute fracture
- indicated until fracture has healed. Once healed, treat as an ABC without fracture unless the fracture has led to spontaneous healing of the ABC
-
aggressive curettage and bone grafting
- symptomatic ABC without acute fracture
- technique
- some use adjuvant treatment (phenol)
- Better result if you are more aggressive - ie; high speed burr
- outcomes
- local recurrence in up to 25% and more common in children with open physes
- >12
- Open physes
- High component of cellular content
- Mitotic index >7 per 50 feilds
- local recurrence in up to 25% and more common in children with open physes
-
Sclerotherapy
- Some reports of reduced recurrence compared to curettage
- Others not reduced recurrence, but better functional outcomes and reduced complications
- Ethibloc is associated with a fatal cerebellar infarct and should not be used as first line treatment
- Embolization with experimental results
-
En bloc resection
- Recommended to reduce recurrence rates in bones that are expendable (fibula/clavicle)

Risk factors of recurrence with ABC
>12
Open physes
High component of cellular content
Mitotic index >7 per 50 feilds
Classification of ABC
- Type I lesions are centrally located and well contained, with either no outline or a slightly expanded outline
- Type II lesions have marked expansion and cortical thinning with involvement of the entire bony segment.
- Type III lesions are eccentric and metaphyseal and typically involve only one cortex.
- Type IV lesions are the least common subgroup and develop subperiosteally, expand- ing away from the bone
- Type V lesions occur periosteally and expand peripherally, ultimately penetrating cortical bone.

Describe this XR. Differential? Epidemiology of top diagnosis.

Giant cell tumor
-
Differential for epiphyseal lesions
- GCT, ABC, TOS
- Chondroblastoma
- Interosseous ganglia
- Clear cell chondrosarcoma
- A benign aggressive tumor typically found in the epiphysis of long bones
- F>M (unlike most bone tumors which show male predominance)
- ages 30-50 years
-
Knee>sacrum>distal radius
- 50% occur around knee (distal femur or proximal tibia)
- 10% in sacrum and vertebrae
- while GCT can rarely occur in the spine, it usually usually occurs in the vertebral body
- phalanges of the hand is also a very common location
- may arise in the apophysis (like chondroblastoma)
-
Malignant potential
-
primary malignant giant cell tumor
- metastatic to lung in 2-5%
- hand lesions have greater chance of metastasis
-
secondary malignant giant cell tumor (15%)
- occurs following radiation or multiple resections of giant cell tumor - thought to be due to older techniques
- No evidence that fracture will increase rate of transformation of mets
-
primary malignant giant cell tumor

Diagnosis? Common Presentation? Work-up?

Giant Cell Tumour
-
Presentation
- pain referable to involved joint
- palpable mass
- decreased range of motion around affected joint
- May present as pathological fracture
-
Radiographs
- eccentric, lytic
- epiphyseal/metaphyseal lesion that often extends into the distal epiphysis and borders subchondral bone
- expansile, formation of neocortex
- may have associated soft tissue mass
- knee, distal radius, sacrum, vertebral body, hand, can also see in proximal femur
-
Bone scan is very hot
- GCT are very vascular tumour
-
MRI
- shows clear demarcation on T1 image between fatty marrow and tumor
- In some cases they can be quite aggressive with associated cortical destruction and soft tissue mass
- In very advanced tumors they can expand into the cartilage of the joint
-
Histology
- neoplastic cell is the mononucleur stromal cell
- hallmark - giant cells are numerous
- secondary aneurysmal bone cyst degeneration is not uncommon
- Often have more nuclei than other tumors that contain giant cells (>50)
- Mesenchymal tumour - produces Type 1 and type 2 collagen
- VEGF (vascular endothelial growth factor) and MMP (matrix metaloprotein) are associate with metastasis

Diagnosis? Treatment/Management?

