Lecture 4: Biliary Secretion: Hepatobiliary function Flashcards
(55 cards)
How can liver failure lead to edema?
Results in hypoalbuminemia, which throws the Starling forces out of wack
What is Cirrhosis of the liver and how does excessive alcohol intake contribute?
- Chronic liver disease in which normal liver cells are damaged and replaced by scar tissue
- Alcohol abuse leads to accumulation of fat within hepatocytes. Fatty liver leads to steatohepatitis, which is fatty liver accompanied by inflammation, which leads to scarring of liver and cirrhosis
What are changes to venous circulation associated with portal HTN?
- Esophageal varices: swollen connection between system and portal system at inferior end of esophagus
- Caput medusae: swollen connections between systemic and portal system around umbilicus
How can liver dysfunction lead to hepatic encephalopathy?
- Decreased hepatic urea cycle metabolism leads to the accumulation of ammoinia in portal circulation
- Ammonia readily crosses the blood-brain barrier and alters brain function
Where is bile produced and secreted from?
Liver
What is the composition of bile?
- Bile salts (50%)
- Bile pigments (2%) i.e., bilirubin
- Cholestrol (4%)
- Phospholipids (40%): i.e., lecithin
- Ions
- H2O
Where are primary bile acids, secondary bile acids, and bile salts made
Primary = hepatocytes of liver
Secondary = lumen of small intestine
Bile salts = conjugated in the liver

What is the relative amounts of the 4 bile acids from greatest to least?
Cholic acid > chenodeoxycholic acid > deoxycholic acid > lithocholic acid
What do bile salts do w/ the products of lipid digestion?
Form micelles

What are the key players of the biliary system that result in bile secretion?
- Liver
- Gallbladder and bile duct
- Duodenum
- Ileum
- Portal circulation

What is the 3 major steps for bile secretion?
- Bile is synthesized and secreted by the liver to the gallbladder
- Gallbladder stores bile salts and concentrates them through the absorption of ions and H2O, secretin causes an increase of ions and H2O in the bile duct
- CCK induces the gallbladder to contract and the sphincter of Oddi to relax allowing bile to flow into the duodenum

What occurs once bile is secreted into the duodenum until its return to to the liver?
- Bile emulsifies and digests fats in the duodenum
- Micelles are formed and fat is absorbed in the jejunum
- Ileum actively absorbs any unused bile back into portal circulation
- Bile salts are then returned to the liver

What happens to bile at the canalicular membrane?
- Together w/ newly synthesized bile salts, the retuning bile salts are secreted into the bile canalicul
- Canalicular bile is secreted by ductule cells in response to the osmotic effects of anion transport
How are bile salts returned to the liver and what occurs here?
1) Transported from the ileum to the portal blood (enterohepatic circulation) and back to the liver
2) Synthesis of bile salts occurs to replace the amount that was lost

Uptake of bile across the basolateral membrane of the hepatocytes is mediated by what two systems?
1) Na+ dependent transport protein, sodium taurocholate cotransporting polypeptide (NTCP)
2) Na+-independent transport protein, organic anion transport proteins (OATPs)

How is bile transported into the hepatocyte and then into the bile canaliculi, which transporters are involved?
- From portal circulation enters hepatocyte via NTCP (Na+-dependent) or OATP (Na+-independent)
- Inside hepatocyte the bile can leave via BSEP (bile salt excretory pump) or MRP2 (multidrug resistance protein 2), both of which are ATP-dependent

What transporters are used to get bile from the lumen of the SI into the enterocyte and then back into portal circulation?
- Enters the enterocyte via ASBT (apical sodium dependent bile acid transporter)
- Once inside the enterocyte it can leave back into portal circulation via the OSTα-OSTβ (organic solute transporter alpha-beta)

How efficient is the ileal transport of bile acids to the portal blood; is there any transport in the jejunum?
- Highly efficient as more than 90% of the bile acids are returned to portal blood via active and passive transport
- Some passive transport of mostly unconjugated bile happens in the jejunum, and only about 3-5% of bile is lost in the feces

What will occur to the de novo synthesis and secretion of bile in the case of an ileal resection; how large will this change be?
- Recycling of bile will be much less efficient so you will see a large increase in the de novo synthesis of bile
- You will likely see a decrease in bile secretion
- Values >10-fold higher than normal
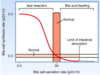
What will occur if we add bile acids to the system, such as a bile acid feeding?
The synthesis of bile will decrease, because the system has more than enough and will only make as much as it needs

With increased bile secretion, the rate of return of bile to the liver will also likely be increased, what effect does this have on the synthesis of bile, specifically on what enzyme?
- Negative feedback on the synthesis
- Cholesterol 7α-hydroxylase will be inhibited by bile salts
What are the 2 mechanisms for bile secretion; what is the main stimuli?
1) Allmost all bile formation is driven by bile acids (bile acid-dependent)
2) Small portion of bile is stimulated by secretin and is secreted from the ducts (bile acid-independent or ductular secretion)
The secretion of bile acids is accompanied by the passive movement of?
Cations into the canaliculus

What effect does secretin have on bile?
Stimulates the secretion of HCO3 and H2O from the ductile cells, resulting in a significant increase in bile volume, [HCO3], and pH. Accompanied by a decrease in the concentration of bile salt











