Hormone-dependant cancers (breast and prostate) Flashcards
How are steriods synthesised?
Steroids are small, multi-ringed and can easily enter cells by passing through the plasma membrane

How do steroids hormones work systemically in males and females?
Females - oestrogen controls the menstrual cycle and breast tissue development, fertility and reproductive organ development
Males - testosterone controls reproductive and supportive organs, development of sexual characteristics in me
How are breast and prostate tissues strongly controlled by steriod hormones?
The tissues are hormone dependent, as steroids govern their growth and development
- Controls how the disease develops and progresses
- But also can be exploited when it comes to treatment
How do steroid hormones bind inside the cell?
Steroid hormones enter the cell and bind to receptors called nuclear receptors each having a unique receptor for each steroid

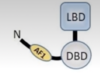
What makes up the nuclear receptor?
Ligand binding domain (LBD) - binds specific steroid molecules with high affinity
DNA binding domain (DBD) - binds specific DNA sequences
Activation function domain (AF1 and 2) - recruits gene activation machinery
What are the 2 zinc finger domains?
DNA binding domain contains 2 zinc finger domains, which are essential for sequence specific DNA binding

What is the breast made up of?
Apocrine gland that produces milk to feed an infant
- Specialised exocrine gland in which a part of the cell’s cytoplasm breaks off releasing the contents
Composed of glands and ducts which produce the fatty milk
15-20 lobes - each with lobules where milk is produce
Milk travels through a network of ducts which come together and exit in the nipple
Mammary glad is located in the breasts and consists of 2 cell compartments:
- Luminal - form a single layer of polarized epithelium around the ductal lumen, luminal cells produce milk during lactation
- Basal - cells that do not tough the lumen, have contractile function during lactation

What are the 2 major phases in breast development?
Hormone-independent from embryonic development up to puberty
Hormone-dependent thereafter during puberty, menstrual cycle and pregnancy
What are the different hormones involved in the life of a human?

What is breast cancer?
Occurs when abnormal cells begin to divide in uncontrolled way
Starts in breast tissue, most commonly in the cells that line the milk ducts
Age - later onset
Genetic mutations like BRCA1 and 2 are at higher risks
Risk factors - weight, underactive, taking hormone replacement, drinking alcohol
What is DCIS?
= Ductal breast carcinoma in situ
When cancer cells develop within the ducts of the breasts but remain within the ducts, they haven’t yet spread outside
What is LCIS?
= lobular breast carcinoma in situ
Abnormal cells form in the milk glands (lobules) in the breast
Isn’t cancer - but if you have it you could have a increased risk of getting cancer
What is the relevance of ER in breast cancer?
**in normal breast ER controls cell proliferation and development and differentiation in a controlled manor
- In breast cancer it becomes uncontrolled
- ER’s ability to bind DNA and open chromatin becomes hijacked and is used to transcribe many genes
The majority of breast cancers arise from the luminal cells which express ER (oestrogen receptor)
- ER positive - good prognosis
- ER negative

What happens if you swtich off ER signalling?
switch off the cancer growth - targeting ER in breast cancer for treatment
If you are ER positive
What is Fulvestrant?
= is a drug that competitively inhibits binding of oestradiol to the ER, with a binding affinity that is 89% that of oestradiol
It impairs the receptor dimerization, and therefore blocks nuclear localisation of the receptor
Any Fulvestrant-ER complex that enters the nucleus is transcriptionally inactive because AF1 and AF2 are disabled
- The complex is unstable, resulting in accelerated degraded of the ER protein

What is tamoxifen?
= drug that can inhibit ER
- Binds the ER at the ligand binding site
- Partial agonist but does not cause full activation of ER - mixed activity but works as a antagonist in the breast tissue

What is the prostate?
Main function of the prostate is to produce prostatic fluid that creates semen when mixed with the sperm produced by the testes
The prostate is an exocrine gland - secrete substances out onto a surface or cavity
How does the prostate gland develop?
- hormone - independent from embryonic development
- Enlargement during puberty
- Hormone-dependent maintenance thereafter in adulthood
- Reactivation of prostate growth in old age - leading to hyperplasia and prostate cancer
What are the symptoms of prostate cancer?
Frequent urination
Poor urinary stream
Urgent need to urinate
Lower back pain
Blood in the urine

How does cancer progess in the prostate?

What is the prostate cancer staging?

How does testosterone bind to the androgen receptor?
Testosterone circulates in the blood and can pass the cell membrane
When it enters a prostate cell, its converted by 5-alpha-reductase into DHT
DHT then binds to the androgen receptor with a high affinity
This causes the AR to become activated and dimerized
AR will then translocate into the nucleus where it will bind androgen response elements (specific DNA sequences in the promoter regions of androgen target genes)
Leads to target protein generation and cell growth

How can we treat prostate cancer?
The prostate gland is an androgen sensitive and dependent tissue - androgens are the key driver of prostate cancer growth
- This can be exploited for treatment
- Switch off AR signalling, switch off cancer growth
How can you inhibit testosterone synthesis?
- The adrenal gland derived androgens circulate in the blood and are converted to testosterone in the testes
- Then it circulates in the blood until reaches target organs like the prostate
- The adrenal androgen production can be inhibited, thus depriving the testis of testosterone
- Abiraterone acetate can switch off the making of adrenal androgens
- Synthetic peptides like goserelin and abarelix - these shut down the HPG axis and reduce the overal amount of testosterone production
- 5a-reductase inhibitors (like finasteride) can stop the transfer of testosterone to DHT