Giant cell tumor
-
Differential for epiphyseal lesions
- GCT, ABC, TOS
- Chondroblastoma
- Interosseous ganglia
- Clear cell chondrosarcoma
- If the diagnosis is clear from the XR, you can go ahead with treatment - confirm with MSK radiologist and ortho oncologist first
-
Staging (if you need to stage)
- Full imaging of bone
- Bone scan to rule out other lesions
- MRI to assess local staging
- CXR - 2% mets to lungs
- Biopsy after staging if concerns
-
Radiation alone
- only indicated for inoperable or multiply recurrent lesions
- leads to 15% malignant transformation
-
Medical management
- medical therapy can be used to augment or replace surgical management depending on the specific clinical senario
-
bisphosphonates
- osteclast inhibitors which may decrease the size of the defect in giant cell tumors
-
denosumab
- monoclonal antibody against RANK-ligand
- recent clinical trials suggest denosumab can decrease the size of the bone defect in giant cell tumor
- Interferon
- often used with mets
-
extensive curettage and reconstruction (with adjuvant treatment)
- challenge of treatment is to remove lesion while preserving joint and providing support to subchondral joint
-
Aggressive curettage
- extensive exterioration (removal of a large cortical window over the lesion) is required
- Need to be aggressive with burrs a
-
Adjuvant Treatment
- 10-30% recurrence with curettage alone verses 3% with adjuvant treatment
- hydrogen peroxide, argon beam, phenol
- Liquid nitrogen not used because it causes fracture
-
Augment
- can fill lesion with bone cement or autograft/allograft bone
- bone cement - cheap, structural, easy to see recurrence
-
Stabilization
- __locking plate
-
En bloc resection with structural allograft and endoprosthesis
- Recurrence
- Grade 3
- Expendable bone
- Clavicle, distal ulna, proximal and middle fibula
- Surgical excision of mets with treatment of interferon

Special considerations in GCT you should be aware of
-
hand lesion treatment is controversial
- if no cortical breakthrough treat with curettage and cementing
- if significant cortical breakthrough consider intercalary resection (with free fibular graft) vs. amputation
-
Sacrum
- Often hard to get access to, commonly abuts the SI joint
- Radiation can be considered
- Pre-op embolization can be beneficial in the spine to help control bleeding of these vascular tumors
-
Mets to lungs
- Elevation of c-myc oncogene
- Treat with surgical resection and interferon with good results

Enneking and capancci classificaiton of GCT
Enneking
- Benign, indolent, or biologically static
- Progressive growth, limited by natural barriers
- Locally aggressive with corre- sponding soft-tissue mass
Campanacci
- Radiographically well-circumscribed lucent lesion with no aggressive features (eg, periosteal reaction, soft-tissue mass, cortical breach). Rare.
- Relatively well-defined radiographic borders without a radiopaque rim
- Indistinct or ill-defined borders with radiographic demonstration of cortical bone destruction, and a soft-tissue mass

Differnetial? Diagnosis?

osteofibrous dysplasia
-
Differential
- OFD and AD
- fibrous dysplasia
- nonossifying fibroma
- unicameral bone cyst
- aneurysmal bone cyst
- chondromyxoid fibroma
- Langerhans cell histiocytosis (ie, eosinophilic granu- loma)
- osteomyelitis
- osteosarcoma
- chondrosarcoma
- hemangioendothelioma
- angiosarcoma
- metastatic carcinoma
Risk of mets in adamatinoma
25% overall
Classic AD (lower with OFD-like AD) Symptoms \< 1 yr Initial management of intralesional or marginal resection
Differential? Diagnosis? Management Plan?
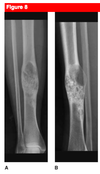
Adamantinoma
- 20-40 yo
- tibial lesion, similar in appearce to osteofibrous dysplasia
-
Presentation
- pain of months to years duration
-
Physical exam
- bowing deformity or a palpable mass of tibia is common
-
Radiographic characteristics
- multiple sharply circumscribed lucent lesions (“soap bubble” appearance) with interspersed sclerotic bone in mid tibia
- some lesions may destroy cortex
- may see bowing of the tibia
- unlike other primary bone tumors, adamantinoma typically shows no periosteal reaction
-
CT extremity and chest
- Can help determine the extent of cortical destruction
- rule out mets
-
MRI
- Important to determine the margins of the tumour and the soft tissue expansion to get tumour free margin
- Can help assess for multi-focal disease
-
Biopsy
- Important even for benign looking lesions
- Open biospy with adequate sample
- Can be very hetergeneous and is important to differentiate from osteofibrous dysplasia
-
wide-margin surgical resection
- often requires intercallary resection with allograft or intercallary megaprosthesis reconstruction
- as adamantinoma is a low-grade malignancy, radiotherapy and/or chemotherapy is not typically used for local control of disease
- Surgical resection of mets

