Cervical Screening / Vulval Pathology Flashcards
identify the cells present within normal ectocervix?

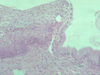
what does the endocervix normally look like histologically?

what is the transformation zone and which physiological changes causes the altering of position of TZ during life?
squamo-columnar junction between ectocervical (squamous) and endocervical (columnar) epithelia
position of TZ alters in response to menarche, pregnancy and menopause
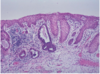
what does the squamo-columnar junction look like histologically?
what is cervical erosion?
the exposure of delicate endocervical epithelium to acid environment of vagina leads to physiological squamous metaplasia
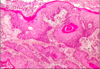
what are nabothian follicles?
mucous filled cyst on surface of cervix - formed when stratified squamous epithelium of ectocervix (nearest vagina) grows over columnar epithelium of endocervix (portion nearest to uterus)
what are the symptoms and causes of cervicitis?
often asymptomatic but can lead to infertility due to simultaneous sildent fallopian tube damage
causes - non specific inflammation, follicular cervicitis (sub epithelial reactive lymphoid follicles present in cervix), chlamydia and HSV
what is a cervical polyp and what is the main symptom?
localised inflammatory outgrowth (not premalignant)
cause of bleeding, if ulcerated
what are the different neoplastic causes of cervical pathology?
cervical intraepithelial neoplasia (CIN)
cervical cancer = squamous carcinoma, adenocarcinoma
what are the risk factors for CIN / cervical cancer?
high risk HPV esp 16 and 18 (sexual partners may increase risk)
vulnerability of SC junction in early reproductive lise - age at first intercourse, long term use of OCP, non use of barrier contraception
smoking - 3x risk
immunosuppression
what strains of HPV causes genital warts and what does this look like histologically?
HPV 6 and 11
condyloma acuminatum = thickened “papillomatous” squamous epithelium with cytoplasmic vacuolation (koliocytosis)
what strains of HPV causes cervical intraepithelial neoplasia (CIN) and what does this look like histologically?
HPV 16 and 18
infected epithelium remains flat, but may show koilocytosis, which can be detected in cervical smears

what does cervical cancer look like histologically?
invasive squamous carcinoma - virus integrated into host DNA
how long does it take for HPV infection to progress to high grade CIN?
6 months - 3 years
how long does it take for high grade CIN to become invasive cancer?
5-20 years
what does mild dyskaryosis with viral features (HPV) look like?

what is cervical intraepithelial neoplasia (CIN) and where does it occur?
pre-invasive stage of cervical cancer - dysplasia of squamous cells which is not visible by naked eye and is asymptomatic
occurs at transformation zone
detected by cervical screening
describe the progressive degrees of dysplasia and neoplasia of cervix?
normal squamous epithelium -> koilocytosis -> CIN1 -> CIN2 -> CIN3

describe the general histology of CIN?
delay in maturation / differentiation (immature basal cells occupying more of epithelium)
nuclear abnormalities (hyperchromasia, increased nucleocytoplasmic ratio, pleomorphism)
excess mitotic activity (situated above basal layers, abnormal mitotic forms)
often koilocytosis (indicating HPV) also present, CIN is graded I-III
descrbe the histology of CIN I?
basal 1/3 of epithelium occupied by abnormal cells
*raised numbers of mitotic figures in lower 1/3
*surface cells quite mature, but nuclei slightly abormal

describe the histology of CIN II?
abnormal cells extend to middle 1/3
*mitoses in middle 1/3
*abnormal mitotic figures

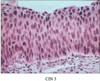
describe the histology of CIN III?
abnormal cells occupy full thicknes of epithelium
*mitoses, often abnormal, in upper 1/3
75-95% of malignant cervical tumours are what kind?
invasive squamous carcinoma (2nd most common female cancer worldwide)
*develops from CIN - preventable by screening
what are the different stages of invasive squamous carcinoma?
stage 1A1 - depth up to 3mm, width up to 7mm
stage 1A2 - depth up to 5mm, width up to 7mm (low risk of lymph node metastases)
stage 1B - confined to the cervix
stage 2 - spread to adjacent organs (vagina, uterus, etc)
stage 3 - involvement of pelvic wall
stage 4 - distant metastases or involvement of rectum or bladder
what are the symptoms of invasive cervical carcinoma?
abnormal bleeding - post coital, post menopausal, brownish or blood stained vaginal discharge, contact bleeding (friable epithelium)
pelvic pain
haematuria / urinary infections
ureteric obstruction / renal failure
describe the spread of cervical squamous carcinoma?
local = uterine body, vagina, bladder, ureters, rectum
lymphatic = early = pelvic, para-arotic nodes
haematogenous = late = liver, lungs, bone
how is cervical squamous carcinoma graded?
well differentiated
moderately differentiated
poorly differentiated
undifferentiated / anaplastic

where do cervical glandular intraepithelial neoplasia (CGIN) arise from and what is it the preinvasive phase of?
arise from endocervical epithelium
CGIN is preinvasive phase of endocervical adenocarcinoma
what is the difference in ease of diagnosis of CIN vs CGIN?
CGIN is more difficult to diagnose on cervical smear than squamous carcinoma
therefore, screening less effective
what does high grade CGIN look like histologically?

endocervical adenocarcinoma makes up what % of cervical cancer?
5-25%
*iincreasing incidence, particularly in young women
some cervical cancer are mixed type (adenosquamous) which arise from common cell of origin - true or false?
true
what has a worse prognosis - endocervical adenocarcinoma or squamous carcinoma?
cervical adenocarcinoma
in which people is adenocarcinoma more common?
higher SE class
later onset of sexual activity
smoking
HPV again incriminated, particularly HPV18
what does adenocarcinoma look like histologically?

name 3 other HPV-driven diseases?
vulvular intraepithelial neoplasia, VIN
vaginal intraepithelial neoplasia, VaIN
anal intraepithelial neoplasia, AIN
what disease is vulval intraepithelial neoplasia associated with?
pagets disease
*crusting rash, tumour cells in epidermis which contain mucin
*mostly no underlying cancer, tumour arises from sweat gland in skin

in older women, VIN causes greater risk of progression to what?
invasive squamous carcinoma
VIN is always HPV related - true or false?
false - often HPV related but not always
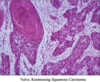
who does vulvar invasive squamous carcinoma arise in and how does it present?
elderly women
ulcer or exophytic mass
how does vulvar invasive squamous carcinoma arise?
from normal epithelium or VIN
*they are mostly well differentiated (verrucous are an extremely well differentiated type)
what is the treatment of vulvar invasive squamous carcinoma?
surgical - radical vulvectomy and inguinal lymphadenectomy
*90% 5 year survival - node negative
*<60% 5 year survival - node positive
what infections can cause vulval disease?
candida (particularly diabetics)
vulvar warts (HPV 6 and 11)
bartholin’s gland abscess (blockage of gland duct)
what non neoplastic epithelial disorders can cause vulval disease?
lichen sclerosis
other dermatoses - lichen planus, psoriasis
what causes atrophic vulval diseases?
post-menopausal
name 3 types of vaginal pathology?
VaIN - vaginal intraepithelial neoplasia - may also have cervical and vulval lesions
squamous carcinoma - less common than cervical and vulval counterparts, a disease of elderly
melanoma - rare, may appear as a polyp


