GU bugs Flashcards
describe the disease, locations, and treatment of: papillomavirus, chlamydia trachomatis candida albicans trichomonas vaginalis herpes simplex virus neisseria gonhorrhea HIV treponema Hep B. Hoemophilus ducreyt sarcoptes scabier phethius pubis
STIs are very common infections and will present in a number of ways. Human papillomavirus- lives in the basal membrane Chlamydia- involved in the lung and eye as well Herpes- skin and neuronal

What are the mechanisms of sexual transmission of infectious diseases?
hand, penis/vulva, ano-rectal, and mouth. with the most transmissions among heterosexual and homosexual being penis to vagina, anus, and mouth
What are some strategies of host defenses and how do the microbia respond to this?
- Gonoccochus:
- integrity of mucosal surface of host with microbio able to combat w/ special attachment mechanisms ex. gonorhea or chlamydia
- urine flow-mechanical flushing similar to GI requiring specific attachment or infection of the epithelial surface ex. gonorrhea and chlamydia
- `phagocytes- or resist being eaten due to capsule(ex. gonoccohus)
- inflammation ex. strong inflammatory response, evading consequences ex. gonorhea, candida, hsv, chlamydia (pelvic inflammatory disease)
- igA antibody=producing iGa protease Gonoccocus
- cell-mediated immune response (t cells, lymphokinds, and NK cells (HIV)- antigenic variation allow multipple reinfection (ex. gonoccpcus still with strong immune response)
- phagocytes- bugs induce little inflammation gram negative (treponema siphylis-planning to be around for a while)
- complement- decreasing complement binding covering up the patterns ex. candida

Describe genital lesions and what causes it?
warts?
vesicles?
ulcers?
warts- (most common papilovirus or molluscum contagiosum when immune compromised) viruses and spirochete -verucus (syphilis)
vesicles- virus HSV1 & 2
Ulcers (cratering tissue can be vessels that erupted). firm ulcer or shanker painful shanker is gram -: (Haemophilus ducrey). Painless : spirochete (treponema palidenum syphilis shankers or crater)
ulceration of genital lymph nodes- lymphoganuloma chlamydia

