Female Anatomy Flashcards
what are the 6 different functions of the bony pelvis?
support of upper body when sitting and standing
transference of weight from vertebral column to the femurs to allow standing and walking
attachment of muscles of locomotion and abdominal wall
attachment for external genitalia
protection of pelvic organs, their blood and nerve supplies, their venous and lymphatic drainage
passage for childbirth
the bony pelvis consists of what 3 structures?
2 hip bones
sacrum
coccyx
*coccyx not part of pelvic girdle

each hip bone is a fusion between which three structures?
ilium
ischium
pubis
*ischium and ilium fused from age 4-5, these do not fuse with pubis until puberty

identify the following structures within the ilium:
a) iliac crest
b) iliac fossa
c) ASIS
d) PSIS

identify the following structures within the ischium:
a) ischiopubic ramus
b) ischial tuberosity
c) ischial spine

identify the following structures within the pubis:
a) ischiopubic ramus
b) pubic arch
c) sub-pubic angle
d) pubic tubercle
e) superior pubic ramus

what are the contents of the pelvis inlet?
sacral promontory
ilium
superior pubic ramus
pubic symphysis

what are the contents of the pelvic outlet?
pubic symphysis
ischiopubic ramus
ischial tuberosities
sacrotuberous ligaments
coccyx

what is the space within the bony pelvis which lies between the pelvic inlet and pelvic outlet called?
pelvic cavity

the pelvic cavity lies continuous with abdominal cavity above, but what separates the pelvic cavity from peroneum?
pelvic floor
name the palpable surface landmarks of the pelvis?
*the inguinal ligament attaches between the ASIS and pubic tubercle

identify the structures of the bony pelvis on x-ray images?

identify the location of the following joints within the pelvis:
a) sacroiliac joint
b) hip joints (synovial)
c) pubic symphysis (secondary cartilaginous)

what are the two ligaments within the pelvis that we must know?
*there are a large number
sacrotuberous ligaments
sacrospinous ligaments
*these ensure the inferior part of the sacrum is not pushed superiorly when weight is suddenly transferred vertically through vertebral column (eg when jumping or during late pregnancy)

do these ligaments constrict or relax during late pregnancy?
relax
which two foraminae do the sacrotuberous and sacrospinous ligaments form?
greater and lesser sciatic foraminae

what is the obturator canal?
area of obturator foramen which is not covered by obturator membrane
contains obturator nerve and vessels

why do pelvic fractures tend to be multiple or combined with joint dislocation?
it is very hard to break a ring in just one place
identify vessels within the bony pelvis which can cause life threatening haemorrhage and/or damage to pelvic organs during trauma?

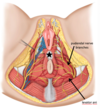
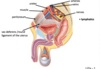
identify the difference between the male and female pelvis?
male = left
female = right (AP and transverse diameters are larger both at pelvic inlet and outlet. The subpubic angle and arch is wider. The pelvic cavity is also more shallow)

what is “moulding”?
the movement of one bone over another to allow the foetal head to pass through pelvis. The presence of the sutures and fontanelles (soft spots) allows bones to do this

what is the “vertex” of the foetal skull?
an area of the skull outlined by anterior and posterior fontanelles and parietal eminences. Important during childbirth to identify where head is lying

what is the difference between the occipitofrontal and biparietal diameters of foetal skull?
the occipitofrontal diameter is longer then the biparietal diameter (ie head is longer than it is wide)

giving that the transverse diameter of the pelvis is wider than AP diameter (female) and also that the occipitofrontal diameter is longer than biparietal diameter (foetus), how should foetus enter pelvic cavity?
facing either to the right or left (transverse) direction
*the distance of the foetal head from the ischial spines is referred to as the “station”. A negative number means the head is superior to the spines, and a positive number means the head is inferior to the spines