Government Financed Health Care: Medicaid, CHIP, the VA, and the IHS Flashcards
(43 cards)
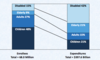
Health Insurance coverage nationally
- Quick review of current status of how Americans get health care paid for
- Does not show how much people pay out of pocket – in addition to coverage.
- For individuals, historicially Medicaid has been a bad deal
- But under the marketplace, the governemtn became kind of the group part of the plan – this was through the affordable care act
- Why do we have 7% who are uninsured? Financially, they are making a risk assessment and saying it is not worth it for them to pay for insurance

Medicaid: basic background
- Enacted in 1965 (Title XIX) as companion legislation to Medicare
- Originally focused on the welfare population:
- Single parents with dependent children
- Aged, blind, disabled
- Guarantees entitlement to individuals and federal financing to states
- Includes mandatory services and gives states options for broader coverage
- Brief hx
- Enacted with Medicare, in 1965, as addition to Social Security Act
- The greatest number of people served by what are sometimes referred to as “entitlement programs” (a government program that guarantees certain benefits to a particular group or segment of the population, also including Medicare and social security, most Veterans’ Administration programs, federal employee and military retirement plans, unemployment compensation, food stamps, and agricultural price support programs)
- Numbers served by top 10 “entitlement” programs:
- Medicaid/CHIP: 63.2 million
- Social Security: 55.8 million
- Medicare: 49.9 million
- Food stamps: 46.6 million
- Child nutrition: 35 million
- College loans: 11.3 million
- Unemployment insurance: 8.9 million
- Supplemental Security Income: 7.9 million
- Veterans compensation: 3.8 million
- Civil service retirement: 2.5 million
- What does it mean if something is an entitelemnt program? If you meet the requirement for something you will get the help from the government. For medicare, the big one is age: 65
- For Medicaid the requirement is to be poor
Medicaid: federal-state partnership
- Partnership of state and federal governments:
- Oversight by federal govt; direct management and admin by states
- Standards and requirements set by feds
- Although participation is optional, all 50 states participate in the Medicaid program.
- However, eligibility for Medicaid benefits varies widely among the states - all states must meet federal minimum requirements, but they have options for expanding Medicaid beyond the minimum federal guidelines,
- ½ to ¾ of financing comes from federal government, states pay for remainder. Depends on the Federal Medical Assistance Percentage (FMAP) - a formula that takes into account the average per capita income for each State relative to the national average. The FMAP is always at least 50%.
- States can apply for waivers from federal standards.
- Part A comes out of taxes
- Part B is a premium that you have to pay for
- Medicare is pretty much 100% federal cost (not state)
- Medicaid is a joint partnership between federal and state

The ACA modernized the Medicaid applicaiton and enrollment experience in all states
Why would the state not want this? Its administered by the state – they have to deal with the paperwork/etc.

Medicaid and the affordable care act prior to the ACA
- ACA sought to remedy some of the vast differences in who was covered by states
- Adults that weren’t taking care of children weren’t eligible

Medicaid expansion with ACA
- One of the primary mechanisms through which the ACA sought to reduce the number of uninsured Americans was through expansion of Medicaid. When the law was passed in March 2010, states were required to expand Medicaid to all adults with income up to 138% of FPL by 2014. If they did not, states would lose Medicaid funds. States were authorized to begin implementation of the expansion as early as April 2010.
- Several states sued the federal government over the expansion requirement, and in 2011 the Supreme Court held that states could not be required to accept the expansion. Rather, Medicaid expansion had to be optional for each state. As a result, 19 states have refused to expand Medicaid
- Instead of the patchwork of eligibility rules that existed around the country, there would be national standard in which anyone with income up to 138 percent of the federal poverty level could qualify.
- That expectation ended in 2012, when the Supreme Court, as part of a ruling that upheld the law’s constitutionality overall, gave each state the latitude to decide whether to participate in the ACA Medicaid expansion.
- As of now, 31 states and the District of Columbia have.
- For states that expanded Medicaid, the federal government paid 100 percent of the cost for newly eligible enrollees for the first few years, and the federal share is now ratcheting down to an eventual 90 percent.
- While some states with Republican governors have expanded Medicaid under the ACA, the Trump administration and many GOP leaders in Congress oppose it. The president has recently indicated that he supports an idea, long popular in conservative circles, that would fundamentally change Medicaid, transforming it from an entitlement (meaning that everyone who is eligible can get into the program and the government spends whatever is needed to provide its benefits) to a program of block grants, in which the government allots to each state a fixed amount of money each year and frees states from many of the program’s rules about what health services must be covered.
- Block grant proponents say that they would give states more flexibility to run their programs as they see fit; detractors say they are a smokescreen to curb federal spending and ultimately would hurt poor people.