a) 1stsyphilis with a painless, nontenderchancrethat represents vascular involvement, with epidermal hyperplasia, a fibrinous exudate, and dense reactive inflammation in the dermis.
b) 2nd with an infectious maculopapular rash involving the palms and soles, includinglarge condylomatalata, representing widespread endarteritis and lymphocytes infiltrating the dermis.
c) 3rd years later, with CNS and aortic involvement; gummasrepresenting granulomatous inflammation.
likes blood vessels
What is it, what class of bugs is it? source/ virulence? immune response? treatment and/or prevention?
What feature about this allows for a multistage disease?
Spirochetessuch as Treponema(syphilis) and Borrelia(Lyme disease) are specialized elongated Gram-negative organisms with periplasmal flagellae (axial filaments) that allow for a corkscrewing motility through tissues, allowing a multistage disease process.
a) Primary syphilis with a painless, nontenderchancrethat represents vascular involvement, with epidermal hyperplasia, a fibrinous exudate, and dense reactive inflammation in the dermis. Get into tissues and use outer membrane to be disguised particular predilection for blood vessels ex. third stage, killed off blood vessels developing hard indurated eschar and solid from strong local response of penetration. then to the lymph node and inguinal nodes.
b) Secondary syphilis, with an infectious maculopapular rash involving the palms and soles, includinglarge condylomatalata, representing widespread endarteritis and lymphocytes infiltrating the dermis. hematogenous secondary spread develop myalgia and converting rash developing warty reaction to the skin, joints, muscles, mucous membranes
c) . Tertiary syphilis not all destroyed and can go under the surface, years later, with CNS (neural syphilis and exotic spinal cord lesion) and aortic involvement; gummas representing granulomatous inflammation (due to trying to kill hard to kill things-chronic system inflammation leading to breakdown of tissues-gummas from TNF) .
Can cross placenta: Incongenital syphilis, the widespread penetration of the spirochete throughout the fetal circulation can lead to a variety of findings, including rhinitis early on and saddle nose, hypoplastic, notched, spaced Hutchinson teeth.
Diagnosis: Diagnosis may be seen by microscopy (rarely), but more typically by serology with nontreponemalor treponemal tests.
Syphilis does generate abit of an immune response in order to track the pathogen.
nonspecific- cross reactivity antibodies form and cross reacting w/ other tissues. depending upon how the body is responding to syphilis will go down if responding. Thenontreponemal tests measure antibodies to lipid complexes, e.g., Veneral Disease Research Laboratory (VDRL) and rapid plasma reagin(RPR), and these nonspecific titers will drop off with treatment.
specific- targetted to the surface features of the syphillis organism itself will stay up. In contrast, the specific treponemal studies, such as fluorescent treponemalantibody (FTA-ABS) and microhemagglutinatio ntest for Treponema pallidum(MHA-TP), will remain elevated.
While the traditional order has been with the non-treponemal test first, depending on the population, there are diagnostic algorithms that start with the specific tests first.
Treponemapallidum
- Pathogen category: spirochete,microaerophilic, extracellular
- Source: human reservoir, sexual transmission
- Virulence factors: spirochetestructure, hyaluronidase(to penetrate through tissues)
- Clinical: syphilis
- Immune response: antibodyresponse that is ineffective to stop the progression, T cell-mediated response that generates gummas
- Treatment and/or prevention: safe sexual practices; penicillin. A June 2017 meta-analysis suggests that ceftriaxone can be an alternative to penicillin in primary treatment can develop flush or chills in response to killing organisms ;
- Penicillin G, for congenital and neuro, (requiring desensitization if someone is allergic) is still the indicated treatment, with increasing doses as the disease progresses within these stages. Alternatives such as azithromycin have documented patterns of resistance (due to alterations in the spirocheteribosome). an interesting argument has been that a PBP of syphilis has a built-in beta-lactamase function, but also has a high affinity for the subsequent metabolites of penicillin
- One of the striking occurrences that can occur with treatment of syphilis or other spirochetes is the Jarisch-Herxheimerreaction, with the release of the pathogen’s endotoxins in the first few hours after treatment.
- Epidemiology: 30,600 reported cases in US in 2017;
- Timing:Incubation time 3 weeks; may persist for decades (APHA 2008)

Localized- neutrophilicresponse to kill recurrent infection (but does not form long-term infection)
Females:- Largelyasymptomatic; otherwise, purulent vaginal discharge, dysuria, pain, bleeding. Ascending infection will cause PID and risk for sterility
Males:- Purulent discharge and dysuria, more commonly seen
Dissemination is possible, and can be a possible risk factor for a hematogenously-spread septic arthritis, #1 cause of monoarticulararthritis in teens and young adults.
Milking of the male urethra can produce purulent material for Gram stainand DNA probe analysis. If culture is necessary, quick plating on Thayer-Martin medium with CO2enriched atmosphere is appropriate.
There may also be vertical transmission of to the fetus. Neonateswill present with a purulent conjunctivitis.
Neisseria gonorrhoeaeis a Gram-negative diplococcus. Note the variety of features that allow the gonococcus to attach, avoid IgA, minimize phagocytosis, and with the modified LPS in the outer membrane, help to generate a strongly inflammatory response in order to try to clear it. Typical: outer membrane (avoid or adhere, hide from immune response) and inner membrane requiring larger load of cephalosporin coverage in order to destroy.
Pathogen category: Gram-negativediplococcus, aerobic, intracellular
Source: human reservoir, sexualspread
Virulence factors: pili;surface proteins with adherence and antigenic variation
Clinical: gonorrhea
Immune response: strong neutrophil response with local inflammation
Treatment and/or prevention:safe sexual practices; ceftriaxone-thirdgeneration cephalosporin (azithromycinadded for the likely accompanying chlamydia). indicatesincreasing drug-resistant GC increasingly appearing worldwide. every child is treated w/ an eye ointment that will treat it for chlamydia and gonorrhea if the parent had it to prevent blindness
Adaptive system may find way to create antibody to that response, but w/ variability makes it hard to tage
Pili- aid attachment to mucosal epithlium, containing constant and hypervariableregions similar to IgG
Porproteins- gram –need some kind of porinto get through periplasm; forms pores through outer membrane, antigenic, specific serotypes w/ virulence
Opaproteins- assist bindigto epithelial cells adherence and decreasing phagocytotoixactivity
LOS- lipoligosacchardie(endotoxin activity)
Rmpprotein (inhibit cidalactivity of serum)
igAcore contains enzyme released by cell to detroyigA1
Capsule- resists phagocytosis unless anitbodypresent
Neisseriagonorrhoeae
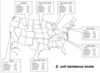
Epidemiology:556,000 cases reported in US in 2017; https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/STD-Trends-508.pdf
Timing:Incubation 1-14 days; treatment quickly stops communicability (APHA 2008)

