GIT Flashcards
Cow producing 30L of milk requires how much dry matter?

Half the number of liters plus five






Tail end of the 5 station exam

Left side 5 station clinical exam

Auscultation of the rumen and left flank
Normal:
- palpate doughy rumen, often with a small gas cap
- Primary contractions approximately every minute
- Secondary cycle approximately every 2 minutes
Abnormal:
- Palpate large gas cap which distends fossa
- Hypermotility (e.g. vagus indigestion)
- Hypomotility (e.g. hypocalcaemia, rumen atony)
- ping (rumen distension)

Percuss and auscultate body wall
* Requirements for pings
- gas distended viscus
- gas/fluid interface
- gas under pressure
- gas distended viscus might be against body wall
- both percussor and stethoscope must be over gas distended viscus
- viscus is singular of viscera

Left sided pings DDX


Abomasal ping
- high pitched/ resonant
- classic location
- beware milk fever!
Rumen ping
- a bit duller
- less resonant
- dorsal location
- can often palpate the gas cap

Auscultation and ballottement

Diagnosing a ping
Abomasal ping
- high pitched/ resonant
- classic location
- beware milk fever!
Rumen ping
- a bit duller
- less resonant
- dorsal location
- can often palpate the gas cap



Right sided auscultation/ percussion

Fluid splashing sounds audible on deep ballottement (succussion)?

5 station exam right side

5 station exam head/neck

5 station exam tail end revisted steps



Abnormal rectal findings include:


Abomasal torsion
Parameters of faeces to assess alimentary tract

5 station exam ancillary tests


pH- the normal is between 6.2 and 7.2
Low values of pH are found after the feeding of carbohydrates
A value of below 5 is considered very suggestive of carbohydrate engorgement
Examination of rumen protozoa
(Could also use a stomach tube)


Measuring pH of the rumen


Paracentesis sites
- To the left of the midline, 3 to 4 cm medial to and 5 to 7 cm cranial to the foramen for the left subcutaneous vein
- 5 cm caudal to the xiphisternum and 5 cm to left or right of mid-line
- The right ventral abdominal wall in the area of the skin under the flank fold above the udder
What could air in the intestines indicate?
Blockage or hypocalcaemia


Tests for abdominal pain
* Grunt test
In the “grunt test” a sharp pressure is applied over and behind the xiphoid whilst listening for an audible grunt from the
cow. The pressure may be applied with a clenched fist, the knee or a pole lifted on both sides. The grunt is sometimes
clearly audible but is often only discerned by auscultation over the trachea. The test is rather subjective and not
particularly reliable. It should be appreciated that a grunt can be elicited from pain in either the anterior abdomen or
chest and the test is not specific for traumatic reticulo-peritonitis, although that is the most common condition associated
with a positive finding
* Withers pinch test
Firm pressure is applied to the whither area by grasping and pinching the whithers. A normal cow will lower the withers to
avoid this contact. A cow with peritonitis may be reluctant to lower her withers and thuis push against the painful
peritoneal surface. This technique requires more subjective interpretation because many nervous cows Are reluctant to
respoind at all to a withers pinch.

Abdominal pain in the bovine
* May be seen in conditions of gastro-intestinal tract such as:
- volvulus, intussusception, phytobezoars, salmonellosis
- Abomasal torsion, spasmodic colic
* But also:
- Diseases of the liver, associated with distension of the organ capsule
- inflammation of the serous surfaces of the peritoneum
- with pyelonephritis, urethral obstruction and distension of the bladder
- early cases of photosensitisation

Exploratory laparotomy

* Anaesthesia- inverted L or paravertebral (disadvantage: a lot of anaesthetic)
- clip area and prepare for surgery
* 20 cm incision right paralumbar fossa
3 steps:
- incise skin and subcutaneous/ external abdominal oblique with vertical incision
- split internal abdominal oblique in direction of fibres
- blunt dissect through transverse abdominous, peritoneum





Exploratory laparotomy- closure

Diseases of the abomasum and intestines

Left Displaced Abomasum (LDA)
Aetiology not fully understood, multifactorial syndrome, heavy grain feeding

Aetiology of LDA

Nutritional factors implicated in LDA

LDA correction

LDA correction- right flank omentopexy

* ID pylorus- pull on omental attachment until the pylorus comes into view- palpate and visualise
* Routine closure
* Broad spectrums abs (Oxytet)
* NSAIDs (long acting- tolfedine or metacam)
* Ketol

