Lecture 1: Liver Biochemistry Flashcards
(50 cards)
Liver recieves blood supply from 2 sources, what are they, and what is the major source?
1) 75% from portal vein
2) 25% from hepatic artery
List the important functions of the liver
1) CHO metabolis
2) Lipid metabolism
3) Nucleotide biosynthesis
4) AA metabolism, ammonia and urea cycle
5) Synthesis of blood proteins
6) Bilirubin metabolism
7) Waste management - inactivation and detox of metabolites and xenobiotics
What is the major role of the liver?
Monitoring, synthesizing, recycling, distributing, and modifying metabolites
What is unique about the circulation of the liver; why is it important?
- Liver receives blood from enteric circulation (via portal vein) and from periphery (via hepatic artery)
- Low portal blood pressure allows for hepatocytes and endothelial cells to have increased contact w/ the blood
What are some of the structural features of the liver that facilitate its function?
1) Low portal blood pressure
2) Lack of basement membrane and tight junctions
3) Gaps between endothelial cells
4) Fenestrations (pores) in endothelial cells
List the important functional characteristics of Hepatocytes?
- Well developed plasma membrane w/ endocytic and exocytic system
- Well developed ER (both rough and smooth)
- Metabolically very active
- Large # of endosomes, mitochondria, and lysosomes
What is needed to generate isopentenyl pyrophosphate (IPP)?
Three acetyl CoA molecules make a 5 carbon IPP
Why is IPP important?
Serves as a building block for the synthesis of all isoprenoids, including steroids, lipid soluble vitamins (ADEK), and prenyl groups that attach proteins to the plasma membrane

What are the sources of acetyl CoA; where is it generated?
- Generated in the mitochondria
- Oxidative decarboxylation of pyruvate
- Beta-oxidation of FA’s
- Catabolism of several AA’s
How is the acetyl CoA transported in the cytoplasm?
The Citrate Shuttle
How is a sterane made and its functional importance?
- 6 units of IPP form a tetracyclic (4-ring) sterane
- Backbone of most steroids

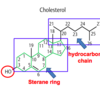
What is the structure of Cholesterol?
- Allicyclic compound made of 4 fused rings
- A sterane ring + hydrocaron chain
- One hydroxyl group at C3
Why is cholesterol important?
- Component of plasma membranes and precurso of biologically active compounds:
- Bile acids and bile salts
- Vit D
- Steroid hormones (progesterone, aldosteone, cortisol, testosterone…)
How is the biosynthesis of cholesterol related to dietary intake?
Biosynthesis is inversely proportional to dietary intake
What is the equation for the cholesterol synthesis pathway?
18 Acetyl CoA + 18 ATP + 16 NADPH + 16H+ + 4O2 —> Cholesterol + 16 NADP+ + 18 ADP + 18Pi
*Just focus on the fact that it takes a lot of energy to synthesize cholesterol
What is phase I of cholesterol synthesis (key steps and enzymes)?
- Acetyl Coa —> Acetoacetyl CoA
- Acetoacetyl CoA —(HMG CoA synthetase) –> HMG CoA
- HMG CoA —(HMG CoA reductase)–> Mevalonate
- Mevalonate —> IPP
What is the rate limiting enzyme of phase I of cholesterol synthesis; what are its activators and inhibitors?
- Hydroxymethylglutaryl CoA reductase
Activators: Insulin and Thyroxine
Inhibitors: Glucagon, sterols, high [AMP], Vit E, and statins
What are the rxns of Phase II of cholesterol synthesis?
- 6 IPP’s to Squalene to Lanosterol to Cholesterol
*Remember I-S-L-C (I Surely Love Cholesterol!)
What are Antimycotics (i.e., miconazole, ketoconazole) and why are they relevant to cholesterol synthesis
- Used to treat fungal infections (anti-fungals) by inhibiting formation of ergosterol (needed to maintain plasma membrane of fungal cells
- At high concentrations they block the enzymes that catalyze the rxn converting Lanosterol –> Cholesterol
What are some of the important side products generated during the synthesis of cholestrol?
- Prenylated proteins (i.e., Ras)
- Heme A
- Dolichol
- Ubiquinone (CoQ10)
What are statins and how do they work?
- Cholesterol lowering drugs
- Strong Competitive inhibitors of HMG CoA reductase
- Increase in SREBP maturation which leads to transcription of LDL receptor and subsequent ehanced clearance of cholesterol via LDL-receptor mediated endocytosis
What are some of the myotoxic side effects of statins?
Decreased formation of ubiquinon (CoQ10) and prenylated proteins
What is the fate of cholesterol once its made and what happens specifically in the liver?
- Packaged into VLDL and released into the blood (CP1)
- In liver: cholesterol used to synthesize bile acids
How is cholesterol synthesis regulated?
- Direct inhibition - by FFA’s, sterols, and statins
- Covalent modification - inactive in phosphorylated form, active in dephospho form. Mediated by energy status and hormones such as insulin, thyroxine, and glucagon
- Transcriptional control - binding of transcription factor to promoter (sterol response element (SRE)) on the gene alters mRNA level
- Translational control - protein synthesis level
- Post-translational control - protein turnover/degradation