Females present with:
- •Asymptomatic (80%)
- •Infection of greater vestibular glands
- •Mucopurulentvaginal neutrophilic discharge
- •Vaginal bleeding
- •Dyspareunia
- •Proctitis
- •Rectal discharge
- •Lower abdominal pain
- •Fever
Males:
- •Asymptomatic (50%)
- •epididymidis
- •Urethral discharge
- •Proctitis
- •Rectal discharge
- •Scrotal pain/swelling
- •Fever
Can also present: painful lymphadenitis following initial small papules or ulcers.
conjunctivitis in eyes of children
Chlamydia trachomatis: obligate intracellular parasites that can not make ATP and do not have much peptidoglycan, butdo contain a truncated type of lipopolysaccharide in an outer membrane surrounding their cell wall. Alsoassociated w/ chronic infection of the conjunctiva and scraping eye.
Serotypes D-K cause one of the most common (often subclinical) STIs in the USA. Thesewill tend to rupture at the surface of an epithelial cell and so spread along the genital tract. Affects organs surrounding urogenital tract as well.
Cell mediated response to clear these w/ only several serotypes but many different strains making it hard to fight against. Need to shut down replication or will develop spores (elementary bodies)
Can create a reactive arthritis (cant see, cant pee, cant climb a tree).
Chlamydiatrachomatis
Pathogen category: intracellular, aerobic bacterium withLPS but no peptidoglycan
Source: human reservoir
Virulence factors: elementary body and reticular(includsionbodies proliferating w/in infected host cell); depends on ATP from host cell
Clinical: chlamydialdiseases
Immune response: strong inflammatory and cell-mediated response;generated antibodies are not long-term protective
Treatment and/or prevention:safe sexual practice;macrolides (azithromycin) or doxycycline/.
Chlamydia serotype L causes LGV (lymphogranuloma venereum; particularly seen in developing countries) with its painful lymphadenitis and nodes following initial small papules or ulcers, as this serotype has its reticular bodies rupture morebasally in the infected epithelial cells and so enter lymphatics accordingly. Alonger course of therapy would be needed for this form of chlamydial disease.
Chlamydial diagnosis:
- Fibrous swab
- Culture
- Nucleic acid amplification
Chlamydial treatment:
- Azithromycinor doxycycline
- Consider inclusion of coverage for gonorrhea
Epidemiology:1.7 million reportedcases in the US in 2017; https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/STD-Trends-508.pdf
Timing:Incubation 1-2 weeks; may persist for months (APHA 2008)

IInternational. painful chancre w/ open sore to pustule becoming soft ulceration; may have lymphatic liquefaction, can help facilitate HIV transmission
The painful chancre (you do cry with ducreyi) of Haemophilusducreyiis more commonly seen overseas, with the open sore helping to facilitate HIV transmission.
Hemophilusducreyi
Pathogen category: Fastidious Gram negative coccobacillus
Source: human reservoir
Virulence factors: Pili and fibronectin in the extracellular matrix, cytotoxintriggering cell cycle arrest and subsequent ulceration
Clinical: Chancroid(erythematous papule arising 4-10 days after exposure which then progresses rapidly to pustule and erodes to a painful ulceration 1-2 cm in diameter. Multiple lesions can be present. Lymph node involvement can be present with liquefaction later in the disease, and can have cutaneous drainage with rupture)
Immune response: Perivascular and interstitial monocytes, dermal lymphocytes, and strong neutrophil response
Treatment and/or prevention:Avoidance; ceftriaxone or azithromycin large single dose
Epidemiology: 5,000 cases per year late 1980s; 7 cases reportedto CDCin 2017, but H.ducyreidifficult to culture and so may be largely undiagnosed; https://www.cdc.gov/std/stats16/other.htm#chancroid
Timing:3-5 days; lesions heal in 1-2 weeks after antibiotics (APHA)

