Female Reproductive System and Breast II Flashcards
The “three D’s” of endometriosis are dysmenorrhea, […], and dyschezia.

The “three D’s” of endometriosis are dysmenorrhea, deep dyspareunia, and dyschezia.
other possible symptoms include chronic pelvic pain and infertility (resection of endometriosis improves conception rates)

The “three D’s” of endometriosis are dysmenorrhea, deep dyspareunia, and […].

The “three D’s” of endometriosis are dysmenorrhea, deep dyspareunia, and dyschezia.
other possible symptoms include chronic pelvic pain and infertility (resection of endometriosis improves conception rates)

The absence of bleeding following a progestin withdrawal challenge may be indicative of low […] levels.
The absence of bleeding following a progestin withdrawal challenge may be indicative of low estrogen levels.
normally estrogen causes the endometrium to proliferate, which sloughs following withdrawal of progesterone; absence of withdrawal bleeding can also occur with inadequate endometrial lining (e.g. Asherman’s syndrome)
The diagnosis of a palpable breast mass can only be confirmed with a […].
The diagnosis of a palpable breast mass can only be confirmed with a biopsy.
e.g. fine needle aspiration or core needle biopsy

The gold standard for diagnosis of ovarian torsion is ultrasound, which typically reveals an ovarian mass with absent […].

The gold standard for diagnosis of ovarian torsion is ultrasound, which typically reveals an ovarian mass with absent Doppler flow.
The gross appearance of inflammatory breast cancer is often described as resembling an […].
The gross appearance of inflammatory breast cancer is often described as resembling an orange peel (Peau d’orange).
due to invasion of lymphatic spaces

The HPV vaccine is typically administered beginning at age 11 - 12 and can be received until age […].
The HPV vaccine is typically administered beginning at age 11 - 12 and can be received until age 26.
recommended for all girls and women age 11-26, regardless of HPV status; boys & men can receive the vaccine between ages 9 - 21 (up to 26 for HIV+ patients)

The main function of hCG during pregnancy is to maintain the […].
The main function of hCG during pregnancy is to maintain the corpus luteum.
hCG is secreted by syncytiotrophoblasts and peaks between 6-10 weeks; necessary to maintain progesterone secretion until the placenta is able to produce progesterone on its own

The most common cause of physiologic galactorrhea is […].
The most common cause of physiologic galactorrhea is hyperprolactinemia.

The most significant risk factors for vaginal squamous cell carcinoma are […] and […].
The most significant risk factors for vaginal squamous cell carcinoma are smoking and HPV infection.
similar to the risk factors for cervical cancer

The pathogenesis of hypogonadotropic hypogonadism involves loss of […] secretion.
The pathogenesis of hypogonadotropic hypogonadism involves loss of pulsatile GnRH secretion.

The pathophysiology of bacterial vaginosis involves decreased colonization of the vagina with […], leading to increased pH and overgrowth of anaerobic bacteria.
The pathophysiology of bacterial vaginosis involves decreased colonization of the vagina with lactobacilli, leading to increased pH and overgrowth of anaerobic bacteria.
e.g. Gardnerella vaginalis

The risk of developing breast cancer is directly correlated with lifetime exposure to […].
The risk of developing breast cancer is directly correlated with lifetime exposure to estrogen.
e.g. increased risk with nulliparity, early menarche, late menopause, obesity, etc.

The risk of endometrial hyperplasia/cancer is directly related to unopposed […] exposure.
The risk of endometrial hyperplasia/cancer is directly related to unopposed estrogen exposure.
risk factors mnemonic “HONDA”: Hypertension, Obesity, Nulliparity, Diabetes mellitus, Age (increased)

The size/tenderness of fibroadenomas and breast cysts increase with exposure to […].
The size/tenderness of fibroadenomas and breast cysts increase with exposure to estrogen.
e.g. with pregnancy, prior to menstruation

Treatment of small genital warts includes topical medications, such as […] or podophyllin resin.
Treatment of small genital warts includes topical medications, such as trichloroacetic acid or podophyllin resin.
larger lesions may require surgical removal; podophyillin resin is contraindicated during pregnancy

Treatment of small genital warts includes topical medications, such as trichloroacetic acid or […].
Treatment of small genital warts includes topical medications, such as trichloroacetic acid or podophyllin resin.
larger lesions may require surgical removal; podophyillin resin is contraindicated during pregnancy

Ultrasound findings consistent with epithelial ovarian carcinoma include a solid mass with thick septations and the presence of […].
Ultrasound findings consistent with epithelial ovarian carcinoma include a solid mass with thick septations and the presence of ascites.

