L11 Anticoagulant Drugs Flashcards
Learning Outcomes (for general perusal)
- List the different classes of anticoagulant drugs and their mode of action
- Contrast the pros and cons of using different anticoagulant drugs
- Compare the pharmacokinetic and dynamic properties of unfractionated and low molecular weight heparins and how these dictate their uses
- Discuss the endogenous and exogenous influences on warfarin’s effect and why this is important for a drug with a ‘narrow therapeutic window’
- Contrast the advantages and disadvantages of newly developed anticoagulant drugs over established anticoagulants
Overview (for general perusal)
- Haemostasis and Thrombosis
- Targets in the Coagulation Cascade
- Heparin
–Unfractionated (UFH)
–Low Molecular Weight (LMWH)
- Vitamin K antagonists - Warfarin
- New anticoagulants
What is Thrombosis?
This is the pathological formation of a ‘haemostatic’ plug within the vasculature in the absence of bleeding
What are the three components of Virchow’s Triad?
- Vessel wall injury
- Altered blood flow
- Abnormal Coagulability

- Describe an arterial thrombosis
- Describe a venous thrombosis
- Altered vessel wall rupture of plaque, Smooth muscle cell, foam cell, necrotic core, tissue factor, cholesterol, atherosclerotic plaque, platelet
- Necrosis. Stroke in the brain MI in the heart.
- Abnormal blood flow, increased coagulability, altered vessel wall.
- Venous system isnt bringing oxygen or nutrients but a Swollen limb can occur (usually in the leg)

What are the drug targets in fibrosis?
- Blood coagulation (fibrin formation) - Anticoagulants => this lecture deals with these
- Platelet Function (antiplatelet drugs)
- Enhance fibrin breakdown (fibrinolytic drugs)
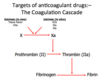
Where are the targets of the anticoagulant drugs?
The Coagulation Cascade
X to Xa (TF, VIIa - Extrinsic)(XIIa, XIa, IXa - Intrinsic)
Prothrombin (II) to Thrombin (IIa) (Xa)
Fibrinogen to Fibrin (Thrombin)
What are the anticoagulant drugs?
-
Heparin
- Unfractionated
- Low Molecular Weight
- Vitamin K Antagonists (Warfarin)
- New Drugs
Heparin - Overview
- What are they?
- Why was this fractionted into Low-Weight Molecular Heparin? (LMWH) 3-7 kDa
- Family of glycosaminoglycans of variable chain length (3-30 kDa), unfractionated heparin (UFH)
- these have longer duration and more predictable anticoagulant effect
2nd year medical student, 1916, extracted from a dog’s liver hence HEPARin (Greek)
Heparin
- What is it’s mode of action?
- What does LWMH have its main effect upon?

- Activates anti-thrombin III (ATIII) by binding to it. The Heparin-ATIII complex then inactivates thrombin (IIa) and Xa (UFH)
- LMWH not long enough to inactivate thrombin (IIa) therefore main effect is to inhibit Xa - still highly effective