Diagnosis? Management?
Adamantinoma
- full history and physical
- XR
- CT chest and lesion, MRI
- alway biopsy in 20-40 becasue AD can look like OFD
- This lesion was treated with wide resection and bone graft

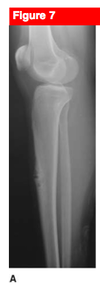
Diangosis? Management

Osteofibrous Dysplasia
- < 10 yo
- M>F
- tibia, confined to cortices
- usually regresses into childhood
-
Presentation
- may be asymptomatic
- painless swelling
- anterior or anterolateral bowing of the tibia
- pseudoarthrosis develops in 10-30% of patients
-
Radiographs
- anterior eccentric lytic tibial lesion in child that often leads to tibial bowing
- usually diaphyseal
- no periosteal reaction
- confined to anterior cortex
- looks very similar to adamantinoma
-
observation
- first line of treatment
- alone is the treatment for most patients
-
bracing
- if deformity significant and interfering with walking
- can help to minimize fracture
-
Casting pathological fracture
- __usually sufficient to heal fracture but will take longer
-
deformity correction with osteotomy
- indication
- rarely needed
- significant deformity
- perform after skeletal maturity
- indication
Diagnosis? Associated conditions and manifestations?

Fibrous Dysplasia
- A developmental abnormality caused by failure of the production of normal lamellar bone
- Fill in with a fibrous tissues, thought to be due to differntiation of cells
- females > males
- found in any and all ages
- onset for 75% of patients at <30 years of age
-
location
- the _proximal femu_r is most common site, followed by rib, maxilla, and tibia
-
Genetics
- GS alpha protein (chromosome 20q13) activating mutation (affects cAMP signaling pathway leading to increased production of cAMP)
- not inherited
- high production of FGF-23 which may lead to hypophosphatemia
-
Associated conditions
-
McCune Albright syndrome (30-50%)
- condition defined by the presence of (triad)
- skin abnormalities (cafe au lait spots in coast of Maine pattern - irregular borders)
- endocrine abnormalities (precocious puberty)
- renal phosphate wasing due to FGF-23 (oncogenic osteomalacia)
- Vaginal bleeding, faster growth, advanced tanner staging
- unilateral polyostotic fibrous dysplasia
- Risk of malignancy = 4%
-
Mazabraud syndrome
- polyostotic fibrous dysplasia
- soft-tissue intramuscular myxomas
- Slowly growing mass, usually present later
- No malignant transformation
-
Cherubism
- Symmetric invovlement of mandible and maxilla
- Can distort the orbits
- Becomes quiet when reaches skeletal maturtiy
-
Osteofibrous dysplasia
- rare form that primarily affects the tibia and is confined to the cortices
-
McCune Albright syndrome (30-50%)
-
nonorthopedic manifestations (more common with polyostotic)
- Hyperthyroidism
- Hypophosphatemia
- Acromegaly
- hyperprolactinemia
- Abnormalities of brain, heart, liver and spleen
- severe cranial deformities with blindness can occur
-
Prognosis
- 1% risk of malignant transformation to osteosarcoma, fibrosarcoma, or malignant fibrous histiocytoma
- Most common site is craniofacial bones
- poor prognosis
- 4% in Mcune albright
Syndromes associated with fibrous dysplasia
-
McCune Albright syndrome (30-50%)
- condition defined by the presence of (triad)
- skin abnormalities (cafe au lait spots in coast of Maine pattern - irregular borders)
-
endocrine abnormalities (precocious puberty)
- renal phosphate wasing due to FGF-23 (oncogenic osteomalacia)
- Vaginal bleeding, faster growth, advanced tanner staging
-
unilateral polyostotic fibrous dysplasia
- Risk of malignancy = 4%
- condition defined by the presence of (triad)
-
Mazabraud syndrome
- polyostotic fibrous dysplasia
- soft-tissue intramuscular myxomas
- Slowly growing mass, usually present later
- No malignant transformation
-
Cherubism
- Symmetric invovlement of mandible and maxilla
- Can distort the orbits
- Becomes quiet when reaches skeletal maturtiy
- Symmetric invovlement of mandible and maxilla
-
Osteofibrous dysplasia
- rare form that primarily affects the tibia and is confined to the cortices
Extraskeletal manifestations of fibrous dysplasia?
- Skin (with mcune albright)
- irregular cafe au lait spots
- Hyperthyroidism
- Hypophosphatemia
- Acromegaly
- hyperprolactinemia
- precocious puberty
- Abnormalities of brain, heart, liver and spleen
- severe cranial deformities with blindness can occur
25yo female comes in with pain in her leg and progressive deformity. Diagnosis? Work-up?