vaginitis? what causes it?
will develop yellow discharge w/ fatty odor when KOH added w/ clue cells
puritis and edema of the vulvar area and cottage cheese consisency discharge yeast or pseudomycelia
foamy purulent exudates
gram - rod: gardnerella vaginallis replacing lactobacilli, which is promiment in the vagina. will develop yellow discharge w/ fatty odor when KOH added w/ clue cells. (alters pH of the vagina) making it more prone to subsequent infection and changing dynamics of the introitus (opening)
yeast: candida species develops puritis and edema of the vulvar area and cottage cheese consisency discharge yeast or pseudomycelia. lives here normally comes about w/ antibiotics, diabetics (inhibitted neutrophils), pregnancy (th2 over Th1 dampening strong cell mediated response)
flagellalted protozoa: flagellated protozoa, foamy purulent exudates
Vaginitis may be an issue of protozoan, bacterial, or fungal, with (reasonably) distinctivefeatures for each.

Signs & symptoms:
The initial infection may be asymptomatic, but the presence of a foul-smelling, watery, sometimes greenish-yellow cervical discharge is characteristic. Men may have a urethritis or prostatitis.
Diagnosis &treatment:
•can be diagnosed with wet mount, culture, or more recently, NAAT(nucleic acid amplification tests)
Trichomonasvaginalisis one of the most common sexually treated organisms. It is a flagellated protozoan (swim around)with only a trophozoitestage that triggers a local neutrophilic response (note the appearance of the discharge).
Signs & symptoms:
The initial infection may be asymptomatic, but the presence of a foul-smelling, watery, sometimes greenish-yellow cervical discharge is characteristic. Men may have a urethritis or prostatitis.
Diagnosis &treatment:
•can be diagnosed with wet mount, culture, or more recently, NAAT(nucleic acid amplification tests)
Trichomonasvaginalis
Pathogen category: flagellate(trophozoiteonly)
Source: human reservoir
Virulence factors: mobility,some cytotoxins
Clinical: asymptomatic;vaginitiswith discharge
Immune response: neutrophilsprimarily; ineffective antibody response
Treatment and/or prevention:safe sexual practice; metronidazoleor tinadazole- becauseof it being an oxygen low environment
gram indeterminate
gray watery discharge with fish-like smell; from amines produced (not much inflammatory response) whencombined w/ KOH. Flagellewould try to help clear this less impacting infections, as a presence for more infections.
Gardnerelluyyyavaginalis: the most common agent in bacterial vaginosis.
Virulence factors:
- -changing the enviornment.pH raised (> 4.5) , from loss of lactobacilli that triggers vaginosis.Can allow increasing in yeast infections
- facultativelyanaerobic Gram negative rod that generates a biofilm
Signs & symptoms:
•gray watery discharge with fish-like smell; from amines produced (not much inflammatory response) whencombined w/ KOH. Flagellewould try to help clear this less impacting infections, as a presence for more infections.
Diagnosis & treament:
•clue cellsof vaginal epitheliaand epidermiscontain the bacterium. Need to destroy these cells.
Gardnerellavaginalis
Pathogen category: facultativelyanaerobicGram variable rod
Source: human reservoir
Virulence factors: biofilm
Clinical: bacterial vaginosis
Immune response: littleresponse
Treatment and/or prevention:metronidazole/tinidazole or clindamycin

