Hypersensitivity and Autoimmunity Flashcards
(28 cards)
What is Immune Hypersensitivity?
An over-reaction of the immune system causing pathology
WHat are the Gell and Coombs classification of immune reaction types?
Type 1: IgE-mediated (allergic or anaphylactic)
Type 2: IgG-antibody-mediated (cytotoxic)
Type 3: IgG immune complex-mediated
1-3 all antibody mediated over-reactions
Type 4: T-cell mediated activation of CD4 Tcells (DTH-delayed type)

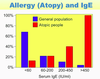
Allergy (atopy) and IgE in the general population
- Lowest concentrated antibody in the blood is IgE
- BUT some people have significantly raised specific IgE types against some specific often innocuous allergins
- Unsure why, some is related to the change in distribution of Th cells (Th1 Th2 etc)
What is IgE and where do uou find it?
What does it cause in these cells
Produces antibodies bind to high affinity FcER (epsilon receptors) regions of Mast cells and basophils.

Mast cells: found on mucosal surfaces and in skin, so once they meet allergin, they bind the IgE at the epsilon receptor, and that signals the cell to Degranulate (release a bunch of pharmacoactive substances from granules in it’s cytoplasm)
What happens once a mast cell has begun to ‘degranulate’
(caused by the cross-linking of the IgE)
The molecules released from the granules do a number of things.
- Attract neutrophils to the site of release
- Activators of vasodilators, complement platelets
- Spasmogens; some smooth muscle contraction, mucus secretion
**this is also all triggered by C3a and C5a and some drugs

Common causes of Allergies?
Rhinitis: House dust mites, pollens, animal dander
Insect Stings: Proteins in venom induce IgE production, anaphylaxis is common.
Food Allergies: Wheat protein, milk proteins, peanuts, strawberries
Small molecules: Penicillin, codeine, corphine
Common sites of allergies?
Respiratory Tract:
- Allergic Rhinitis (hay fever)
- Sinusitis (inflamed nasal sinuses)
- Conjunctivitis (inflamed conjuctiva in eyes)
- asthma (w allergic component)
Skin:
- Urticaria (weals)
- Angioedema (deeper skin involvement)
Gut:
- Food allergy (diarrhoea, abdo cramps, vomiting)
How do you deal with/treat Type 1 allergies?
- Avoidance: often difficult
- Antihistamines: common for mild forms; eg; hay fever
- Corticosteroids: essential for chronic condition such as asthma
- Sodium cromoglycate: Stabilises mast cells
- Sympathomimetics: epinephrine (adrenaline) in anaphylaxis
- Desensitisation: gradually increasing doses of allergen to induce high affinitiy IgG antibodies (compete with IgE for allergen) good for bee-stings
Type 2 Hypersensitivity
- Antibodies against cell-surface antigens
- here we have some surface w antigen that I am making antibodies (yellow against) it binds my own tissue antigen and then does
- Serves as a focus for my neutrophils which have an affinity for my FcgammaR and become activated to deliver killing signals in the form of ‘cell-mediated cytotoxicity’
- Antibodies bound to antigens form ‘immune complexes’ change in the CH2 domain → complement activation
- leads to membrane attack complex
- deposit C3b which act as an additional attachment for neutrophil → frustrated phagocytosis where they release vacuole contents to cause damage to the cell they’re bound to

Examples of Type 2 hyper-sensitivity are….
WHat is haemolytic disease of the newborn?
- Organ specific autoimmunity
- Haemolytic disease of the newborn
- Anti-RhD red cell IgG antibodies
- RhD- mother becomes pregnant with an RhD+ fetus. First pregnancy fine but the mixing of the babies red cells with the mums circulation exposes the B cells → antibody response (initally IgM then IgG)
- If she then becomes pregnant with another RhD+ fetus, these IgG antibodies will be transported across the placenta and lead to Complement-mediated lysis of the Red Cell Haemolytic Disease

Treatment of Haemolytic disease of the Newborn?
- Immediately after the birht of the first child, you passively inject the mother with anti-RhD antibodies to neutralise and remove any of the babies red cells that may be remaining.
- This stops the sensitisation of the B cells, so that if another RhD+ baby was born it would not have been affected (she will, however still require another dose of the anti-RhD antibodies)
Describe Type 3 Hypersensitivity??
- antibodies that are forming soluble Immune complexes
- eg; infection that is chronic, the amount of antigen will persist for a little longer, and these may be around suring the period of time our IS begins to produce responsive antibodies → immune complexes
- When we have an equal balance of antibody and antigen the complexes that form are large, lattice-like complexes that:
- Large so sticky and lodge into small vessels
- Multiple sites for complement activation (andif IgG, alot of Fc regions for NP attachment)

Vasculitis and Bephritis induced by Type 3 Hypersensitivity?
These are pathological consequences that can occur in addition to removal of the antigen due to the presence of large, lattice like Immune-complexes.
Can Cause:
Vascular Damage: May lead localisation in vessels, organs etc that cause cause occlusion, microthrombus formation, neutrophil recruitment, complement activation and therefore further neutrophil activation, components of the complement cascade damaging the blood vessel wall. The complexes themselves and damaging but what they cause is!!

