Lower GI Tract Flashcards
(29 cards)
LO:
- Organs of the gastrointestinal tract: Summarise the structure of gastrointestinal organs and relate these to their functions
- Intestinal disorders: Summarise the pathology and pathophysiology of small and large intestine disorders
- Intestinal disorders: Describe the clinical features and treatment options of small and large intestine disorders
Session Plan
Learning Aims
1) Recap on basic anatomy and function
2) An overview of LGI tract disorders
3) A focus on Inflammatory Bowel disease
i. Incidence and presentation
ii. Types
iii. Aetiology
iv. Management
4) Conclusion and take home messages

Lower GI Tract disorders-recap on basic anatomy

Large bowel-In reverse anus and rectum, sigmoid is s shaped, then descending colon, transverse colon, ascending colon, then caecum
caecum-where you also find appendix
Ileocaecal valve-gives access to small bowel
Blood supply-Small intestine-supplied by SMA
Colon is supplied by branches of SMA and IMA
IMA covers mainly left side of colon
Venous uptake from bowel is through the SMV and the IMV that join to form the portal vein and eventually join the inferior vena cava.
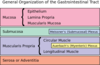
Wall structure of colon-4 layers-first is mucosa (composed of 3 layers itself)-has lots of glands that produce mucin to lubricate bowel and make passage of stools easier, thickened layer is submucosa, then have muscularis layer (circular and longitudinal muscles), then serosa which is like a duvet over other layers and it contains the main vessels and the nerve supply.
Nerve supply comes from centrally but also remember in the bowel we have submucosal and myenteric plexuses which act as localised pace makers for the bowel. These are usually between the muscularis and submucosa layer.
Yellow bits are nerve supplied layered between submucosa and muscularis
Serosa is covered by visceral peritoneum

Recap on basic anatomy and function:
Parasympathetic and sympathetic supply
Centrally and locally!
- Parasympathetic: ascending colon and most of transverse colon innervated by vagus nerve.
- Whereas more distal innervated by pelvic nerves.
- Sympathetic- lower thoracic and upper lumbar spinal cord.
- External anal sphincter controlled by somatic motor fibres in the pudendal nerves.(s2, s3, s4)
Recap on basic anatomy and function:
sensory and other nervous supply
- In addition have afferent sensory neurons detect pressure. Very important in rectum as they send signals for emptying process of rectum.
- Enteric nervous system also important- Hirschsprung’s disease (no enteric intramural ganglia).
Hirschsprung disease is characterized by congenital aganglionosis of the distal bowel. The aganglionosis always involves the anus and extends proximally for a variable distance. Both the myenteric (Auerbach) plexus and submucosal (Meissner) plexus are absent, resulting in poor bowel motility and function.
•Myenteric plexus ganglia concentrated below taenia coli
An overview of disorders
LGI tract disorders can be divided into:
1. Inflammatory
- Inflammatory Bowel Disease (IBD)
- Microscopic colitis-inflammation of bowel as well but characterised by normal looking mucosa when seen in colonoscopy, but when take biopsy can see collagenous changes and lymphocytes.
2. Infective
- C Diff
- E Coli .. etc
3. Structural
- Diverticular disease
- Haemorrhoids
- Fissures
4. Functional
- Irritable bowel syndrome-common and characterised by normal investigations and GI tract but lots of symptoms like pain, bloating and even diarrhoea.
5. Neoplastic
- Colonic polyps & colon cancer
6. Other
- Neurological, metabolic & vascular.

Inflammatory Bowel Disease
- Very common and serious condition. Affects 1.5 million people in America and 2.2 million in Europe
- Several hundred thousand more worldwide
- Lifelong chronic disease, often affecting young people
- Major toll
- Burden of therapy for patients
- Hospitalisation
- Surgery
- Health-related quality of life
- Economic productivity
- Social functioning
Becoming more common to detect IBD. Common age of detection is in 2 peaks age: 20-30 and 50-60
Chronic condition which waxes and wanes, no cure so burden of therapy is high
Particularly high incidence in Northern hemisphere. Originally thoughout it was a more european disorder but even asia and middle east have shown an increase so may be due to increase in migration and mixing of genetic pool. Places like australia have significantly higher numbers, but may be due to european gene pool that compromises this country.