Uterine […] is a form of pelvic organ prolapse in which the entire uterus herniates through the vagina along with the anterior and posterior vaginal walls.
Uterine procidentia is a form of pelvic organ prolapse in which the entire uterus herniates through the vagina along with the anterior and posterior vaginal walls.

Very elevated levels of […] is characteristic of menopause.
Very elevated levels of FSH is characteristic of menopause.
due to loss of negative feedback on FSH due to decreased estrogen

What cancer(s) are associated with atypical glandular cells on Pap testing?
cervical and endometrial adenocarcinoma
thus presence of AGCs warrants evaluation of the ectocervix, endocervix, and endometrium

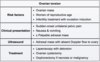
What cause of vaginitis is characterized by a green, malodorous, frothy discharge and vaginal inflammation?
Trichomoniasis (Trichomonas vaginalis infection)
some cases may also present with punctate hemorrhages on the cervix (“strawberry cervix”)

What cause of vaginitis is characterized by a positive amine whiff test?
Bacterial vaginosis
i.e. the presence of an amine (fishy) odor with the addition of potassium hydroxide

What cause of vaginitis is characterized by a thick, white discharge and vaginal inflammation?
Candida vaginitis (Candida albicans infection)

also typically presents with vaginal pruritus, which may be apparent on physical exam as vulvar erythema and excoriations
What cause of vaginitis is characterized by a thin, white discharge with a fishy odor and no vaginal inflammation?
Bacterial vaginosis (Gardnerella vaginalis infection)

What is the best long-term management for stress urinary incontinence due to urethral hypermobility?
Urethral sling surgery

What is the definitive treatment for endometriosis?
Hysterectomy and oophorectomy
typically done in symptomatic women who have completed childbearing

What is the definitive treatment for pregnant patients with HELLP syndrome?
Delivery
delivery should occur at > 34 weeks gestation or with deteriorating maternal/fetal status; antihypertensive medications and/or magnesium may be needed for stabilization

What is the effect of low estrogen levels on vaginal pH?
Increased pH (> 5)
thus increased pH with normal urinalysis may indicate a hypoestrogenic state (e.g. atrophic vaginitis)

What is the extent of epithelial involvement by immature dysplastic cells in CIN I?
less than 1/3
low-grade CIN; high-grade CIN involves > 1/3 epithelium and includes CIN II and III

What is the first-line pharmacologic treatment for infertility due to polycystic ovarian syndrome?
Clomiphene citrate
primarily blocks estrogen receptors at the hypothalamus, inhibiting the negative feedback mechanism and restoring pulsatile release of GnRH

What is the first-line pharmacologic treatment for menstrual irregularity due to polycystic ovarian syndrome?
Oral contraceptives

What is the first-line test/imaging study to evaluate infertility in a patient with a history of pelvic inflammatory disease?
hysterosalpingogram
minimally invasive way to detect fallopian tube patency and/or uterine cavity anomalies

What is the first-line treatment for infertility or menstrual irregularities due to polycystic ovarian syndrome?
Weight loss
helps restory ovulatory cycles

What is the first-line treatment for premenstrual syndrome (PMS)?
SSRIs

What is the first-line treatment for primary dysmenorrhea?
NSAIDs and/or hormonal contraception
treatment preference depends if the patient is sexually active (OCPs) or sexually inactive (NSAIDs)

What is the first-line treatment for stress urinary incontinence due to urethral hypermobility?
Pelvic muscle exercises (e.g. Kegel exercises)

What is the first-line treatment for vulvar lichen sclerosus?
High-potency topical corticosteroids (e.g. clobetasol)
helps provide relief from itching and dyspareunia

What is the gold standard diagnostic test for acute cervicitis?
Nucleic acid amplification testing (NAAT)
has a high sensitivity/specificity for Chlamydia trachomatis and Neisseria gonorrhoeae, which are the most common causes of acute cervicitis

What is the gold standard method for diagnosis of cervical intraepithelial neoplasia (CIN)?
Colposcopy
acetic acid is used to help visualize abnormal cervical tissue (e.g. aceto-white changes)

What is the gold standard test for male factor infertility?
Semen analysis
evaluates sperm concentration, motility, and morphology; male infertility occurs in as many as 25% of cases
What is the initial management for mild atrophic vaginitis?
Vaginal moisturizer and lubricant

What is the initial test/imaging study for a women age < 30 with a palpable breast mass?
Ultrasound
helps differentiate a cystic lesion versus a solid lesion; mammogram is not as useful due to increased breast tissue density in younger women

What is the initial test/imaging study for a women age > 30 with a palpable breast mass?
Mammogram
ultrasound may be added for better characterization of the mass; tissue biopsy is needed to confirm the diagnosis