What is HIV what are the different proteins it produces? what is its virulence etc.
describe its transmission as well
In contrast to therareprimary immune deficiencies touched on during immunology, secondary immune deficiencies are much more common, especially with AIDS(acquiredimmune deficiency syndrome) from HIV (humanimmunodeficiency virus). HIV targets Thcellsby targeting the CD4receptor with the gp120 envelope protein, with additional chemokine coreceptorinvolvement as well. The gp41 envelope proteinassists with viral fusion to the Thcell.
Reverse transcriptasecreates a ds cDNA(complementary DNA) strand that can be integrated into the host helper T cell genome. Viral genes can drive the infected cells to proliferate, and so cause a chronic infection. Large virus, major capsidproteins, RNA strands- carrying own reverse transcriptase to subsequently integrate w/in the host genome w/in cell w/ matrix proteins (between envelope and capid).
Note that there are gag (core proteins), pro(protease), pol(reverse transcriptase,protesase(one bigprotein sliced up allows virus to make protein and then split it up, and integrase)-createdprotease inhibitors first drug, and envgenes (envelope glycoproteins), in addition to others. Attachment versus fusion protein allows the virus toinfect the host cell. Budding- as it multiples can bud out and pick up envelope.
Human immunodeficiency virus
Pathogen category: enveloped +ssRNAvirus (retrovirus)
Source: human. resource-rich countries: common in homoesexual. resource-poor countries: heterosexual relationships to child in utero. can be sexual contact or IVDU receiving infected blood/tissue
Virulence factors: targeting of immune cells; parenteraland/or sexual spread.
Clinical: opportunisticdisease with loss of CD4 cell function
Immune response: initialantibody and CTL response that becomes less effective with ongoing infection of Th1 cells
Treatment and/or prevention:safe sexual practices, blood-borneprecautions; antiretroviraltherapy

What is the HIV life cycle? where do each of the drugs act on it? how do they work? what is recommended to prescribe now?
1) Remember class not name of the agent. Order of development
2) Blocked by CCR5 receptor antagonist. Add ons
3) Blocked by fusion inhibitor. Add ons
4) 2x: Inhibited by NRTI(competitive antagonist of reverse transcriptorsimilar to acyclovir) , NNRTI
5) Blocked by protease inhibitor
6) 1x: Blocked by integrase inhibitor
TheHIV replicationcycle allows for several points of antiretroviralactivity.
Glycoprotein on the surface of HIV- preferentially attaching to CD4 on helperT cells (coreceptorfor T cell receptor). Cytokine receptor on Thcells and other cells on macrophages allowing the ability of the glcoproteinand fusing allowing it to infect other immune cells besides helper t cells.
Penetration:Thesewould be used as second-line agents in HIV for those who have failed primary therapy.
- Maravirocinterfereswith the CCR5 co-receptor necessary for the gp120 on HIV to bind. Block chemokine receptor- blocking that interaction. Add on.
- Enfuvirtideblocks HIV entry by blocking the entry of the virus into Th(helper T) cells.Fusion w/ glycoprotein 41 and virion
Genome replication: use a couple
Targettingvirus w/out membrane potential going after reverse transcriptaseand less side effect profile. Treat multiple ways to prevent proliferation and changing the structure
AZT (zidovudine, ZDV short course to lessen viral load decreasing placental crossing) is the classic exampleof aNRTI (nucleoside reverse transcriptase inhibitor-firstgeneration), with emtricitabineas a more recent example, with tenofoviras aNtRTI(nucleotide reverse transcriptase inhibitor). These lead to cDNA chain termination (AZT is stillused with pregnant women). This is an example of a competitiveantagonist for the RT enzyme.
Efavirenz: a NNRTIpallostericinteraction(non-nucleoside reverse transcriptase inhibitor) binds to binds to reverse transcriptase near its active site, so that it does not produce cDNA very well. This is an example of a noncompetitiveantagonist for the RT enzyme.
Bictegravir: an integrase inhibitor (strand-transferintegrase inhibitor, STII) to complement the NRTIs.
Assembly: anti-retraltherapy when it becameeffective making it a treatable chronic disease. Use one
Protease inhibitors (PI)interfere with an HIV-1 protease that cleaves between Gag and Pol, thus freeing the separate components for proper virionassembly. Darunaviris a currentone. Along with other PIs, it is taken with P450 inhibitorssuch as ritonavirto boost their effective levels.
ART(antiretroviral therapy);increasing indications for starting treatment early, given efficacies of regimens. Guidelines revised 7/10/2019: https://aidsinfo.nih.gov/guidelines
STII (integrase inhibitor) + 2 X N(t)RTIas the preferred current regimen for primary treatment
What is HIV’s pthogenesis? and progression?
- Pathogenesis:
- The high mutation rate of the reverse transcriptase can allow for the increased viral diversity that HIV+ individuals carry. Note that Thcells and macrophages (carried by dendritic cells),both expressing CD4, are targeted by HIV.
- Infected resting CD4 and T cell into lymph nodes where it can proliferate and develop lymphadenopathy.
- Overall, Th cells are targeted to the CD4 co-receptorvia the HIV gp120envelope protein, which also secondarily interacts with cytokine receptors such as CCR5 and CXC4 (named because of the cysteine-cysteine cross-bridging).
- CCR5 is present on other cells, e.g., macrophages, (which along with CD4 expression, indicates why they also become infected with HIV). These “R5” viruses that infect macrophages can then be introduced into places such as the CNS. A CCR5 ∆32 (32 bpdeletion) is a human mutation which is noted for conferring resistance to HIV infection. The “X4” viruses targeting the CXCR4 coreceptoron Thcells, along with their CD4, can lead to HIV-triggered Thcell destruction.
- Progression:
- AchronicHIV infection will lead to CD4+ cell death and hence, loss of cell-mediated immunity. Developing mild illness and initial proliferation in lamina propriadeveloping lymphadenoapthyand a rash that can occur.
T cell infection- can have cytopathic cell killing it, unexpected activation of helper T cells and when one is activating an adaptive cell triggering apoptosis.
HIV specific cytotoxic T cell and MHC 1 w/ expression of MHC particles and proteins triggering killing of infected cells by virus specific cytotoxic T cell. Depressing immune response over time decreasing CD4 and developing new numbers of cells, less Thcells to coordinate a response allowing for an oppurtunisticinfection, which are more lethal than HIV.
Following the initial mononucleosis-like syndrome, HIV progression to AIDS can be marked by a variety of opportunistic infections that are normally controlled by CMI. As the cell count decreases over the years, the more severe the opportunistic infections become.

