Gastointestinal Infections and Disorders Flashcards
(15 cards)
LO:
- Intestinal disorders: Summarise the pathology and pathophysiology of small and large intestine disorders
- Intestinal disorders: Describe the clinical features and treatment options of small and large intestine disorders
GI Disorders & Infections – Case 1
Stroke in 2003
Apixaban-anticoagulant
Ramipril-for BP
Nitrofurantonin for recurrent UTIs

Temp of 37.6 so mildly up
On coamoxiclav for 4 days after op
white cells are elevated, Hb normals
Creatinine high (renal dysfunction)
Coagulation screen in normal
Albumin low at 16
CRP is inflammatory marker and has gone up
Skin turgor is a sign of dehydration

Case 1 Differential Diagnoses:
-Creatinine, skin turgor and dry mucous membrane suggest AKI indicating dehydration.
Think of infectious and non-infectious causes when see diarrhoea.
Infectious diarrhoea includes C.difficile because of her history of antibiotics. May be salmonella or ecoli though.
Usually IBS after an infection happens weeks later but this is quite acute in nature. Same with IBD it creeps up slowly and this is acute.
As dehydrated and low BP she coudl present with ischaemic colitis but this tends to come with a lot of bleeding and more abnormal blood tests
Coeliac disease since this is diarrhoea but unlikely as this wouldn’t come on acutely.

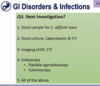
Next investigation to do:
=Stool sample for C.difficile toxin and stool culture because of the acuity of the onset.
Can see small bowel shadows which are normal in nature and so this is a normal abdominal X-ray.
Most important is C.diff then stool sample, then abdominal x-ray, then endoscopy

Case 1-Management
Discontinue antibiotic associated with causing C.difficile
If you have the severe c difficile but also have hypotension or shock and dilated toxic megacolon=fulminant colitis

Oral-better absorbed and directly goes and attacks bacteria better than IV. As C difficile is in intestine so oral goes straight to the right place to target it.
FMT from healthy people is almost 98% effective in treating C.difficile.
If have really bad diarrhoea, need to be looked after in high dependency unit as losing lots of fluids and electrolytes.
Ileus is the medical term for this lack of movement somewhere in the intestines that leads to a buildup and potential blockage of food material.

HR has gone up from 89, her BP has dropped further and her temp is up. So she is getting worse despite being on antibiotics.
WCC higher, creatinine has almost doubled and CRP has skyrocketed

Bowel is significantly dilated compared to last X-ray and her blood pressure is worse so more likely to be fulminant colitis.
CXR shows bowel loops are so dilated they are creepy up to the level of the diaphragm.
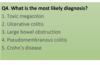
What is the most likely diagnosis?-toxic megacolon, small or large bowel obstruction or ileus
(ileus is spasming of the bowel)
=TOXIC MEGACOLON
Not small bowel obstruction as here can see large bowel dilated. Sepsis in general could cause ileus and spasming in the bowel, but with this her having c diff and her crp and white cells up indicate toxic megacolon.

1st line treatment:
-medications to increase BP to perfuse her kidneys and make them work
HR and BP normalised
Tend to give patients 4-6 weeks of vancomycin to fully get rid of C.difficile

Indications for surgery:
Some patients perforate because of toxic megacolon and don’t respond to aggressive medical treatments.
So if don’t respond to therapy or have complications, then surgery is needed.
Pseudomembranous colitis is what we see when we do colonoscopy associated with C.difficile. Classical feature on histology when we biopsy.

GI Disorders & Infections – Case 2
Tenesmus-feeling of incompleteness of passing bowel movement

Blue=abnormal
WCC and platelets and CRP-bit elevated
Kidney function which is urea and creatinine is normal

Case 2: Differential Diagnoses
Long history-so not acute, has been going on for a while.
Platelets can be an inflammatory and infectious marker
Shigella, clostridium and ecoli can present with bloody diarrhoea.
Haemorrhoids tends to be just bleeding but no diarrhoea
Microscopic colitis-don’t see inflammation when examine, don’t tend to see PR bleeding
Ischaemic colitis is unlikely as she is young and otherwise healthy
Coeliac disease can cause diarrhoea, but again PR bleeding is unlikely
So thinking IBD or infectious cause

Calprotectin is an inflammatory marker in bowel
Stool culture and calprotectin (specific for bowel inflammation) to find out if infectious cause. Other infections probably more important that C.difficile in this case so test for them first. (c diff is more common if on antibiotics or immunodeficient so less likely, but if get negative for other cultures then would do this).
Would probably do endoscopy before imaging in this case as she is young and don’t want to put her through radiation

=UC
as continuous inflammation and lack of granulomas
Management options and UC severity
She has mild ulcerative colitis

As suppository, as on left side, but presented with worsening symptoms so we should escalate therapy

-Look at WCC and CRP to check severity
Remember steroids work well acutely but not long term
Think of next step after 5-ASA so immuno-modulators (check vaccinations as they suppress immune system)

She has gone from mild to moderate to severe so we need to escalate therapy again.

As she was on Azathioprine which reduces immunity, need to check for infections and C difficile.
Need to do a CT to check for perforations etc.
Infliximab=TNF-alpha blocker medication used in severe IBD
Pic shows side effects of anti-TNF therapy. We know there is synergistic effect so maintain on azathioprine as this enhances the action of Infliximab so gave combination therapy.