What is the likely diagnosis in a 35-year-old woman that presents with infertility, irregular menses, and hot flashes?
Primary ovarian insufficiency
i.e. cessation of ovarian function before 40 years of age

What is the likely diagnosis in a 38-year-old woman that presents with infertility despite a regular menstrual cycle and normal physical exam?
Decreased ovarian reserve
characterized by decreased oocyte number and quality; sharp decline in conception is notable after age 35

What is the likely diagnosis in a 6-month postpartum woman that presents with irregular vaginal bleeding, an enlarged uterus, and dyspnea with multiple infiltrates on CXR?
Choriocarcinoma
classically occurs after a complete hydatidiform mole, but can occur after normal pregnancy or spontaneous abortion

What is the likely diagnosis in a breastfeeding woman that presents with fever and localized breast erythema/tenderness with a palpable, fluctuant mass on physical exam?
Breast abscess
persistent mastitis can result in a collection of pus, thus causing an abscess

What is the likely diagnosis in a female athlete that presents with amenorrhea and decreased FSH, LH, and estrogen on laboratory exam?
Hypogonadotropic hypogonadism (hypothalamic amenorrhea)
symptoms related to loss of pulsatile GnRH secretion precipitated by weight loss, stress, or chronic illness

What is the likely diagnosis in a morbidly obese woman that presents with amenorrhea and normal pituitary hormone levels (e.g. FSH, LH, prolactin)?
Anovulation
anovulation occurs due to decreased progesterone production (secondary to the effects of hyperinsulinemia, insulin resistance, and hyperandrogenism on steroidogenesis)
What is the likely diagnosis in a patient that presents with foul-smelling brown discharge from the posterior vaginal wall two weeks after a vaginal delivery complicated by third-degree laceration?
Rectovaginal fistula
red, velvety rectal mucosa may be visualized on the posterior vaginal wall
What is the likely diagnosis in a patient that presents with pelvic pressure and voiding dysfunction one year after a hysterectomy? Pelvic examination reveals a protruding vaginal mass, especially with the Valsalva maneuver.
Pelvic organ prolapse
due to herniation of pelvic organs (e.g. bladder, uterus, rectum) through the vagina; risk factors include obesity, multiparity, and hysterectomy

What is the likely diagnosis in a patient that presents with sudden-onset unilateral pelvic pain with an enlarged, edematous ovary on ultrasound? Pregnancy test is negative.
Ovarian torsion
absence of free pelvic fluid helps differentiate ovarian torsion from a ruptured cyst

What is the likely diagnosis in a patient that presents with sudden-onset unilateral pelvic pain with free fluid in the pelvis on ultrasound? Pregnancy test is negative.
Ruptured ovarian cyst
free pelvic fluid helps differentiate a ruptured cyst from ovarian torsion (enlarged, edematous ovaries on ultrasound)

What is the likely diagnosis in a patient with crampy abdominal/back pain during the first few days of menses with a normal physical examination?
Primary dysmenorrhea
due to release of prostaglandins; timing of pain helps differentiate from endometriosis, which typically peaks just prior to menstruation

What is the likely diagnosis in a patient with fever, hypotension, and a macular rash involving the palms/soles? The patient’s last menstrual period was 3 days ago.
Staphylococcal toxic shock syndrome
likely due to prolonged tampon use, which causes a systemic inflammatory response to toxic shock syndrome toxin-1, an exotoxin that acts as a superantigen

What is the likely diagnosis in a patient with primary amenorrhea and the following physical exam: absent uterus/upper vagina and normal ovaries, pubic hair, breast development.
Mullerian agenesis
characterized by no upper vagina, cervix, or uterus but otherwise normal female development

What is the likely diagnosis in a patient with primary amenorrhea and the following physical exam: absent uterus/upper vagina, minimal pubic hair, and normal lower vagina, breast development.
Androgen insensitivity syndrome
patient’s are 46,XY and have normal testicular secretion of anti-Mullerian hormone (absent cervix, uterus, upper vagina) and testosterone (converted to estrogen for breast development)

What is the likely diagnosis in a post-menopausal woman that presents with chronic pelvic pain and a solid ovarian mass with thick septations and ascites on ultrasound?
Epithelial ovarian carcinoma
due to abnormal proliferation of ovarian or tubal epithelium or peritoneum; may also present with bloating and/or early satiety

What is the likely diagnosis in a postmenopausal woman that presents with breast tenderness and vaginal bleeding with a large adnexal mass on ultrasound?
Granulosa cell tumor
symptoms are due to estrogen secretion; may cause prococious puberty in children

What is the likely diagnosis in a postmenopausal woman that presents with vaginal pruritus/dryness, dysuria, and increased urinary frequency? Urinalysis is normal.
Atrophic vaginitis (genitourinary syndrome of menopause)
due to reduced estrogen support after menopause; urinary symptoms can mimic UTI therefore urinalysis and urine culture are needed to rule out concurrent infection

What is the likely diagnosis in a postmenopausal woman that presents with vulvar itching and thin, dry, white plaque-like vulvar skin?