What is HIV’s virological events? and its response to anti-retroviral therapy?
Stages of virologicalevetnts: acute HIV syndrome, wide dissemination of virus, seeding of lymphoid virus (carried by macrophages), seeding of lymphoid tissues, destruction of gut-assoociatedlymphoid tissue, and establishment of HIV reservoir (glial cells in the brain).
Plasmaviremiaonce the body is generating identifying antibodies, virus specific cytotoxic T cells, viral load tellwahtmomentum.
Current initial testing guidelines: antibody testing for HIV-1 and HIV-2 strains, as well as antigen testing for p24 antigen.
Capsid and other surface protein show up early. HIV antibody-after for weaks
CD4 counts: sense of current status of individual where you are in terms of prediction of future oppurtunisticinfection.
Viral load (HIV RNA via PCR): prognostic
Notethe improvement in CD4 count and the decrease in HIV RNA with ART. Initial huge increase, As CD4 count starts to drop virus kicks up again. Activatingthe immune activation w/ targettingof CD4 specific will develop cytotoxic t cells against it, with death of Thcells that coordinate it means it is a failed response. Antibodies can only affect what is cirulcatingand not what it is in host genome.
Using:NTRY, NnTRY, and integrase proteins. Keepthe viral load low, and CD4 high. Minizmingestablishment of HIV along the way. If keeping them low

What are some opporutinistic infections associated w/ AIDS
Loss of CD4 and Th1, losing cell mediated immunity. Granuloma, neutrophil, and macrophages cannot be controlled. Normally able to target infected cell and clear it out.
Top left to bottom right are classic examples of immunocompromised-associated conditions, with the loss of cell-mediated immunity:
w/ decreasing lower CD4 as you go down…
- Leukoplakia from EBV
- Thrush from Candida albicans
- Kaposi sarcoma from HHV8
- PCP from Pneumocystisjiroveci
- CMV retinitis from cytomegalovirus
- Cryptosporidiasisfrom Cryptosporidiumparvum

