GI bugs Flashcards
(50 cards)
what are the adaptive immune response in the GI tract?
dominated by IgA generation. Peyer patches- collections of lymphoid tissue, where M cells (microfold) sample antigen in the lumen, generating endosomes to surround and transport that antigen through the cell, to then release that antigen into the interstitium. There, dendritic cells will phagocytose and subsequently present that antigen to the gut-associated lymphoid tissue (GALT) or to the local mesenteric lymph nodes.
What is the innate immune respnose to the GI tract?
normal flora crowd out pathogens, saliva contains lysozymes “animals licking wounds”
esophagus- can be infected w/ candida in HIV
helicobactor pylori-avoids acid pH minimizing normal flora
peristalsis- important for getting rid of worms in the GI tract
bile- protected detergent in order to break up lipids and envelopes (diarrhea from unenveloped viruses)
peyers patch spots of organized opportunities for lymphacytic engagement w/ flora function of antigen sampling

A syndrome characterized by gastrointestinal symptoms including nausea, vomiting, diarrhea and abdominal discomfort.
Gastroenteritis
ex. stomach flu
Abnormal fecal discharge characterized by frequent and/or fluid stool; usually resulting from disease of the ____ and involving increased fluid and electrolyte loss
what is it where is it located?
Diarrhea
small intestine
Inflammation involving the mucosa of both the small and large intestine
what is it?
give example
Enterocolitis
ex. from typhoid
An inflammatory disorder of the gastrointestinal tract often associated with blood and pus in the feces and accompanied by symptoms of pain, fever, abdominal cramps; usually resulting from disease of the ____
what is it and where is it
Dysentery
large intestine
What are the strategies that a bug can do in order to pathogenize the GI?
Pharmacologic action of bacterial toxins, local or distant to site of infection, e.g. cholera, staphylococcal food poisoning
Local inflammation in response to superficial microbial invasion, e.g. shigellosis, amebiasis
Deep invasion to blood or lymphatics; dissemination to other body sites, dysentery in the large intestine e.g. hepatitis A, enteric fevers
Perforation of mucosal epithelium after infection, surgery or accidental trauma, e.g. peritonitis, intra-abdominal abscesses.
Infection of the gastrointestinal tract can cause damage locally or at distant sites.

describe these organisms commonly found in the GI and if they were found in the animal reservoir, food-brone, or water borne

Campylobacter- chicken, sinniameats most are human to human
Salmonella, campylobacter food supply
Chloerain the water supply
watery diarrhea-suggestive of small intestine
bloddy- tissue penetration, mucosal involvement suggest large intestine

What are the incubation periods of these bugs?
what are the responses of these bugs?
diarrhea, vomiting, abdominal cramps, fever
what do the different factors mean?

multi-days must need to multiply
minutes-hours suggest toxin preformed and triggering an elaborate gut response
multi-week duration suggest attachment and not able to be flushed out
salmonella, campylobactera all go systemic

what are the most common diarrheal disease proportion of children in the world?
A)These GI pathogens are common
B)The diseases they generate have overlapping clinical features
●
Rotavirus- not common in country due to vaccinationrate
Cryptosporidium- attacks immune compromise underreported with mild watery diarrhea for those w/ intact immune systems

patient has watery stools w/ vomiting w/ fever what are the bugs?
watery-small intestine
vomiting- stimulating peristalsis
fever- active inflammation at the gut or going systemic. The presence of fever, which would imply tissue penetration and additional system involvement.
salmonella- PMNs in the stools ex. daycare, pets
vibrio-shellfish
norovirus- nursing homes many strains and can develop new strains
rotavirus- child, usually adults vacccinated
dont need to know EPEC

patient has watery stools w/ vomiting w/ no fever what are the bugs?
The non-fever diarrheas here would involve toxins.
mostly gram +, two gram- very watery- large volume of water of cholera

bloody stool with vomiting w/ no fever or no fever what are the bugs?
EHEC- washington county fair infection

dont worry about first ecoli.
bloody stool w/ vomiting w/ fever
w/out fever
Bloody stoolsare associated with dysenteryand colonic involvement. enterocolitis type of level
PMN in stool means that enough dilation and breakdown to get it from the blood stream
shigella- straight dysentery picture, large intestinal dysentery
camplyobacter contaminated meats and person to person, much more systemic
C. diff.- toxins causing pseudomembrane
fever w/ no neutrophils- battle fought in different territory yersinia- peyer patches and inflammatory disease simmilar to appendicitis presentation
no fever- parasitic not bacterial requring eosinophils ex.entomeobea munching where they end up go into intestinal wall and portal circulation, can create liver abscesses causing right upper quadrant pain