Fibrous Dysplasia
-
Symptoms
- usually asymptomatic and discovered as an incidental finding
- may have swelling or deformity
- bone lesions may be monostotic (80%) or polystotic (20%)
- pain from stress fractures
- Complete medical history to rule out associated endocrine anomalies
-
Physical exam
- inspection
- cafe au lait spots, skin hyperpigmentation
- larger and more irregular borders than neurofibromatosis
- swelling around lesion (prominent jaw, rib mass, bossing of the skull)
- cafe au lait spots, skin hyperpigmentation
- Can get bowing of affected bones due to microfracture and remodelling
- Look for signs of precocious puberty
- inspection
-
Screening blood work with referal to pediatrician for full endocrine work-up
-
ALP, urine hydroxyproline
- Usually elevated with active disease
- Can be used to follow response to treatment
- TSH, Ca, Phos
- Testosterone, estrogen, estradiol
-
ALP, urine hydroxyproline
-
Radiographs
- central lytic lesions in medullary canal (diaphysis or metaphysis)
- may have cortical thinning with expansile lesion
- highly lytic lesions or a ground glass appearance
- “punched-out” lesion with well defined margin of sclerotic bone is common
- modest expansion of bone
- Shepherd’s crook deformity
- vertebral collapse and kyphoscoliosis
- Evidence of malignant transformation
- Lytic lesion where previously sclerotic
- Periosteal reaction
- Cortical disruption
- Soft tissue mass
-
Bone scan
- usually warm, cold does not rule lesion out
- Helpful to identify polyostotic lesions
-
CT
- Can help assess bone quality and extent of lesion
-
MRI
- Can help assess full lesion with cystic degeneration
- Help stage the soft tissue lesion following malignant degen
-
Histology
- alphabet soup
- Trabeculae not lined with osteoblasts
15yo male. Fall from height and unable to WB on right side. Diagnosis? Treatment?