LDA correction- rolling

LDA correction- toggle technique

Prevention of LDA

Key Points of LDA



RDA/RTA typical history and clinical signs

Aetiology of RDA



Abomasal dilatation and torsion

Abomasal dilatation and torsion- correction
* First assess prognosis- melena and HR > 100 are bad signs when corrected, omentopexy to prevent recurrence
* Standard closure
* IV fluids if very shocked
* Antibiotics
* NSAIDs

RDA Key points

Dietary abomasal impaction
Dietary abomasal impaction treatment

Typical history of physical obstruction of the pylorus

Typical signs of intestinal phytobezoars
Physical obstruction of the pylorus treatment

Intestinal phytobezoars

* Signs are less severe than seen in cattle suffering from an obstruction due to a volvulus or intussusception
* Findings
- sudden severe depression in milk yield
- dehydration
- commonly a very small amount of greenish rumen discharge observed at nares of affected animals
- ballottement/auscultation right abdomen- may detect fluid splashing sounds
- rectal exam: early stages the amount of faeces is reduced and somewhat pasty… later, grey, yellow faeces- extremely pasty, very foul smell- pathognomonic
** As condition progresses- dehydration increases, HR increases

Intestinal phytobezoars- treatment?

* right paralumbar approach
careful search of intestines - palpation

Key points- intestinal phytobezoar

Intussusception


Intussusception surgery

Key points intussusception

Intestinal torsion


Dilatation, volvulus and torsion of the caecum

Dilation and torsion of the caecum- signs

Dilatation and torsion of the caecum- treatment

Caecal dilatation, volvulus and torsion

Carb overload, two conditions

History of acute rumen acidosis
Pathogenesis of acute rumen acidosis

Rumen acidosis



Acute rumen acidosis secondary effects





Diagnosis of acute rumen acidosis

Four stages of acidosis Treatment
- Cow has above + some systemic effects
- as above plus antibiotics
- avoid secondary effects - Cow is down
- as above plus NSAIDs, fluids
- ? how much fluids and what type
- consider rumenotomy
- careful of water

Rumen buffers

Ancillary treatments of ruminal acidosis

What is sub acute rumen acidosis?
* herd problem due to diet
* reduced rumenation (cud chewing)
* mild diarrhoea
* foamy faeces containing gas bubbles
* undigested grain in faeces
* Reduced milk fat (<3%)

Indirect indicators of ruminal acidosis
* laminitis
* faeces

Faeces indicators of fibre intake

Laminitis and grain

SARA treatment

Prevention of rumen acidosis

Buffers in feed
More than 4 kg a day need buffers in the feed
bicarb 2-3% to the grain

Virginiamycin
Concern with ab resistant bacteria however works really well with rumen acidosis
Takes a fortnight to work and need veterinary prescription
Produce medicated feed orders (like prescription) send into feedmill and the feedmill adds the Virginiamycin


Carb engorgement conditions

Other rumen upsets aside from carb engorgement

Treatment of abdominal conditions






Acidosis or alkalosis

Fluid therapy in adult cattle
* only bother to treat severe dehydration in most cows, if they are down need to correct if for them otherwise they will correct it orally themselves
* Most cows are alkalotic
* At a farm visit, can really only give 5-6 liters of IV fluid at once
* A practical method of treatment is 2-3 L of hypertonic saline (4 ml/kg BW) IV (over about 4 minutes) plus 20 L of water administered by stomach tube
* Can add some bicarbonate in grain overload cows
* Be careful of hypertonic fluids in very dehydrated cows (as distinct from endotoxic shock)
* MUST follow up with oral fluids (Water is ok)

Define abdominal distension? Bloat?

Abdominal distension- principles?

What does a ping mean?

Left abdominal distension

Bilateral abdominal distension

Trilateral abdominal distension

Abdominal distension left– mechanisms?

Abdominal distension- diseases

Bloat





Frothy bloat

Drenching cows with bloat

Other option aside from drenching for cows with bloat?

Drenching, tubing, or?? cow with bloat?
* the hole sometimes blocks up
* you only need to let enough gas out so that the cow can breathe again
* drench her with bloat oil then

Emergency rumenotomy

When does bloat occur?

