HTN Flashcards
Special considerations
Renal disease- Initial increase in creatinine normal….. Contraindicated in bilateral renal artery stenosis ACE might temporarily increase creatinine but should level off if not they might have bilat renal artery stenosis- we are blocking BF to renal arteries
CAD- BB’s may be added to ACE-I
Diabetes Mellitus- Usually need multiple agents Avoid adverse glucose metabolism Lower BP goal ACE-I or ARB 1st line
Reproductive women- Estrogen stimulation of hepatic angiotensinogen
Elderly : > 75y/o Modest doses reduce stroke
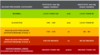
Stages of hypertension
•Stage 1
Modify lifestyle
May add monotherapy anti-hypertensives w/ co-morbidities
CAD/stroke risk or DM/CRI (renal disease)
•Stage 2
Will use combo therapy (systolic 140 or higher/ diastolic 90 or higher) diuretic and beta blocker or something
Which number is more related to cardiovascular risk? Systolic or diastolic?
- Systolic- Max pressure to eject blood out of heart; higher max pressure on a constant basis= more ling term weakening to BV’s
- Diastolic- Lowest pressure arteries go thru; lowest pressure is still pressure; also not enough can cause poor coronary artery perfusion
- Also pulse pressure matters= the wider it gets the less coronary artery filling you have
Why does BP control matter???
- 7/10 people having their 1st MI= uncontrolled BP
- 8/10 people having 1st stroke= uncontrolled BP
- 7/10 people with CHF= uncontrolled BP
Types of Hypertension
Essential/ Primary/ Idiopathic: an identifiable cause cannot be found: Interrelated renal, hormonal, vascular
Secondary: an identifiable cause is present (pheocromcytoma
Essential: Commonalities
- Familial incidence
- Deficiencies of endogenous prostaglandins and NO
- Renin or adrenergic dysfunction
RAAS

Low renin hypertension- subset of essential HTN
- Salt-sensitivity
- Diuretic responsiveness
- Expanded extracellular fluid volume
- African descent, diabetics, elderly- thiazides
High renin hypertension
- Plasma renin levels above normal
- Poorly responsive to competitive antagonists of angiotensin II- 50%
- Increased adrenergic activity- give beta-blocker
Modulation defect
- Salt-sensitivity: kidney doesn’t excrete Na+ properly
- More insulin-resistant: getting type II DM at the same time
- Susceptible to ACE-I
- Males, postmenopausal
Diagnosis of HTN
•Persistently high resting blood pressure
Per month x 3
Seated, back supported, feet on floor
Not talking, arm on flat surface, level with heart
Correct sized cuff
Diagnosis Lab

Treatment of Stage I w/out co-morbidities
•Lifestyle modifications
***Diet/weight loss
Moderate alcohol intake
Increase physical activity
Cessation of smoking
Sodium restriction
Initial Pharmacotherapy- HTN
•Stage I – risk for CAD or stroke/ already have DM
Monotherapy: Diuretics, CCB, ACE/ARB
BP goal < 130/80
Sequential addition if needed- 2nd drug of different class
•Stage II
2 agents, different classes= usually ACE/ARB or CCB and diuretic
Separate or combo (can have both drugs in one pill)
Diuretics
thiazide most used for HTN, loop more short-term, can swap to K+ sparing if loop causing prob

Diuretic therapy considerations
- Sodium diuresis/volume depletion
- May decrease PVR: max pressure to artery
- Effective within 3-4 days
- Out of favor (d/t hypokalemic side effects but….. < 25 mg/day HCTZ we don’t have bad hypokalemia
ACE INhibitors

ACE-I therapy
- Inhibit generation of potent vasoconstrictor
- Retards degradation of bradykinin- 2 armed approach w/ vasoconstriction
- Especially useful in diabetic patients- prevent negative side effects of excessive carbohydrates
- Cough 5-10%, hyperkalemia, angioedema- w/ ARBS don’t have
ARB’s

ARB therapy
- Most selective blockers of R/A system
- Fewer side effects than ACE-I
- Blocks Ang II from attaching to receptor- we do not currently know if there is a long term effect of blocking but still circulating Ang II
CCB’s

CCB therapy
- Modify calcium entry thru α-1 L-type voltage channels but more than 1 type (at least 3)
- Specificity to unique binding sites…
- All: vasodilation
- Only Diltiazem and Verapamil: slow AV conduction
Secondary Hypertension
- 5% of cases
- Renal artery stenosis most common cause
- Other examples
Pheochromocytoma
PIH
Cushings’s syndrome
Coarctation of the aorta
Systemic Hypertension: AHA