Inflammatory Bowel Disease-types
UC-mainly affects superficial layer of mucosa
Continuous inflammation
Inflammation from rectum to descending or sigmoid or further up
UC and CD are not related, they are separate
CD
Granulatomous inflammation is a sign of Crohns ie macrophage aggregation
Can affect any part of gi tract, can be patchy in nature, anywhere from anus to mouth. Doesn’t just affect mucosa but can affect deeper so can form fistulas (deep penetration from one wall to another eg inflammation in wall of colon can extend deeply to small bowel-penetration between those two walls causing interaction between these areas) and strictures (narrowing of lumen due to swelling and inflammation, can get fibrosis tissue after which doesn’t open up again)
Much deeper inflammation
Patchy granulatomous inflammation which can change

Inflammatory Bowel Disease-types of Ulcerative colitis and types of Crohn’s disease:
UC-always involves rectum, when only affect rectum=proctitis
Can see it is always a continuous pattern, no gaps
If more extensive and entire colon involved=pancolitis
CD-can involve different segments, patchy inflammation
Random: Hallmark of crohn’s disease is deep ulceration and because it is deeper into mucosa it can cause strictures and fistulas.

IBD-Symptoms depend on site of inflammation:
Colitis-inflammation of mucosa of the bowel
- Bleeding
- Mucus
- Urgency-hallmark of a lower rectal disorder due to sensory changes there
- Diarrhoea
Perianal-penetrating severe structures (remember UC is rectum so colon, so anus not affected)
- Anal pain
- Leakage
- Difficulty passing stool due to pain
CD it can be painful as deeper ulcers but UC generally isn’t very painful. Perianal symptoms is a hallmark of crohn’s disease. So often perianal fistulas etc.
Small bowel disease
- Abdominal pain- as usually Crohn’s disease and it’s ulceration
- Weight loss-as poor absorption, occurs in small bowel
- Tiredness/lethargy-tend to become anaemic (ulcers can bleed and lack of iron and B12 absorption) and other mineral absorption
- Diarrhoea
- Abdominal mass
UC-only affects large lowel so doesn’t tend to cause malnutrition like crohns does

IBD-Extra-intestinal manifestations:
As autoimmune condition, it can have effects outside GI tract. Immune reaction can present on other organs eg
Arthritis-affects joints
- Axial – Ankylosing Spondylitis
- Peripheral
Skin
- Erythema nodosum (see leg pic-rash)
- Pyoderma gangrenosum (severe form of rash shown on top)
Eyes
- Anterior uveitis (eye pic seen on bottom)
- Episcleritis/Iritis
Liver
- Primary Sclerosing Cholangitis (PSC)-in 80% of UC ie more commonly seen in people with UC
- Autoimmune hepatitis

Inflammatory Bowel Disease - Aetiology
Still don’t now what causes IBD. But research is coming closer to understanding it.
Impaired mucosal immune response
Genetically susceptible people respnd inappropriately to gut microbiota. We think there is an imbalance between healthy microbiota and the pathological microbiota and the immune system reacts inappropriately to this imbalance and causes inflammation at the level of the mucosa and therefore effects the bowel mucosa.
Multiple environmental factors and luminal microbes eg mycobacterium species have been linked to patients with IBD
The immune response will have autoantibodies such as PANCHA in UC
In genome wide association studies, so when looking at genetics of millions and millions of people, we noticed that certain genes are very prevelant in IBD patients. Especially NOD2 on 2nd chromosome which is associated with Crohn’s disease. (Remember NOD2 as IBD can cause erythema NODosum!). More than 30 genes now that are associated with IBD. All are associated but don’t know how they contribute but we know in these patients their reactions to the microbiota activates the immune system and causes the inflammation.

Inflammatory Bowel Disease - Aetiology
-Poor diet eg high sugar and takeaways and imbalanced diet resulting in change in microbiota different to healthy patient and ths together with genes cause dysbiosis which means unhealthy gut microbiota.
In pic-see physically active people have less IBD, people without appendix (appendicectomy) are protected from UC but they can get Crohns as appendix acts as reservoir for microbiota and it might be linked to the activation of the immune system
Smoking- we think nicotine changes permeability of mucosa making it more susceptible, so makes Crohns more severe and means it is diagnosed at earlier ages. Smoking is protective for UC as people who stopped smoking developed UC later.
Protected and high hygeine areas tend to develop IBD.
Poor microbiota triggers immune inflammation