Lichen sclerosus
skin is classically described as “cigarette paper” quality and patient’s may have retraction of normal anatomical landmarks (e.g. clitoral retraction); does NOT affect the vaginal mucosa, which is an important distinguishing feature from atrophic vaginitis

What is the likely diagnosis in a postmenopausal woman with a painful, eczematous, pruritic rash on the nipple/areola refractory to corticosteroids?
Mammary paget disease

What is the likely diagnosis in a premenopausal woman that presents with adnexal fullness and an ovarian cyst with calcifications and hyperechoic nodules on ultrasound?
Dermoid ovarian cyst (mature cystic teratoma)
common benign ovarian tumor in premenopausal women; may contain sebacious materal with epithelial components (e.g. hair, teeth)

What is the likely diagnosis in a premenopausal woman that presents with dyspareunia and dry vaginal mucosa? The patient’s history is significant for chronic dry eyes/mouth.
Sjogren syndrome
extraglandular features include arthritis, Raynaud phenomenon, cutaneous vasculitis, and non-Hodgkin lymphoma

What is the likely diagnosis in a premenopausal woman that presents with unilateral bloody nipple discharge with no palpable breast mass or lymphadenopathy?
Intraductal papilloma
papillary tumor affecting a single lactiferous duct; most common cause of bloody nipple discharge

What is the likely diagnosis in a premenopausal woman with aversion to sexual intercourse due to muscle spasm/pain with penetration? External pelvic examination is unremarkable.
Genito-pelvic pain/penetration disorder (vaginismus)
treatment is aimed at relaxing the vaginal muscles (e.g. desensitization therapy, Kegel exercises); differentiated from vulvodynia by absence of pain to superficial touch of the vaginal vestibule

What is the likely diagnosis in a premenopausal woman with heavy menstrual bleeding and a uniformly enlarged, tender, globular uterus?
Adenomyosis
i.e. the presence of endometrial tissue in the uterine myometrium; typically presents in a women > 40 years old with new-onset dysmenorrhea

What is the likely diagnosis in a premenopausal woman with heavy menstrual bleeding and an irregularly enlarged uterus?
Leiomyomata uteri (fibroids)

What is the likely diagnosis in a woman that experiences mood swings, fatigue, bloating, and hot flashes one week prior to menstruation? The symptoms resolve with menses.
Premenstrual syndrome (PMS)
symptoms must cause impairment of function (e.g. missed work); other possible symptoms include irritability and breast tenderness

What is the likely diagnosis in a woman that presents with “labor pains” despite recently having her period? Pelvic examination reveals an irregularly enlarged uterus and a dilated cervix with a firm mass visible through the external os.
Prolapsing uterine fibroid
typically occur when a submucosal or intracavitary fibroid prolapses through the cervical os, resulting in labor pains and cervical dilation

What is the likely diagnosis in a woman that presents with fever and RLQ abdominal pain with a large multiloculated adnexal mass on ultrasound?
Tubo-ovarian abscess
severe complication of pelvic inflammatory disease

What is the likely diagnosis in a woman that presents with fever, lower abdominal pain, and purulent cervical discharge? Physical exam reveals cervical motion tenderness.
Pelvic inflammatory disease
typically preceded by Neisseria gonorrhoeae or Chlamydia trachomatis cervicitis

What is the likely diagnosis in a woman that presents with infertility and chronic pelvic pain with a fixed, immobile uterus on physical exam?
Endometriosis
pelvic adhesions may interfere with oocyte release and/or block sperm entry, thus causing infertility; resection of lesions improves conception rates

What is the likely diagnosis in a woman with a history of a dermoid cyst that presents with LLQ pain, nausea, and voluntary guarding? Pregnancy test is negative
Ovarian torsion
pain due to ischemia/necrosis of the affected ovary; ovarian torsion is more common in patients with a pelvic mass

What is the likely diagnosis in a woman with suspected pelvic inflammatory disease that presents with severe RUQ pain?
Fits-Hugh-Curtis disease (perihepatitis)

What is the likely diagnosis in a women age < 30 with a well-circumscribed, firm, mobile breast mass?
Fibroadenoma (benign)
fibroadenoma is firm and most common before age 30, versus a breast cyst, which is soft and most common after age 30



