Lecture 1: Microbiology of the Cardiovascular System Flashcards
(100 cards)
What are 6 differential diagnoses for Myocarditis?
- Acute MI
- Acute and/or chronic HF
- Atypical chest pain
- Pericarditis
- Cardiomyopathies
- Valvular disease
During PE/ausculation of patient with myocarditis what are 3 possible findings?
- Soft S3/S4 (impaired ventricular function)
- New murmur (2’ to valvular insufficiency - variable)
- Pericardial friction rub (if extension into pericardium)
With myocarditis the signs and sx’s will be similar to CHF of which part of h cardiac cycle?
What signs/sx’s?
- Systolic CHF (decreased contractility)
- Orthopnea, dyspnea on exertions, crackles, paroxysmal noctural dyspnea
Upon extra-workup for myocarditis utilizing an EKG what are you assessing for and what are the most common findings?
Which rhythm is most common?
- A assess for arrhythmia (sinus TACHY most common)
- Transient ST-T wave
What are 5 workups that should be considered to aid in your diangosis of myocarditis?
- EKG
- CXR
- Echocardiogram
- PCR - detection of viral genome
- Labs
What would an echocardiogram help you assess in a patients with suspected myocarditis?
- Ventricular function and structure
- Evaluation of ejection fraction, LV size, and wall abnormalities
Which 5 lab values would be helpful in the diagnosis of myocarditis?
- CBC (possible leukocytosis)
- Cardiac enzymes (likely ↑ 2’ to myocyte damage)
- BNP (signs/sx’s of HF)
- CPK (assesing muscle damage)
- ESR and CRP
Which invasive diagnostic study may aid in the definitive diagnosis of Myocarditis?
Endomyocardial biopsy

What are 3 possible complications of myocarditis?
- Dilated cardiomyopathy
- Myopericarditis
- Sudden cardiac death (20%)
Which 3 drug classes are feasible options for treating myocarditis?
- Beta blockers
- ACE-I
- Diuretics
What are 3 things that need to be avoided or reduced in a patient with myocarditis?
- NSAIDs and Alcohol
- Exercise (restricted)
What are the 3 most common infectious etiologies of Myocarditis?
- Coxsackie B
- Trypanosoma cruzi
- Trichinella spiralis
Which viral family does Coxsackie B virus belong to and what is it’s morphology?
- Picornaviridae, Enterovirus
- (+) ssRNA virus, small, naked, icosahedral
When is the peak incidence of Coxsackie B virus and it’s mode of transmission?
- Summer and fall
- Fecal-oral transmission
What are 4 clinical manifestations caused by Coxsackie B virus?
- URI
- Pleurodynia (Devil’s grip - severe intercostal pain and fever)
- Myocarditis (most common infectious etiology)
- Aseptic meningitis
Which parasitic cause of Myocarditis is described as a hemoflagellate (intracellular protozoa)?
Trypansoma cruzi
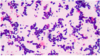
What are 2 diagnostic methods for Chagas disease (Trypanosoma cruzi)?
- Peripheral smear for trypomastigotes
- Xenodiagnosis

Signs/sx’s of acute phase Chagas Disease?
- Chagoma, Romana sign
- Fever, malaise, LAD
- CV: myocarditis
- CNS: severe meningoencephalitis (young pt’s)

What are the sign/sx’s of chronic Chagas Disease, both CV and GI?

- CV: dilated cardiomyopathy, arrhythmias
- Megalcolon and achalasia
What type of helminth is Trichinella spiralis**?
Invasive nematode

How is Trichinella spiralis transmitted?
Ingestions of cysts from raw pork (boars OR even horses)
Explain the life cyle of Trichinella spiralis upon ingestion of cysts, where do larvae mature and disseminate?
- Develop in gut –> mate –> larvae disseminate hematogenously
- Penetrate muscle tissue: skeletal, heart, and brain

What are the signs/sx’s Trichinella spiralis based on location in the body?
- Abdominal pain, diarrhea, fever (small intestines)
- Muscle aches (muscle invasion)
Periorbital edema, myositis, and eosinophilia should make you consider the diagnosis of which organism?
Trichinella spiralis