unanticipated gap for poor in some states
- And, unfortunately, the ACA did not anticipate that some states would not expand Medicaid, and the law does not have provisions for poor people who do not qualify for Medicaid. So they are also not eligible for Market place plans and subsidies, and are thus left with no options under ACA to get health insurance coverage (in the 19 states that did not expand Medicaid, despite the fact that the federal govt paid 100% initially, and would then cover 90%, for people with up to 138% of FPL)

For which populations does medicare play a critical role?

What is Medicaids highest expense?
- Elderly and people with disabilities!
- Current estimates are that Medicaid pays for health care for more than 74.5 million people nationally.
- Those with most serious – and costly – conditions, require greater expenditures
- Disabled and elderly, are ~ ¼, but need almost 2/3 of funding for their care
Majority of medicaid expenditures
- ACUTE CARE! Not long term care
- Acute care = 2/3
Medicaid benefits - “mandatory” items and services
- •Physicians services
- •Laboratory and x-ray services
- •Inpatient hospital services
- •Outpatient hospital services
- •Early and periodic screening, diagnostic, and treatment (EPSDT) services for individuals under 21
- •Family planning and supplies
- •Federally-qualified health center (FQHC) services
- •Rural health clinic services
- •Nurse midwife services
- •Certified nurse practitioner services
- •Nursing facility (NF) services for individuals 21 or over
Medicaid benefits - “optional” items and services
- •Prescription drugs
- •Medical care or remedial care furnished by licensed practitioners
- •Diagnostic, screening, preventive, and rehab services
- •Clinic services
- •Dental services, dentures
- •Physical therapy
- •Prosthetic devices, eyeglasses
- •TB-related services
- •Primary care case management
- •ICF/MR services
- •Inpatient/nursing facility services for individuals 65 and over in an institution for mental diseases (IMD)
- •Inpatient psychiatric hospital services for individuals under age 21
- •Home health care services
- •Respiratory care services for ventilator-dependent individuals
- •Personal care services
- •Private duty nursing services
- •Hospice services
medicaid financing
- The federal government matches state Medicaid spending on an open-ended basis (the Federal Medical Assistance Percentage, FMAP)
- The current matching rate ranges from 50% to 75.65%, based on a state’s per capita income
- Enrollees who are newly eligible under health reform qualify for higher match, starting at 100% in 2014-16 and phasing down to 90% in 2020 and beyond
- ½ to ¾ of financing comes from federal government, states pay for remainder. Depends on the Federal Medical Assistance Percentage (FMAP) - a formula that takes into account the average per capita income for each State relative to the national average. The FMAP is always at least 50%.
- TEST QUESTION:
- Is this a state program or federal? BOTH!!!
Federal Medical Assitance Percentage (FMAP)
- The Federal Medical Assistance Percentage (FMAP) is computed from a formula that takes into account the average per capita income for each State relative to the national average. The FMAP cannot be less than 50%.
- The multiplier is based on the FMAP. For every dollar the state spends on Medicaid, the federal government matches at a rate that varies year to year. For example, in FY2004, the rate for Alabama was 1:2.80 (73.70%).
- FMAPs displayed here apply to the federal fiscal year indicated unless otherwise noted, which runs from October 1 through September 30. For example, FY 2018 refers to the period from October 1, 2017 through September 30, 2018.
- US federal minimum FMAP is 50%.
Is medicaid budget item or a revenue item in state budgets?
- Medicaid is both a budget item and a revenue item in state budgets.
- States receive federal dollars, and expend revenue for services to Medicaid resipients
ACA medicaid expansion to low-income adults
- 32 states cover parents and other adults with incomes up to 138% FPL ($28,676 per year for a family of three and $16,753 per year for an individual in 2018) under the ACA Medicaid expansion to low-income adults
- “…Other adults…” – not pregnant or parents with children in the household
States that have not expanded Medicaid
- In the 19 states that have not expanded Medicaid, the median eligibility limit for parents is 43% FPL ($8,935 per year for a family of three in 2018) and other adults remain ineligible, except in Wisconsin (Figure 5).