Inflammatory Bowel Disease - Management
Main goals:
Goals
- Induce clinical remission
- Maintain clinical remission
- Improve patient quality of life
AND
- Heal mucosa so doesn’t stricture
- Decrease hospitalisation/ surgery & overall cost
- Minimise disease and therapy related complications

Inflammatory Bowel Disease - Management
- Steroids
- 5 ASA (Aminosalicylates)
- Immune suppressants eg.
- Azathioprine
- Methotreaxate
- Biologic therapy-targets anti-TNF TNF is main driver of immune reaction
- Others –diet, FMT, antibiotics, probiotics, novel agents
Inflammatory Bowel Disease - Management with steroids
Diffuse and bind in nucleus to Glucocorticoid Responsive Elements (GRE).
- GRE interact with specific DNA sequences
- Increase anti-inflammatory gene products
- Block pro-inflammatory genes
Mode of Delivery:
•IV, Orally or rectal enemas
Use:
- Short term or only to induce healing in an acute setting as we know steroids stop working in the long term and also have significant side effects in long term use.
- As a bridge to other therapy/interventions
- In acutely unwell patients

Steroids-adverse effects:
In long term-ie 6-8 weeks+

Inflammatory Bowel Disease - Management-5 ASA
(not as useful as biologics and immunosuppressant drugs)
- Inhibition of pro-inflammatory cytokines (IL-1 and TNF-a )
- Inhibition of the lipo-oxygenase pathway i.e. prostaglandin and leukotrienes
- Scavenging of free radicals
- Inhibition of NF-kB/ TLR via PPAR-gamma induction (perioxisome proliferator activated receptor-gamma)

5 ASA also has
- Some immunosuppresive activity – inhibiting T cell proliferation, activation and differentiation
- Impairs neutrophil chemotaxis and activation
- Mode of Delivery:
Orally or rectal
Note: it’s a first line treatment for UC but only really used for mild crohns (less often used)

5 ASA - side effects:
- Intolerance
- Diarrhoea
- Renal impairment
- Headache
- Malaise
- Pancreatitis
- Pneumonitis
Inflammatory Bowel Disease - Management-Immunomodulator eg Azathioprine:
- 6-TG interferes with adenine and guanine ribonucleotide production.
- Results in reduced number of B and T lymphocytes, immunoglobulins and interleukins. So basically suppresses the immune reaction and therefore reduces inflammation that way.
- Another pathway potentially results in apoptosis of T cells
Azathioprine is a precursor of Mercaptopurine (6-MP), which with these enzymes, TPMT and HPRT, changes to 6-MMP and 6-TIMP (remember the enzymes as tent and hert and then replace e with p!). And finally 6-TIMP changes to 6-TGN. And 6-TGN intervenes with adenine and guanine so affects DNA function and production.
Need to remember these pathways as we always check TPMT in patients as if TPMT enzyme in low in patients, then we have to reduce the dose of 6-MP, because otherwise there would be very high dose of 6-GTN and the side effects can increase then.
Low TPMT is just caused by genetics, some people genetically have less than others.
So with Azathioprine, if you have low TMPT, then all the azathioprine will take the pathway on the right ie into 6-TGN, so it won’t go half half. So if you do that, the 6-TGN will be very high and so will have many side effects. Therefore you need to reduce the Azathioprine dose if you have low TMPT, as only a little bit of aza is needed to go down the pathway on the right.

Azathioprine side effects
Check…
Skin cancers such as BCC Basal cell carcinoma and SCC Squamous Cell Carcinoma
Check Hep b/c as they are immunosuppressed so could reactivate. As with other disorders that could be reactivated.
Measure TPNT is that if it is low, then all the 6-MP will go to 6-TMP

Inflammatory Bowel Disease - Management-Methotrexate
- Mechanism not clear
- Interferes with DNA synthesis & cell reproduction
- Increased adenosine levels (anti-inflammatory)
- Increased apoptosis of peripheral T cells
- Takes 3 months to work
- Need history re liver abnormalities
- Monitor LFTs, FBC
- Advise NO pregnancy
- Folic acid supplements (reduces side effects)
- WEEKLY DOS

Methotrexate – side effects
- Rash
- Nausea, mucositis, Diarrohea
- Bone marrow suppression
- Hypersensitivity pneumonitis
- ↑’ed liver enzymes
- Hepatic fibrosis/cirrhosis
- Known abortifacient
- No documented ↑ed risk of lymphoma or skin cancer