Type 4 Hypersensitivity can be tested by…
Mantoux Test: immune memory assessment eg; intradermal TB, mumps, candida albicans
- Take small amount of antigens, inject under the skin and wait 24-48hrs.
- if they have a lot of CD4 memory cells circulating they enter this site, be triggered by the antigen, release cytokines, change vessel permeability → red, swollen, lump
- ‘Delayed Type Hypersensitivity Reaction DTH’
Contact Sensitivity:
*
Contact sensitivity (Type 4 HS) is?

- Typically something with small chemical ions or solvents etc
- If repeatedly exposed to this, the skin will take up the antigen, process it and present to memory Th1 cells circulating. If still exposed then these cells will eventually come back into contact with the stimuli and cause an inflammatory reaction eg; Adult excema
- Macrophage and Lymphocyte recruited
How this happens: sometime small molecules (nickle/ions) will chemically attach to some proteins (these become ‘carriers’) becoming antigenic structure big enough to be seen by the immune system.
These can now stimulate an immune response and T cell stimulation, if the stimuli remains (keep jewellery on) then memory Th1 cells will return and provoke inflammation.

Haptens?
The small molecules in contact sensitivty that alng cannot cause an immune reaction but can bind to our normal proteins to form an antigenic complex
Type 2 and 3 are the reactions that we see in __________. This is generally classified into 2 groups.
- .
- .
Type 2 and 3 are the reactions that we see in Autoimmune reactions. This is generally classified into 2 groups.
- Organ Specific (Type 2)
- directed against particular tissue and causes localised damage there
- Systemic (Type 3)
- Antibodies against soluble molecule, form immune complexes.
- Describe Autoantibodies that we find. How common are these?
- Natural IgM low affinity autoantibodies common
- to a variety of self-antigens that cause no pathology
-
Anti-nuclear antibody (ANA) against RNA and DNA
- Increase with age, common in elderly people
- Seen in Systemic Lupus Erythematosis (SLE)
-
Anti-Thyroid antibodies
- Seen in Thyroid disease
- in 10% of elderly; only cause disease in <2% as levels too low
So whilst Autoantibodies are common, autoimmune disease is RARE
What are our Mechanisms of Tolerance against Self antigens?
- Clonal Deletion (central as where we are building repertoire)
- Bone marrow and Thymus; delete all cells that have a high affinity for self-antigens
- Clonal Regulation (Peripheral)
- No co-stimulation; anergy: when a self antigen is presented to an APC
- Suppresion (peripheral)
- Actively activating CD4 cells to regulate the particular antigens, to control self-reactive cells.
- Ignorance
- There are some parts of our body where we make antigens that our immune system is not allowed to see! Eg; eye, testes. Immunologically privileged sites
Molecular Mimicry causing autoimmunity
- Infection (with certain bacterial peptides) presented to my immune system, and coincidentally those bacterial epitopes look very similar to some self-peptides
- A response to the bacteria cross-reacts to my own tissues → Autoimmune Phenomena (post-infective)

*Doesn’t mean they are the same, just that the T cells think they look the same!
**Doesn’t occur in everyone, dependent on their HLA haplotypes!
Organ Specific Autoimmunity Examples?
Antibodies against specific organ tissue
Outcome/presentation vaires dependent on the tissue!

Goodpastures Syndrome: against glomerular BM
Myasthenia Gravis: Block AChR ⇒ muscle issues
Hasimotos Thyroiditis: Destroys thyroid tissue till no thyroxine
Idiopathic Thrombocytopenia Purpura (ITP): against platelets
Addisons Disease: Destruction of adrenal cortex, hyperpigmentation
Skin …..
IDDM
IDDM - diabetes
Autoantibodies and cytotoxic T cells against Pancreatic Beta cells compromising insulin ⇒ low insulin issues
Pernicious Anaemia
- Autoantibodies against Parietal Cells
- Stops production of Intrinsic Factor
- Can’t bind/ uptake vitamin B12
- Can’t make Red cells

What’s Graves Disease and how is it different to other autoimmune diseases
Doesn’t cause destruction of the tissue, instead overstimulates it.
- Antibodies against TSH receptor of thyroid cells
- Stops Thyroxin being produced that is the regulatory negative feedback molecule for the thyroid
- When the AAB bind, it overrides the system ⇒ chronic thyroid stimulation → even though we stop TSH due to high thyrocin levels the AAB still stimulates