Toxin: works similar to the cholera toxin to activate adenylyl cyclase to elevate cAMPlevels, to keep the chloride CFTRchannels open in the crypt enterocytes, and hence to trigger a watery diarrhea.
Symptoms: bloody diarrhea, hemolytic uremic syndrome.
Certain strains: These contain Shiga toxins with an A:B5 format, where once internalized after one of the five binding units is taken in, the active unit is split and one component acts as an enzyme to then shut down ribosomal function. The appearance of schistocytesin the peripheral smear and inflammation affecting glomeruli and other vessels indicates the presence of endothelial damage and triggering of a microangiopathichemolytic anemia. Dialysis may be necessary as part of the supportive treatment.
requires supportive care, no antibiotics (if antibiotics quinolone for one strain)
what is it?
what is the pathogen category? normal colonic flora? virulence factors? clinical? immune response? treatment and/or prevention? describe how it works in general and the particular strains that cause damage
TheEnterobacteriaceaeare a family of Gram-negative rods well-represented among pathogenic flora, including Escherichia, Salmonella, and others, often with many strains with different pathogenic features. As an example, two major strains of Escherichia coli are enterotoxigenicand enterohemorrhagicE. coli.
Escherichia coli
Pathogen category: G-rod, aerobic, extracellular
Source: normal colonic flora
Virulence factors: capsule, flagellae, pili
Clinical: UTIs, bacteremia from nosocomial exposure, neonatal meningitis
Immune response: Igsto surface features, neutrophils
Treatment and/or prevention:depends on local resistance patterns; oral quinolone
EnterotoxogenicE. coli(ETEC): traveler’s diarrhea. The ETEC toxin works similar to the cholera toxin to activate adenylyl cyclase to elevate cAMPlevels, to keep the chloride CFTRchannels open in the crypt enterocytes, and hence to trigger a watery diarrhea. would treat w/ quinolone
Enterohemorrhagic E. coli (EHEC): the infamous O157:H7strain and others, with bloody diarrhea and risk of hemolytic uremic syndrome. These contain Shiga toxins (commonly due to meat recall) with an A:B5 format, where once internalized after one of the five binding units is taken in, the active unit is split and one component acts as an enzyme to then shut down ribosomal function. The appearance of schistocytesin the peripheral smear and inflammation affecting glomeruli and other vessels indicates the presence of endothelial damage and triggering of a microangiopathichemolytic anemia, sticking up from platelet clumps and act to cut up RBCs or shystocytes. triggering fibrin conduction. very impacting in the kidney hemolytic niuremic syndrome. dont treat w/ antibiotics because you dont want the bacteria to burst more. Dialysis may be necessary as part of the supportive treatment.
Generally speaking, E. coli-induced diarrheas require supportive treatment, not antibiotics. With EHEC, antibiotic treatment may lead to more release of the toxin asthe bacteria die in a lytic fashion.