Prevention of bloat

Diet to prevent bloat

Oils to prevent bloat

Detergents to prevent bloat

Monensin
* often added to the grain ration fed to dairy cattle
- increases proprionic acid production
- prevents coccidosis in young stock
* Very toxic for horses
* Typically occurs in feed at 11-18 mg/kg (dairy) or 25-33 mg/kg (beef)
* Horses 20 times more sensitive than cattle (200x more than chooks)
* Heart and skeletal muscle death from mitochondrial dysfunction

Abdominal distension- diseases

Free gas bloat acute or chronic
* ANY recumbency
* Oesophageal obstruction
* Hypocalcaemia
* Stop them dying of bloat
* Treat the underlying condition

Oesophageal obstruction
Buscopan

Chronic secondary bloat

Simple indigestion

Simple indigestion aetiology? Clinical findings? Diagnosis? Treatment?

Vagus indigestion

Vagus nerve


Diagnosis of vagus indigestion


Treatment of vagal indigestion

Abs for peritonitis

Anti-inflammatories of vagal indigestion

Post mortem bloat

Abdominal distension- right


Needle head placed in to check if fluid comes out



Abomasal volvulus

Hydrops amnion and allantois

DDX to hydrops amnion and allantois

Abdominal distension- left

Abdominal distension-right?

Abomasal ulceration

Incidence of abomasal ulcers

history of abomasal ulcers? typical clinical signs?
Ulceration of the abomasum when severe?


Key points abomasal ulceration

Peritonitis

Traumatic reticuloperitonitis

Presentation traumatic reticuloperitonitis


Ruminant digestive system
Ruminants grasp mouthfuls of food and swallow before it is chewed, wrap their tongues around a mouthful of grass, clamp down their teeth and pull to break the grass at its weakest point and swallow
* Ruminants will chew their cud (regurg) their food material and then grind it with their molars at a time when the animal is resting
* this is done until the food particles are small enough to pass through the reticulum into the rumen
* Since ruminants do not chew their food when it is taken in, at times foreign material like rocks, nails, small pieces of wire can be swallowed
* While the animal is chewing its cud foreign particles that are heavy sink in the reticulum, preventing many foreign particles from entering the rest of the digestive system
* Once foreign material enters the reticulum, it can stay there for the life of the animal
* If the reticulum squeezes a piece of wire it may penetrate through into the chest/ heart
Sequelae to traumatic reticuloperitonitis

Treatment of traumatic reticuloperitonitis

Prevention of traumatic reticuloperitonitis

Secondary rumen atony

Key points of abdominal distension and bloat

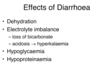
Pathophysiology of Diarrhoea

Effects of diarrhoea
Lists of diseases with diarrhoea

Aetiology of diarrhoea
BVDV

Acute disease in naive animals

In utero infection BVDV
* 100-150 days
- viral damage to developing organs: especially CNS
- may be PI or have high Ab levels
* > 150 days
- usually no clinical effect
- virus free
- seroconverted to pestivirus

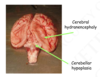
Congenital defects BVDV


BVDV
Mucosal disease in PI animals (BVDV)
* Acute or chronic forms
* usually in younger animals
* 100% fatal but low numbers affected

Less typical presentations of BVDV

Epi of BVDV
Laboratory diagnosis BVDV

Control of BVDV

Salmonellosis

Epi of S. dublin

Epi of S. Typhimurium

Local Epi of BVDV

Clinical presentation of BVDV
* Acute enteritis
- anorexia, reduced milk production, pyrexia, depression
- profuse, putrid diarrhoea +/- dysentery
- Abdominal pain
- dehydration, recumbency, death
* Abortion may occur subsequently

Zoonotic BVDV

Diagnosis of BVDV

Treatment of BVDV
* Supportive therapy: fluids– oral supplemented with electrolytes, IV for acidosis (NaCl/ H2CO3)

Short term control of BVDV

Yersiniosis

Pathogenesis of Yersiniosis

Clinical signs of Yersiniosis

Diagnosis of Yersiniosis
JD
Prevalence of JD
Importance of JD

Epi of JD
* preclinical
Clinical signs of JD

JD

JD Lab tests

More tests JD

Combination of tests for JD

Treatment of JD

Control of JD
* If you have got JD in your herd…
- prevent spread
– detect infected adults and remove them
– manage calves to reduce exposure (JDCAP)
- reduce exposure to adult faeces; vaccinate
* Minimize the risk of further introduction
- don’t introduce animals into the herd
- source introduced animals from low risk herds (JDMAP)

