Introduction to respiratory pharmacology + Anti-inflammatory medications: preventors Flashcards
What is asthma? 3 characteristics?

Goals of treatment with asthma?

What are the different classifications of asthma?

Explain the origins of asthma? (thing which sensitises people)
Exposure of antigetn (virus, allergens) to the dentrites. These are then given to the T helper cells. These CD4 cells often do not respond to this.
However, in an asthmatic the interlukens are released which activates the CD4 cell which, these then activate B lymphocytes and then activate eosinophils which produce this inflammatory response when the antigen is next exposed.
B cells = IgE response which bind to mast cells and eosinophils in bronchi. Re-encounter causes release of inflammatory cytokines and histamine.

What extra things (not histamine and cytokines) are released when an asthma exacerbation occurs?

What are each of these responsible in asthma?


What are the ‘slow-reacting’ substances of anaphylaxis’ in asthma? What affect do they have?
If we want to target this then we need to decrease C,D and E but also B4 because B4 is the chemoattractant.
This is done by knocking out the 5-lipooxygenase enzyme.

What do prostacyclins and thromboxane A2 do in asthma?

Why do you not want to completely knock out all of the prostaglandins?

Explain drug induced rhinitis?

Mechanism of a B2 agonist on asthma?
What is the second messenger?

Why do you also need a muscarinic antagonist a long with B2 agonsit?
Essentially the beta 2 receptors work in the opposite direction to the muscurinic receptor.

How does theophylline work?
Increases the availability of cAMP as it is a PDE inhibitor

How do muscarinic antagonists work?
Muscarinic antagonist will block the effects of acetylcholine therefor prevent bronchoconstriction.

What are the anti-inflammatory compounds which can be used (aka preventors)?
Inhaled vs oral

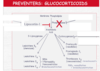
How does glucocorticoid work?
Will bind to the surface receptor which will chaperone it into the nucleus to alter cell function.
- Highly effective at suppressing inflammatory cytokine production.
- prevents phospholipid release and decrease eosinophil recruitment

Glucocorticoid upregulates gene transcription of _________ inhibitors such as ________. This has the effect of….


Does glucocorticoids cause bronchodilation ?
NO: but over time decreases the airway responsiveness.

Oral corticosteroids systemic effects?

Some side effects of glucocorticoids?

Explain the cushingoid effect and some other side effects of high dose oral corticosteroids?
How can you avoid this with respiratory diseases?
Inhaled reduce the systemic effects of oral corticosteroids.

Main example of inhaled glucocorticoids?