•(ineffective) response triggers increased capillary permeability, inhibits gas exchange, leading to the characteristic diffuse bilateral infiltrates and will lead to high mortality if untreated
in immunocompromised individuals
If a huge load normal people can develop mild pneumonia.
Reactivation tuberculosis canoccur in AIDS once the CD4 count starts to drop into the 500/mm3range.
In contrast, Mycobacteriumavium-intracellulare complex:a soil/water organism that is an opportunist for lung and gut infections in immunocompromised patients, when the CD4 count is lower than that for Pneumocystis, e.g., <100 to 50/mm3. A common systemic infection in AIDS patients, including fever, diarrhea, and cough.Clarithromycin, ethambutol, and rifabutin for an extended period represents an effective combination.
As identified in the pulmonary lectures this summer, given that these and related mycobacteria are ubiquitous organisms, immunocompetent patients can occasionally get lung infections from larger inoculations.
Mycobacterium avium-intracellularecomplex
Pathogen category: acid-fastmycobacterium; obligate aerobe, intracellular
Source: environmental
Virulence factors: mycolicacid in cell wall; environmental persistence
Clinical: opportunisticpneumonia with dissemination
Immune response: type IV hypersensitivity with granulomaformation
Treatment and/or prevention:antiretroviraltherapy; combination therapy (not isoniazid). chlarithromycin

A common systemic infection in AIDS patients, including fever, diarrhea, and cough.
environmental pathogen in immunocompromised patigent that can be the basis of brain abscesses.
Similarto MAC, Nocardia(gram _ filament aerobic)is another environmental pathogen that can appear in immunocompromised patients. It can spread beyond the lung embolize, through heart then can be the basis of brain abscesses in such patients.
Nocardiaasteriodescomplex
Pathogen category: Gram+ aerobic,filamentous, branching bacterium. Some acid-fast staining
Source: environmental, e.g., soil, water
Virulence factors: macrophageinhibition (similar to mycobacteria)
Clinical: invasivepneumonia in immmunocompromised; can disseminate and generate brain abscesses
Immune response: cell-mediatedresponse
Treatment and/or prevention:multiplemonths of sulfa drugs similar treatment w/ pneumocystis
demyelination pattern of PML (progressive multifocal leukoencephalopathy) that has a faster onset than multiple sclerosis, high fatality. taking MS meds
Whilea common exposureto the population (80% of adult population with antibodies),the JC virus targetsoligodendrocytes in the CNS in immunocompromised individuals, leading to a demyelination pattern of PML (progressive multifocal leukoencephalopathy) that has a faster onset than multiple sclerosis, and is fatal in approximately 50% of cases.Whilea consideration in patients with AIDS, PML can also occur in patients taking newer MS meds, e.g., natalizumab(monoclonal antibody that blocks integrins, and hence adhesion for migrating leukocytes). Targettingoligodendrocytes (sheathing for CNS neurons), targgettingimunologulationin oligodendrocyte(similar to multiple sclerosis), but can be worsened by the meds that you take to treat MS. Indicationsifbehavior changes and white matter involvement.
JC virus (John Cunningham)
Pathogen category: unenvelopeddsDNA virus (polyomavirus) most have antibodies to it
Source: human; many infected asymptomatically
Virulence factors: reactivation afterimmunosuppression
Clinical: asymptomaticfor many; progressive multifocal leukoencephalopathy (PML)
Immune response: cell-mediatedand humoral response
Treatment and/or prevention:ART if HIV+