- In 11 of these states, parent eligibility is at less than half of the poverty level, and only two of these states (ME and WI) cover parents at or above poverty. Wisconsin is the only non-expansion state that provides full Medicaid coverage to other adults, although eligibility at 100% FPL remains below the expansion level and the state does not receive the enhanced match available for expansion adults for this coverage.2
- In the non-expansion states, 2.4 million adults with incomes above the Medicaid eligibility limit but below poverty fall into a coverage gap; they are ineligible for Medicaid and do not qualify for subsidies for Marketplace coverage, which become available at 100% FPL
income eligibility levels for children in Medicaid/CHIP
- As of January 2018, 49 states cover children of parents with incomes up to at least 200% of the federal poverty level (FPL, $41,560 per year for a family of three in 2018) through Medicaid and CHIP (Figure 1, Table 1and 1A).
- This count includes 19 states that cover children with incomes at or above 300% FPL.
- Only two states (ID and ND) limit children’s eligibility to below 200% FPL.
- Across states, the upper Medicaid/CHIP eligibility limit for children ranges from 175% FPL in North Dakota to 405% FPL.
INcome eligibility levels for pregnant women in medicaid/CHIP
- Most states extend coverage to pregnant women beyond the federal minimum of 138% FPL through Medicaid and CHIP.
- As of January 2018, 34 states cover pregnant women with incomes at or above 200% FPL ($41,560 per year for a family of three in 2018), including 12 states (including DC) that cover pregnant women with family incomes above 250% FPL.
- Five states extend coverage for pregnant women through CHIP and 16 states use CHIP funding to provide coverage through the unborn child option, under which states cover income-eligible pregnant women regardless of immigration status
Medicaid income eligibility levels for parents
- As of January 2018, 32 states cover parents and other adults with incomes up to 138% FPL ($28,676 per year for a family of three and $16,753 per year for an individual in 2018) under the ACA Medicaid expansion to low-income adults (Figures 3 and 4, Table 3).
- The District of Columbia extends eligibility beyond the expansion limit to parents with incomes up to 221% FPL and other adults with incomes up to 215%, and Alaska covers parents with incomes up to 139% FPL.
*
how do most beneficiaries receive care
- Most beneficiaries receive care through some type of managed care arrangement.
policy issues for medicaid
- Coverage for low-income families
- Reduces uninsured
- Improves access to care
- Per enrollee costs low
- Responds to economic downturn
- Assistance for the elderly and disabled
- Helps poorest and sickest Medicare beneficiaries
- Essential supplement to Medicare
- Primary users of prescription drugs and long-term care
- Per enrollee costs high
- Fiscal Pressure
- Pressure from declining state revenue and growing health costs
- Need to keep pace with private sector to assure access
- Most dollars in elderly/disabled and long-term care
- Fiscal tension between federal government and states
- Restructuring proposals/state flexibility
what is CHIP
- Children’s Health Insurance Program
- •Enacted in 1997
- •8.1 million children ever enrolled in FY 2013 (compare to 72 million people covered by Medicaid)
- •$13 billion ($9 billion federal and $4 billion state) in FY
- 2014 (compare to >$400 billion for Medicaid)
- •Similar state-federal partnership design
- •Can be operated as Medicaid expansion or separate program (or both)
- It is kind of a companion to Medicaid
- Higher income eligibility is a great thing!!
How does CHIP differ from Medicaid
- From the perspective of the enrollee:
- •Not an entitlement to individuals: states can establish waiting periods, waiting lists
- •Income eligibility is higher; upper limit ranges from 175% of federal poverty level (FPL) (North Dakota) to 405% FPL (New York)
- •Modeled on private insurance with options for:
- •Monthly premiums
- •Benefits may be pegged to commercial benchmark
- •Branding
- From the perspective of the state:
- •Funding is capped and allotments to states set in statute
- •Matching rate is enhanced at 65–82% (compared to Medicaid’s match of 50-74%)
- •Choice of design (Medicaid expansion, separate CHIP)