Heparin - Pharmacokinetics
- What is their mode of administration?
- Why?
- When is it active when given IV?
- Given intravenously (UFH) or subcutaneously (UFH / LMWH)
- Large, highly charged molecules therefore cannot be absorbed by the GIT
- If intravenous then immediately active, T1/2 40-90 minutes, give bolus then infusion adjusted according to the activated partial thromboplastin time (APTT) aim for 1.5-2.5 x control
LMWHeparin - Pharmacokinetics
- How is it given?
- How often is it given?
- What is the dose adjusted by?
- What doesn’t it effect?
- What can be done to assess effect?
- How is it excreted?
- Subcutaneously
- Once/twice a day - longer half life
- Weight e.g. 1mg/kg b.d
- Does NOT effect APTT ( Activated Partial Thromboplastin Time)
- can measure factor Xa activity (Rarely done)
- Renally excreted therefore caution / dose adjustment in renal failure
Heparin / LMWH - Uses
- What is it used for?
- What is it used in the treatment of?
- Prevention of thromboembolic disease (DVT /PE)
- thromboembolic disease (DVT /PE)
–Initially prior to Warfarin
–In pregnancy
–(On going malignancy)
- Treatment of Acute Coronary Syndrome (ACS)
- Treatment of acute peripheral arterial occlusion
- Extracorporeal circuits (haemodialysis)
* Works for venous and arterial occlusion (antiplatelet drugs DONT)
Patients in hospital given low dose LMWH to prevent DVT at patients lie around
Heparin
- Outline the main adverse effects
- What are the rarer side effects?
- •Haemorrhage – maybe reversed with protamine sulphate
- Hyperkalaemia (Hypoaldosteronism)
- Thrombocytopenia (a low platelet count)- Transient early relatively common. HIT - rare
- •HIT (Heparin-induced thrombocytopenia)
- Osteoporosis (>6months Rx)
- Hypersensitivity
- Thrombosis
Heparin-Induced Thrombocytopenia (HIT) - Rare
- What is it characterised by?
- What should you do if it is suspected?
- •Immune-mediated
–Usually 5-10 days in to Rx
–>50% drop in platelet count
–Thrombosis
–Rash
- –Stop heparin and use an alternative anticoagulant
–Measure heparin-platelet antibodies
–Consult haematology
Oral Anticoagulant – Vitamin K antagonists
Give an overview of this group
- Coumarins: Warfarin
- 1920’s N America
- Spoiled sweet clover
- Wisconsin Alumni Research
- Foundation
- Rat poison
- Main oral anticoagulant
Warfarin - Mode of Action
- What is the mode of action?
- What does this mean for onset?
- What is used to cover this delay?

- Competitive inhibitor of vitamin K epoxide reductase. Prevents the post-translational gamma-carboxylation of factors II, VII, IX and X
- delayed for a few days until the already formed active factors are degraded
- LMWHeparin is used at the start to cover this delay

Warfarin
- What is it used for?
-
Treatment of thrombo-embolic disease
- (DVT / PE)
- Atrial fibrillation
- Mechanical prosthetic heart valves
Only used for treatment, not prophylaxis
Warfarin - Dose and Monitoring
- What should be checked at baseline?
- How long is a loading dose given for?
- How is the maintenance dose adjusted for?
- What should be continuously monitored?
- prothrombin time (PT)
- 1-3 days
- •Measure the International Normalised Ratio
(INR – ratio of patient’s PT and control sample)
- Adjust maintenance dose based on serial INR readings
- Aim for INR value for the given condition
–E.g. DVT: 2.5, AF: 3.0
- INR must continue to be monitored at a warfarin clinic throughout treatment period
Warfarin
What are some general precautions that need to be taken?

Important that people are aware you are on warfarin.
Any new prescription shouldn’t alter INR
Now have ‘Point of Care Testing’ – can measure straight away in GP.
Yellow warning cards being phased out.
Warfarin
- What can cause variation in warfarin effect?
- Diseases
- Acute and chronic liver disease
- Right ventricular dysfunction (CCF)
- Thyrotoxicosis
- Drug interactions – MOST CLINICALLY IMPORTANT
- Genetic variation
- VKORC1
- CYP450-2C9 (and others)
Warfarin
What are the adverse effects?
- Haemorrhage / High INR
- Drug interactions
- Unexplained fall in Hb
- Teratogen – avoid in pregnancy (esp 1st and 3rd trimester)
- Alopecia
- Skin necrosis
(If your PT/INR test result is too high, it means that your blood is clotting too slowly, and you are at risk of bleeding. Your dose of warfarin is too high. On the other hand, if your PT/INR test result is too low, your dose of warfarin may not be enough to protect your blood from clotting.)
Haemorrhage on warfarin
What actions should be taken if there is major bleeding?
- Vitamin K (slow iv)
- Prothrombin complex concentrate or Fresh Frozen Plasma (FFP)