acute but typically self-limited diarrhea with vomiting; antibiotics are not helpful in mild cases; fluoroquinolones if severe, with azithromycin as second line. gram - rod.
- motile and pathogenic with capsule
- sensitive to stomach acid, hence requiring a large number of ingested bacteria to cause infection
this develops into rose spots ,inflammation, diarrhea (blood, urine, feces)
what is it?
what is the pathogen category? normal colonic flora? virulence factors? clinical? immune response? treatment and/or prevention? describe how it works in general and the particular strains that cause damage
Salmonellaenterica(many serotypes)
Pathogen category: G-rod, aerobic, intracellular
Source: zoonotic transmission; contaminated food products
Virulence factors: antigenic variation, capsule (escapes peyers patch by this), bacterial-mediatedendocytosis
Clinical: salmonellosis, typically gastritis,but can be systemic and typhoidal
Immune response: stomach acidpreventative, neutrophils generate an inflammatory response, T cell-mediated immunity for clearance, Igs
Treatment and/or prevention:typhoidvaccine (not fully effective); ciprofloxacin for gastroenteritis if needed
Salmonellaentericaconsists of many serotypeswell, with a major distinction between typhoid and others. General features of interest include: enters via endocytosis taken up by peyers patch if not caught there can circulate around and cause typhoid fever.
- Gram negative rod, member of the Enterobacteriaceae
- motile and pathogenic with capsule
- sensitive to stomach acid, hence requiring a large number of ingested bacteria to cause infection
- acute but typically self-limited diarrhea with vomiting; antibiotics are not helpful in mild cases; fluoroquinolones if severe, with azithromycin as second line (Sanford Guide).
typhoid fever:
Salmonella enterica subtype typhi: the serotype responsible for typhoid feveris taken up by macrophages to spread throughout the body, with significant systemic signs and symptoms. There are only human carriers for S.typhi, which is particularly associated with gallbladder carriage, e.g., Mary Mallon- cook in 20th century.
Local inflammation and maculopapularrose spots(that represent bacterial embolization) may appear in 50% of typhoid patients as part of that systemicspread.
Typhoid is treatable with ciprofloxacin (except if Asia-acquired, in which caseceftriaxone, azithromycin or chloramphenicol are options. Available vaccines do not give full protection.
transmural infection or inflammation occuring in the mucosa, submucosa, and other layers of the guts hemorrhaging.
rose spots- embolization of the infetion creating spots on the body
invasion of the galbladder- having bacterial shed from the gut not a lot of white cells and can be sanctuary reservoir. common in places w/ bad sanitation due to sheeting of fecal stage

disease with fever and headache prodrome, followed by cramping and bloody diarrhea. gram - rod poultry and beef reservoir
illness can be associated with Guillain-Barrésyndrome, with ganglioside-like components of its LPS triggering autoantibodies against myelin. gram - rod poultry and beef reservoir
what is it?
what is the pathogen category? normal colonic flora? virulence factors? clinical? immune response? treatment and/or prevention? describe how it works in general and the particular strains that cause damage
Campylobacter jejuni
Pathogen category: G-curved rod, microaerophilic, extracellular
Source: zoonotic transmission; contaminated food products
Virulence factors: antigenic variation and motility with flagella
Clinical: dysentery; post infection reactive arthritis, Guillain-Barrésyndrome
Immune response: inflammatory response, Igsand cell-mediated immunity subsequent to infection
Treatment and/or prevention:azithromycin
Campylobacter jejuniis another common cause of inflammatory diarrhea/dysentery. Features of interest:
- Gram-negative curved rod (“gull-wing” pattern), microaerophilic-low O2 environment, treatable with macrolides, truncated villi triggering inflammatory environemnt in the small intestine getting bloody and watery diarrhea to dysentery.
- poultry and beef reservoirs
- disease with fever and headache prodrome, followed by cramping and bloody diarrhea (note the intestinal invasion in the image)
- illness can be associated with Guillain-Barrésyndrome, (percentage of people w/ this conditoin have some kind of infection due to cross reaction) with ganglioside-like components of its LPS triggering autoantibodies against myelin

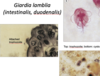
a patient ate not fully cooked seafood. after several hours to days they developed watery and tinge of blood diarrhea painless watery diarrhea with some fever
another similar strain a patient ingests freshwater producing painlesss watery diarrhea can lead to death from dehydration
what is it?
what is the pathogen category? normal colonic flora? virulence factors? clinical? immune response? treatment and/or prevention? describe how it works in general and the particular strains that cause damage