Fibrous Dysplasia
-
Work-up
- ALP, hydroxyproline urine
- TSH, Ca, Phos
- Testosterone, estrogen, estrodiol if concerned
- Full length XR
- Bone Scan - assess for other lesions
- CT/MRI
-
observation
- asymptomatic patients
-
Diphosphonate therapy
- symptomatic polyostotic fibrous dysplasia
- effective in decreasing pain and reducing bone turnover
- Evidence of:
- Cortical thickening
- Decreased pain
- Progressive ossification
- Prevent pathological fracture
- Decrease N-telopeptide
- Decrease size of the lesion
-
Ca and Vitamin D
- Can help prevent secondary hyperparathyroidsim
-
internal fixation and bone grafting
- indications
- symptomatic lesions
- impending/actual fractures through lesions in areas of high stress (femoral neck)
- severe deformity
- neurologic compromise in the spine
- Nonunion
- malignancy
-
technique
- never use autogenous cancellous bone, as the transplanted bone will quickly turn into fibrous dysplastic woven bone
- use cortical allografts
- intramedullary device more effective than a plate in the lower extremity
- Then can currette the lesion if accessible
- never use autogenous cancellous bone, as the transplanted bone will quickly turn into fibrous dysplastic woven bone
- indications
-
Pathological fracture
- Casting
- Microfracture/pathological fracture needs to be treated first with cast immobilizaition in the upper extremity
- Proximal femur fractures
- Treat with IM Nail
- IV bisphosphanates
- Casting
-
osteotomies
- Valgus osteotomy - coxa valga
- Helps to reduce risk of pathological fracture
- Medializing osteotomy - shepard’s crook
- Valgus osteotomy - coxa valga
-
Outcomes
- Upper extremity does well with operative or non-operative treatment
- Lower extremity more often requires internal fixation
- <18 have worse outcomes due to recurrent pathological fractures
Indications to operate on fibrous dysplasia
- symptomatic lesions
- impending/actual fractures through lesions in areas of high stress (femoral neck)
- severe deformity
- neurologic compromise in the spine
- Nonunion
- malignancy
Manifestations of Pagets
-
Orthopedic
- long bone bowing and bone pain
- fractures
- large joint osteoarthritis (medial OA with protrusio)
- Spinal cord compression
- high output cardiac failure
-
Other
- Hearing loss
- Warmth over affected area
- Vertigo
- Cranial nerve palsies
- Paget’s sarcoma
- less than 1% will develop malignant Paget’s sarcoma (secondary sarcoma)
- osteosarcoma is the most common, followed by fibrosarcoma and chondrosarcoma
- most common in pelvis, femur, and humerus
- Paget’s sarcoma has a poor prognosis
- 5-year survival for non-metastatic Paget’s sarcoma is less than 5%
- appropriate treatment for Paget’s sarcoma includes chemotherapy and wide surgical resection
Stages of Pagets
- (1) an initial, short-lived burst of multinucleate osteoclastic activity, causing bone resorption
- Get increased ALP
- (2) a mixed phase of both osteoclastic and osteoblastic activity, with increased levels of bone turnover leading to deposition of structurally abnormal bone
- (3) a final chronic sclerotic phase, during which bone formation outweighs bone resorption
Work-up for Pagets
-
Labs
-
ESR, CRP
- If elevated may be due to malignant transformation
- elevated serum alkaline phosphatase, urinary hydroxyproline (collagen breakdown marker)
- Can be used to monitor response to therapy
- increased urinary N-telopeptide, alpha-C-telopeptide, and deoxypyridinoline
-
normal calcium levels and Vit D
- Should be used to screen for other metabolic disease
-
ESR, CRP
- Radiographs
- coarsened trabeculae which give the bone a blastic appearance
- both increased and decreased osteodensity may exist depending on phase of disease
- lytic phase
- lucent areas with expansion and thinned, intact cortices
- ‘blade of grass’ or ‘flame-shaped’ lucent advancing edge
- mixed phase
- combination of lysis and sclerosis with coarsened trabeculae
- sclerotic phase
- bone enlargement with cortical thickening, sclerotic and lucent areas
- remodeled cortices
- loss of distinction between cortices and medullary cavity
- long bone bowing
- bowing of femur or tibia
- fractures
- commonly femoral neck
- hip and knee osteoarthritis
-
osteitis circumscripta
- (cotton wool exudates) in skull
-
Arthritis associated with pagets
- Medial OA (as opposed to superior)
- Coxa vara
- protrusio
-
Paget’s secondary sarcoma
- shows cortical bone destruction
- soft tissue mass
-
MRI
- may show lumbar spinal stenosis
- Would show a mix of fat and tumour in the marrow in the lytic phase
- Will enhance with gadollinium
-
Bone scan
- accurately marks site of disease
- intensely hot in lytic and mixed phase
- less hot in sclerotic phase
-
CT Scan
- cortical thickening and coarsened trabeculae
Medical Treatment of Pagets
-
bisphosphonates
- oral agents
- alendronate and risedronate
- etidronate disodium (Didronel)
- older generation medication
- inhibits osteoclasts and osteoblasts
- cannot be used for more than 6 months at a time
- intravenous agents
- pamidronate, zoledronic acid (Zometa)
- newer generation medications that only inhibit osteoclasts
- disadvantageous in that they only come in IV form
- oral agents
-
calcitonin
- causes osteoclasts to shrink in size and decreases their bone resorptive activity within minutes
- administered subcutaneously or intramuscularly
-
teriparatide
- is contraindicated in Paget’s disease due to risk of secondary osteosarcoma
Approach to THA in this patient?