*Warfarin - Drug Interactions*
Give examples of drugs that INCREASE warfarin’s effect?
- Antibiotics
- Amiodarone
- Cimetidine
- Clofibrate
- Fluconazole
- Metronidazole
Not a finite list (BNF Appendix 1 Interactions)
- Alterations in alcohol + diet
- (antiplatelet drugs and NSAIDs – increase bleeding risk)
*Warfarin - Drug Interactions*
Give examples of drugs that DECREASE warfarin’s effect?
- Barbituates
- Carbamazepine
- Rifampicin
- Sucralfate
Not a finite list - see BNF Appendix 1 Interactions
•Alterations in alcohol + diet
Warfarin
What are the contraindications?
What are the relative contraindications?
- Pregnancy
- Active bleeding
- Peptic ulcer (recent) (3-6months)
- Uncontrolled severe hypertension
- Bacterial endocarditis
- Recent surgery
- Liver / renal impairment
What are the ‘New Anticoagulants?’
Give Examples
- Direct Thrombin Inhibitors
- Dabigatran
- (Bivalirudin)
- Direct factor Xa inhibitors
- Rivaroxaban
- Apixaban
New Anticoagulants
- What do the Direct Thrombin Inhibitors target?
- What do the Direct factor Xa inhibitors target?

- Thrombin (IIa)
- Xa

New Oral Anticoagulants (NOACs)
Why was there a name change to DOACs (Direct Oral Anticoagulants)?
What are these?
NOAC was read as “No anticoagul’, didn’t get coagulation, so name has been changed
- DabigATran
- AntiThrombin (direct Thrombin inhibitor)
- RivaroXaban, ApiXaban
- direct Xa inhibitors
DOACs
- What are the advantages?
- What are the disadvantages?
- –Orally available
–No need for monitoring INR (but still need to monitor patient and other blood tests!!)
- –No reversing agent developed yet
–Less known about these agents i.e. efficacy and safety
DOACs
- What are their indications for use?
- What do the dosing regimens depend upon?
- When are they NOT recommended
- What are some other points of note?

- Stroke prevention in patients with non-valvular AF
Prevention and treatment of DVT/PE
- indication, renal function, weight and age
- Pregnancy or if an artificial heart valve present, liver disease or malignancy
- Complex switching regimens between the different anticoagulants. Variable discontinuation times for differing procedures based on bleeding risk

What are the doses for
- Dabigatran
- Rivaroxban
- Apixaban
- 150mg bd
110mg bd
- 20mg or 15mg daily AF
(15mg bd 3wk then 20mg daily DVT/PE)
- 5mg bd or 2.5mg bd AF
(10mg bd 1wk then 5mg bd, 2.5mg bd after 6mth DVT/PE)
How are these excreted?
- Dabigatran
- Rivaroxban
- Apixaban
What monitoring is needed for these DOACs?
- 80% renal
- 60% renal
- 30% renal
U&E, LFTs, FBP, Coagulation profile
3mth adherence
ADRs/efficacy
6-12mth FBP, U&E, LFTs
Heparin - Summary for general perusal
- Unfractionated or LMW Heparin
- Given as subcut or intravenous injections
- UFH-ATIII complex inactivates Xa and IIa
- LMWH-ATIII complex inactivates Xa
- Used for prevention and treatment of DVT /PE, ACS, Acute arterial occlusion etc.
Adverse effects
–HAEMORRHAGE
–Thrombocytopenia
–Hyperkalaemia
–Osteoporosis
Warfarin - Summary for general perusal
- Oral anticoagulant
- Inhibits vitamin K epoxide reductase preventing formation of factors 2,7,9,10
- Used for treatment of DVT, PE, AF, mechanical heart valves
- MUST be closely monitored with INR
- MULTIPLE drug interactions
Adverse effects
–HAEMORRHAGE
–Occult decrease in Hb
–Teratogenic
–Alopecia / skin necrosis


