Fever and Cough: Pneumonia Flashcards
Describe Bronchitis and how it differs from Pneumonia.
- Benign viral inflammation of the conducting airways
- Antibiotics don’t improve
- cough sometimes with sputum
- Not usually fatal, benign and self-limiting
- Doesn’t impact gas exchange
- can cause a VQ mismatch
Whereas pneumonia is potentially fatal infection that starts in the lower alveolis themselves, filling with pus. and involving gas exchange. Strep. pneumonei most common cause and doesn’t cause bronchitis.
Are antibiotics an effective treatment of pertussis (whooping cough)
AB’s have NO difference in symptoms but you decrease infectivity and risk of spread to family/friends
What’s the best to distinguish Bronchitis from pneumonia?
The best way is experiance!
Investigations
- Chest xray
- auscltatioin
- chest expansion
Clinical features
- Listen to breathing: hear changes in breath sounds, hear crackles
- Place hands on chest
- Are they short of breath?
- Percuss and find dullness
How is pneumonia in the elderly different then usual?
Fever 50%
Consolidation 30%
Non-pulmonary 20% (eg; delerium or falls)
RR 69%
Crackles 80%
Pneumonia is a systemic illness particularly in the elderly
How do people develop pneumonia?
Via Aspiration from the upper airways
- We all microaspirate when we are asleep!
- You get a nasty pathogen down your lungs and your innate immune system cannot deal
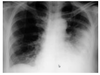
what’s wrong?

- Infection of the Left lung (LLL and LUL)
- White pus
- Bronchiae are more visible due to an interference between tissue and pus
**note the RUL pneumonia also and a horizontal fissure
this person is shunting blood into the left lung, and so not getting mych oxygen around their body, you can see the ventilatory wire
?

Pneumonia of the LLL and the diaphragm is really hard to follow!
Somes a lateral view is helpful too.
If their is no lung-diaphragm interface, it’s a lower lobe infection!

What are the risk factors for developing pneumonia?
- Age <2 or >65
- chronic lung disease
- smoking
- immune dysfunction: this can be anything!!
What are the main causative agents of pneumonia
((remember the list))
Pneumonia is a bacterial infection (red) caused by
- Streptococcus pneumoniae*** 20-60% of cases, by far most common
- Chlamydophila pneumonia
- haemophilus influenzae ~5-10%
- staph. aureus rare but consider if severe
- Legionella (mild but very severe)
- INFLUENZA 8-16%
Pneumonia the worst/most common of most serious/deadly bacterial infections. And very often we don’t even find the cause!!

Describe Streptococcus pneumoniae
- Alpha haemolytic streptococcus: can partially haemolyse RBC (B-haemolysis is when they are fully haemolysised)
- VIridans group related to S.mitis
- Colonises the nasopharynx: 5-10% adults, 20-40% children
- Prevalence of colonisation increases in winter
- Colonisation persists for a few weeks in adults
What is this picture of two different strep. pneumonia showing?

Cultured new S.pneumonia in the presence of dead ones.
Dead ones producing sugary capsule, but the new ones aren’t. when mixed, the new ones took up the DNA of the dead ones, but not the ability to make the sugary capsule.
The difference is that the new ones aren’t virulent, proving the capsule is vital for the bacteria to be able to cause disease!!!
How does strep.pneumoniae capsule cause virulence?
The capsule prevents neutrophil recognition and phagocytosis, as well as opsonisation. Also avoids abtibody depositi
- Complement factor C3b can’t bind to the sugary capsule
- Releases pneumolysin toxin into the lung that lyses neutrohpils and epithelial cells in alveoli
- Choline Binding protein binds to immunoglobulin receptor that acts as a trojan horse, able to get into epithelial cells
- Pneumococcal surface protein AL binds to epi cells and prevents C3b deposition
- pili help colonisation
- PspC prevents complement

Invasive pneumoccal disease (not just pneumonia)) has rates of…
- 12.2/100,000 people
- But much higher in elderly and children!
Seasonality affects adults more in Winter!
Once a patients pneumonia is confirmed, what investigation or questions should we be thinking about?
Think…
- How sick are they now (what’s gonna happen)
- What is the bug (if it’s important)
Usually treat with antibiotics assume it’s strep. pneumonia if mild!!
If kidney function is declining, this is a sever case with a worse prognosis. With severe cases try find out the bug!
*remember that people often present when they are at their sickest, so if they seem okay with only mild pneumonia, once treated with ABs they shouldn’t ‘crap out’

Antibiotic Treatment is required to reduce duration of illness and risk of death. NZ is pretty bad at over-prescribing penicillin for resp issues.
What issues does this bring?
- Penicillin resistance is increasing! mediated by altered PBP/transpeptidase which REDUCES penicillin binding affinity (not completely stopping like MRSA). This could be reduced by vaccines
- Oral dosing might be inadequate, IV dosing will be okay and overcomes binding issues consider when treating meningitis from strep. pneu
- Penicillin resistance is ass. with resistance to other ABS
Bacterial ribosomes are different to human ribosomes. How can we take advatage of this?
By therapeutically targeting these differences
- 5OS transoeotidation macrolides, lincosamides
- 5OS peptidyl transferase chloramphenicol
- 3OS initiation aminoglycosides (bacterocidal)
- 3OS tRNA binding tetracyclines

Why are macrolides important?
They bind where the transfered RNA is meeting the transcribed DNA, stopping the DNA handing it’s peptide over, stopping protein synthesis and the cell ‘can’t go on’
- various forms
- ABs mainly used for pneumonia, and when people are allergic to pneumonia
- also treatment for chlamydia
Adverse effects of Macrolide antibiotics are?
- GIT upset: erythromycin agonist of motilin receptor, increases peristalsis
- Sudden death: class effect has an impact on cardiac conduction
- Drug-drug interactions