Vibrio parahaemolyticus
Pathogen category: G-curved rod, aerobic, extracellular
Source: free-livingin salt water
Virulence factors: abilityto penetrate into intestinal mucosa, enterotoxin
Clinical: gastroenteritis followingcontaminated seafood ingestion
Immune response: stomach acid kills it; inflammatory response to enterotoxin, Igsonce infected
Treatment and/or prevention:symptomatic treatment with fluid and electrolytereplenishment, as it is a self-limited infection
Epidemiology:45,000 cases/year;
Timing: 24 hour incubation, 1-7 day duration;
Vibrio parahaemolyticusalso causes a watery diarrhea. Therecan be fever and some bloodiness to it, as V.parahaemolyticuscan be invasive, as compared to cholera.
Vibrio cholerae
Pathogen category: G-curved rod, aerobic, extracellular
Source: human reservoir, can exist in fresh water
Virulence factors: adhesion to intestinal epithelium, flagella for motility for spreading; cholera- toxin driven
Clinical: cholera
Immune response: stomach acid kills it; Igsonce infected
Treatment and/or prevention:rehydration; doxycycline or azithromycin
Epidemiology:1.3 to 4 million cases/year; with estimated range of 20,000-140,000 deaths/year; https://www.who.int/en/news-room/fact-sheets/detail/cholera
Timing:0.5 to 5 days incubation, can kill within hours without rehydration; WHO
Vibrio cholerae: a Gram-negative curved, flagellated rod. acid sensitive require large dose for it to occur. The choleraexotoxin greatly increases enterocyte secretion via irreversible activation of adenylyl cyclase and subsequent high cAMP stimulation of CFTR, so a painless rice-watery diarrhea that can lead to shock and death by dehydration. key feature of treatment is rehydration (ORT- salt-sugar water combination to enhance absorptioin) doxy and zithromycin for shortening disease course and controllingw ater and sewer control.
vulnificus- working in salt water, diabetes, and wound causing infections
salt water toxin- rest can live in salt water.
vibrae- freshwater
vibriae- paralyticus eat not fully cooked seafood watery and tinge of blood diarrhea

incubation of 1 to 2 days, fever and cramps, followed by watery diarrhea that can then turn bloody. gram -. under endoscope develop white splotches
what is it?
what is the pathogen category? normal colonic flora? virulence factors? clinical? immune response? treatment and/or prevention? describe how it works in general and the particular strains that cause damage
Shigellaspecies
Pathogen category: G-rod, aerobic, intracellular
Source: human reservoir
Virulence factors: Shigatoxin; stomach acid resistance; invasion plasmid antigens
Clinical: shigellosis
Immune response: inflammatory response with neutrophils, Igssubsequent to infection
Treatment and/or prevention:ciprofloxacin
Shigellaspecies also generate a bloody diarrhea or dysentery. Features of interest:
- Gram-negative,nonmotilerods treatable with fluoroquinolones
- low dose of pathogen needed (as compared to Salmonella)
- incubation of 1 to 2 days, fever and cramps, followed by watery diarrhea that can then turn bloody (note the intestinal invasion in the colonoscopeimage).
- Shiga toxin is an AB-type toxin that inactivates ribosomal function.
- Localized battle in the peyerspatch developpingpockets of pus developing infiltrates all the way through developing
S. sonneileads to a mild disease in this country, e.g., during the summer with young children (less than 5 years old). S. dysenteriaegenerates a more severe illness in developingcountries.
may show up as right lower quadrant pain mimicing appendicitis with painfully swollen lymph nodes. watery/bloody diarrhea
what is it?
what is the pathogen category? normal colonic flora? virulence factors? clinical? immune response? treatment and/or prevention? describe how it works in general and the particular strains that cause damage
Yersinia enterocolitica
Pathogen category: G-rod, aerobic, extracellular
Source: animal reservoir;ingestion of infected cold meat, milk
Virulence factors: coldtolerance- ; YadA(Yersiniaadhesin A) binds anticomplementproteins; Yop(Yersiniaouter proteins) injected to inhibit macrophage secretion and trigger cell apoptosis
Clinical: watery/blooddiarrhea; regional adenitis
Immune response: inflammatoryresponse with neutrophils; Igsonce infected
Treatment and/or prevention:oftennone; doxycycline and gentamicin if sepsis
Epidemiology:120,000 cases/year in US; https://www.cdc.gov/yersinia/faq.html
Timing: 4-7 days after exposure; 1-3 weeks of disease; https://www.cdc.gov/yersinia/faq.html
Yersinia enterocoliticainfection, although uncommon,can mimic appendicitis, as it infects terminal ileum and mesenteric lymph nodes. Gram-negative rod, can be treated with doxycycline combined with aminoglycoside if severe (Sanford Guide).
- requires large load of bacteria to generate an infection
- cold-tolerantso can appear in contaminated, refrigerated meat or dairyproducts
- Exotoxin- kill off local immune cells not having battle at mucosa or loose connective tissue but can go to the local lymph node prolieratingto those activities.
Once at 37o, thepathogen injects Yops(Yersiniaouter proteins), which despite their name, act as exotoxins that decrease phagocytosis and other macrophage functions, allowing the pathogen to spread and proliferate in lymph nodes and have them swell painfully.