National JD control program
BJD Zoning

JD MAP

JD CAP

JD CAP

Fibre requirements in the diet?
Adequate intake of neutral detergent fibre (NDF)– 25% NDF in total dietary DM. 75% of which is supplied by coarse forage to maintain rumen function and health.
* Many pasture diets, especially those supplemented with concentrates, will be near the lower limit of effective fibre required in the diet.
* Estimates of diet NDF should be matched with observations from the field cud-chewing, faecal formation, milk fat and protein content and rumen pH to ensure optimal and safe diet
How are the volatile fatty acids absorbed to buffer the acid in the rumen?
Absorbed through the rumen wall (papillae)
Cow produces huge amounts of bicarbonate in her saliva– enough roughage and food with sufficient particle length that the cow is going to need to regurgitate and chew it

Could cause if an abscess burst and causes local peritonitis–> LDA, RDA, vagal indigestion
* Predisposing factor carb overload in the first part of lactation

Undigested grain

Caval syndrome

Saw horse stance due to laminitis


Parasite mechanisms of survival

Effects of parasites

Most common nematodes in Australia
Ostertagia
* Most pathogenic nematode
aka Teladorsagia
Small up to 9 mm
Outbreaks– Type I and Type II
Abomasum

Trichostrongylus axei

Haemonchus

Cooperia

General life cycle of the nematode

Length of life cycle

Timing of dung pat and larval migration

Dung pats and nematodes

Larval migration

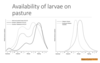
Timing of Population % of eggs deposited

Timing of availability of larvae on pasture
When do calves have eggs in their faeces? When are they first drenched?


Type I Ostertagiasis?
When is high risk time of weaned calves?



Immunity and hypobiosis in yearlings and older beef cattle?

Type II Ostertagiasis

Seasonal occurrence of adult worms and inhibited larvae of O. ostertagi in different temperate zone regions of AUS

Drenching who beef?

Dairy calves and parasites?
* Grazing dairy cattle likely to be infected with nematodes
* 80% trials showed a positive response to anthelmintics
* Median increase 0.67 litres/day
* There is no way of determining whether an animal or herd has a sufficient parasite burden to interfere with production

Diagnosis of nematodiasis

Faecal egg counts




Plasma pepsinogen

Bulk Milk ELISA

Toxocariasis

Intestinal cestodes
Cysticercosis
◦
Taenia saginata (Cysticercus bovis)
Echinococcus granulosis
◦
The
most
common
cause
of
downgrades
in
QLD
abbattoirs
◦
Notifiable
◦
NZ
is
hydatid free
(?
Tasmania
too)
Coenurosis cerebralis (Taenia multiceps)

Who does Fasciola hepatica affect?

Liver fluke effects

Fasciola hepatica life cycle
IH hosts
Lymnea tomentosa (native)
L columella
Both live in (L. columellla) and around (L. tomentosa) bodies of water

Pathogenesis of Fasciola hepatica

Acute Fluke Disease


Chronic Fasciola hepatica


Fluke diagnosis
* Antibody ELISA
- Sensitivity of 87.5% reported
* Detects non-patent infections (from 14 d)
* Blood, milk, or bulk milk
* Useful as a screening test for a group of animals
** Post mortem as well– flukes or scarring

Treatment/ Prognosis of Fasciola hepatica

Treatement and control of Fasciola hepatica

Lungworm

Lungworm life cycle


Lungworm infection in a group of weaned calves: note the open-mouth breathing in one animal and loss of condition through the entire group

Field post-mortem examination of a calf with lungworm infection; the airways are characteristically full of a bloody froth and many adult worms are present
Lungworm diagnosis

Treatment of parasites

Types of anthelmintics

White drenches

Clear drenches

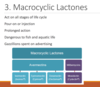
Macrocyclic lactones
Choosing a drench– factors

Which product?

Control of parasitic gastroenteritis

Withholding periods

When to drench dairy calves
* depends who you ask
* Standard recommendation- drench at calving
* drying off?
* Calving?
* Probably not a critical decision

When to worm beef cattle

Drench resistance


Managing AR on dairy farms


How to apply refugia on dairy farms

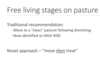
Free living stages on pasture


Pour ons

combo anthelmintics
Quarantine testing

Mgt of resistance

What is the best drench for calves?
Injectable Dectomax
Times where it makes a difference is if you have a problem