Pagets
-
Indications
- affected patients with degenerative joint disease
-
technique
- treat Paget’s with pharmacologic agents prior to arthroplasty to reduce excessive bleeding
- Ok to do cementless
- Malignment leads to early loosening
- May need osteotomy
- May need to burr out the canal (better than a rasp or reamer)
- Component positioning
- Protrusio, sclerosis
- May need TM cup or antiprotrusio cage
- Lateralizing liner
-
outcomes
- greater incidence of suboptimal alignment secondary to pagetoid bone
-
Complications
- HO - consider radiation
- Blood loss
- Non-union of osteotomy
- Periprosthetic fracture
- Loosening
contraindications to limb salvage surgery
- Major neurovascular structures encased by tumor when vascular bypass is not feasible
- Pathologic fracture with hematoma violating compartment boundary
- Inappropriately performed biopsy or biopsy-site complications
- Severe infection in the surgical field
- Immature skeletal age with predicted leg-length discrepancy >8 cm
- Extensive muscle or soft-tissue involvement
- Poor response to preoperative chemotherapy
Enneking staging system
-
IA
- Low Grade
- T1 - intracompartmental
-
IB
- Low Grade
- T2 - extracompartmental
-
IIA
- High Grade
- T1 - intracompartmental
-
IIB
- High Grade
- T2 - extracompartmental
-
III
- Metastatic
- T1 - intracompartmental
- M1 (regional or distant)
-
III
- Metastatic
- T2 - extracompartmental
- M1 (regional or distant)
Diagnosis? Genetics? Characteristics?

Osteosarcoma
-
Bimodal
- second decade
- later - pagets, radiation
- knee > proximal femur, humerus, pelvis
-
Usually presents as IIB
- 20% have pulmonary mets
-
Associated with retinoblastoma gene (Rb) and p53
- Le-Fremeni Syndrome
- risk increased in Rothmund Thomson syndrome
Prognostic factors of osteosarcoma
- advanced stage of disease (most predictive of survival)
- < 90% necrosis after chemo
- tumor site and size
- expression of P-glycoprotein
- high serum alkaline phosphatase
- high lactic dehydrogenase
- vascular involvement
- surgical margins
- type of chemotherapy regimen
- Skip mets
- Lymph node invovlement
Comes in with pain, fever, chills, night sweats. Diagnosis? Work-up?
- Blood work
- ESR, CRP, ALP, LDH
- Full length XR
- blastic destructive lesion
- sunburst, hair on end, codmans triangle
- calcification/osteoid
- large soft tissue mass
- MRI lesion
- Bone Scan - skip lesions, distant bony mets
- CT chest - more sensitive than CXR for pulmonary mets
- Biosy
- lacey osteoid, high grade mitotic figures and malgnant features