consumption of meat leading to diarrhea
what is it?
what is the pathogen category? normal colonic flora? virulence factors? clinical? immune response? treatment and/or prevention? describe how it works in general and the particular strains that cause damage
Clostridium perfringens: consumption of the spores in meat can lead to a fairly common diarrhea (as vs. a gas gangrene).

initially watery diarrhea may progress to full-blown colitis.
treat w/ metronidazole, vancomycin (high concentration to kill it off and not impacting normal gram - flora). gram + rod.
what is it?
what is the pathogen category? normal colonic flora? virulence factors? clinical? immune response? treatment and/or prevention? describe how it works in general and the particular strains that cause damage
Clostridium difficile
Pathogen category: G+rod, obligate anaerobe, extracellular
Source: gut flora, can outgrow other flora with antibiotics, nosocomial
Virulence factors:endospore formation, toxin A as enterotoxin, toxin B as cytotoxin
Clinical: pseudomembranous colitis
Immune response:normal flora
Treatment and/or prevention:metronidazole (anaeorbic specialist damaging DNA), vancomycin; fecal transplant if recurrent
Epidemiology:450,000 cases/yearin US with 30,000 deaths;
Timing: usually after 1 week of antibiotics, with abrupt onset of diarrhea
Clostridium difficilefeatures:
- Gram-positive rod, anaerobic, spore-forming, normal inhabitant of the GI tract
- implicated in antibiotic-associated diarrhea; avoid broad-spectrum antibiotics if possible
- with overgrowth, C. difficilereleases exotoxinsthat bind to and stops protein synthesis and kill enterocytes, with resulting pseudomembraneproduction
- initially watery diarrhea may progress to full-blown colitis
- spores can spread the disease; wash those hands with soap and water!
- screen feces with ELISA for toxin
Difficult to treat, with antibiotic cessation and infection control (wash hands, minimize spore spread), treatable with vancomycin as standard options, with metronidazole less popular, particularly for the severely ill or infirm. Given the challenge of C. diff infections, additional items of fidaxomicin (RNA polymerase inhibitor) as expensive alternative drug. For recurrent infection, fecal microbiota transplant (FMT) is more effective than vancomycin. Bezlotoxumab(monoclonal antibody against the B toxin) was approved by the FDA in 2016 as an agent to lessen recurrence.

triggers vomiting (rarely diarrhea) within 3-6 hours of consumption of contaminated food that is usually protein-rich
what is it? What is produced by this? How is it caused? How do you treat it and prevent spread?

Staphylococcus aureusgenerates a number of exotoxins. The one that you might be most familiar with is enterotoxin A that triggers vomiting (rarely diarrhea) within 3-6 hours of consumption of contaminated food that is usually protein-rich. Wash those hands prior to food preparation!
Thestaphylococcalenterotoxin A that generates such a rapid response acts as a superantigenwhich triggers a lot of nonspecific activity in the lamina propriaof the intestines. enhance interact w/ T cells and MHC. bursts of immune mediators in the connective tissue

Child ingests soil and dust and loves honey becomes floppy, including diplopia, dry mouth, and descending paralysis can develop respiratory distress
in adults inadequately heating canned materials w/ similar symptoms but less severe
gram + structure.
what is it?
what is the pathogen category? normal colonic flora? virulence factors? clinical? immune response? treatment and/or prevention? describe how it works in general and the particular strains that cause damage
Clostridium botulinum
Pathogen category: G+rod, obligate anaerobe, extracellular
Source: soil, contaminated food
Virulence factors:endospore formation, botulinum toxin that blocks AChrelease
Clinical: botulism with flaccid paralysis
Immune response:no immunity to toxin
Treatment and/or prevention:avoidance, human botulinumantitoxin, supportive therapy
Epidemiology:2015 Ohio outbreakof 29 with one death from potato salad made from improperly home-canned potatoes;
Timing:12-72 hour incubation; symptoms may go on for days or longer
Clostridium botulinum: botulism. The botulinum toxin that inhibits release of acetylcholine to the neuromuscularjunction by proteolytically cleaving proteins that assist with exocytosis.
- Gram positive anaerobic rod, endosporeforming, found in soil and dust
- may be seen in adults as the result of inadequate heating of canned materials to kill the toxin
- in children, spores ingested (often in honey), leading to floppy baby syndrome
- 1 to 2 day incubation, with onset of diplopia, dry mouth, and descending paralysis
- supportive treatment, e.g., ventilation and immune globulin
- antibiotics are not useful