ring-enhancing lesion with surrounding edema suggestive of an abscess-type process from the multiplying and feeding tachyzoites. AIDS and if a pregnant lady scoops cat litter.
The sporozoanorganism Toxoplasma gondiimay be of concern for pregnant women (scooping fat litter, or undercooked meat-can cross the placenta) and primary infection,as well as immunocompromised individuals with primary infectionor reactivation.Oocystsare taken in, with tachyzoitesthen feeding or encysting.
Tough cystic stages established elsewhere and can lead to proliferation. Preferentially an animal paraistesimilar to pork worm trichinellaestablished out in the muscle and craniocysticform taken up by cat. Th1 down due to aids or steroid use Toxoplasma can take up the fecal oocystsgetting established and developing enhancement around the site of infection. w/ ring of edema around infection
Toxoplasmawill be the most common brain pathogenin AIDS patients (along with CNS lymphoma), but other agents such as Cryptococcusmay be present as well. Note the ring-enhancing lesion with surrounding edema suggestive of an abscess-type process from the multiplying and feeding tachyzoites.
Prophylaxis wouldbe with sulfa drugs, and treatmentwould be with pyrimethamine (Daraprim; notoriously bought out by Turing Pharmaceuticals and having its price raised 5000% and sulfadiazine (similar to sulfa drugs in terms of their interference with folic acid synthesis), and leucovorin (a reduced form of folic acid for “rescue” of normal tissues). A particular challenge is for pregnant women in their first trimester; a specialized drug (available from Stanford, as it is considered experimental in the US) called spiramycin(macrolide-type agent) would be considered.
Toxoplasmagondii
Pathogen category: sporozoan(apicomplexan)
Source: catas definitive host; other organisms from cat-shed oocysts
Virulence factors: oocysts
Clinical: asymptomaticfor many; toxoplasmosis
Immune response: cell-mediatedand humoralresponse
Treatment and/or prevention:avoidanceof raw or undercooked meat or cat litter or cat-infected soil for spyromycin for pregnant women (if they do not have titers to Toxoplasma); pyrimethamineand sulfadiazine

What is the anatomical basis for UTIs?
what is urethritis?
cystitis
pyelenonephritis
Normally, urine is full of urea and at a low pH, with the bladder being emptied frequently. Alter those conditions and one is more likely to have infection, e.g., with obstruction.
A number of factors can lead to the onset of a UTI, both bacterialand anatomical. Urethral lengthis the major factor in the much higher rate of UTIs among women as compared to men.
Issue offlow- prostate
Alterations of flow-preexisting stones
Bladder trauma-pregnancy
Regular flushing of urine does a lot to prevent seeding of UTI. Colonization will occur and has to do w/ how well they adhere
Bacterial attributes:
Capsular antigens0 covering up PAMP
Urea- modify urea for bacterial benefits
Hemolysis- break WBC
- Urethritis: burning on urination
- Cystitis: dysuria, frequency, occasionally hematuria; possible suprapubic tenderness. There is the possibility of asymptomatic bacteriuria, with a positive urine culture but no symptoms.
- Pyelonephritis:more systemic features like fever, chills, CVA tenderness
Pathogenesis ofpyelonephritis:
- bacteria enter, grow in the bladder, and ascend the ureters to the kidney
- with this bacterial infection, neutrophils are part of the subsequent inflammation
- the renal medulla is vulnerable to bacteria, as the ammonia inactivates complement and the high osmolarityinhibits PMN function. At that point, bacteria can enter the bloodstream and cause septic shock.

what causes most UTIs?
Escherichia coli: greater than 10^5 suugggestive due to some colonizaiton occuring.
Gram negative rod, which in the uncomplicated UTI setting may be covered with sulfa drugs. As the infection becomes more severe, fluoroquinolones would then be recommended.
From the bacterial end, it is the pilli and other factors that allow the pathogens to ascend the urinary tract. Uropathic strains of E. coli have P pili (fimbriae) that allow additional adherence. UropathologicE. colihave adherent pili that the tannins in cranberry juice seem to bind to, hence the discussions that cranberryjuice may be helpful for prevention, although the accumulated data do not consistently support its use.
Other urinary tract pathogens, particularly other Gram-negatives, may be higher on the differential with nosocomial infections.
- Escherichia coli: 80%
- Staphylococcus saprophyticus(on plateà): 10-15%
- Klebsiella pneumoniae: 3%
- Proteus mirabilis: 2%
hospital:
klebsiella and enterococcus

UTI uncommon in young, newly sexually active women. Gram +.
gut pathogen
Staphylococcus saprophyticus: relatively uncommon; part of differential of UTIs in young, sexually active women.
Staphylococcussaprophyticus
Pathogen category: Gram-positivecoccus
Source: human gastrointestinal tractreservoir, normalflora
Virulence factors: lipoteichoicacid;adhesin
Clinical: UTIin young, sexually active women
Immune response: phagocytosisbyneutrophilsfollowing opsonizationby C3b or IgG
Treatment and/or prevention:cephalosporin,Augmentin, or fluoroquinolone, although isoften covered by sulfa drugs in empirical UTI treatment