Eye disease Flashcards
part 1,2,3
WHta do we need to be able to see?

Some processing visual signals ar ein retina but most is in the brain

The eye and what happens where
- We need to get clear retinal image so need smooth refractive surface and transparancy of cornea with clarity of lens and then healthy optic nerve to transmit electrical signals ot brian so it can begin to interpret what we are seeing.

The cornea
5 layers
- Outmost layer is epitheliam cells
- Responsible for majoirty of refraction of light
- Needs to be smooth for clear image to be fgormed
- Transparancy maintained in part of epithelium (stoped tears enterign cornea) and endothelial cells which pump aqueous out of cornea to maintain clear cornea and supply nutrients.
- Can get oxygen form atmsophere to meet metsbolic needs.
- Endothelial cells do not reproduce

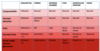
Refractive Errors
- SHape and size has impact on refraction of light but axial length has greater effect
- Hypermetropia/ myopia - due to difference in axial length then image may be formed behind or in front of retina not retinal plane lik emmetropria.

Astigmatism
- Cornea is not spherical
- Different radii of curvature in different axes
- In this case the verticsl radius is hsorter than horizontal radius so the curvature of the cornea is steeper in the vertical axis than horixontal axis
- To correct this a cyclindrical lens is needed with different powers in different axis
- Often described as rugby ball eyes

Corneal Disease
- Corneal ulcer - massive white area in middle and would be unabel to see through this. often by poor hygiene of contact lenses wearer.
- Corneal dystrophy - rare and some have genetic inheritance. Depends on opacity as to if they can see well.
- Keratoconus - cornea becomes distored

The lens
- SOme refraction
- Accomdoation/ fine focus - circumferential ciliary muscle contracts allowing lens capsule to relax, lens beocmes more spherical
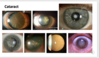
- Cataract = clouding of the lens -> age, diabetes, corticosteroids, congenital, trauma. Can be treated by surgery.

Cataract on image
Clouding of the lens
Age, diabetes, corticosteroids, congenital, trauma
Csn be treated by surgery
Retina layers
Centrla retinal arteru - to inner layers
chroid artery - to outer layer
Retina =

Optical Coherence Tomography
Allows oyu to see the exact layer where disease has occured

Foveal dip
Wher elight entering eye csn cause sharpest image as highest visual acuity

Concentration of Rods and Cones in Retina

Photoreceptors
Where phototrasnduction tkes place
Light stimulates chemical cascade -> hyperpolarisation
- Rods scotopic vision
- Cones photopic vision
- Disks hold opsin molecules
- Rhodopsin in rods, iodopsin in cones
- Light stimulates the isomerisation of retinal which activates opsin leading to hyperpolarisation of the photoreceptor.
- 3 different opsins present in all cones but one predominates in each of three different cones:
- “Blue” cones containing mostly blue-sensitive opsin are excited chiefly by a wavelength of around 420 nm,
- “Green” cones by a wavelength around 530 nm, and
- “Red” cones by a wavelength near 560 nm.

Phototransduction
Photons -> electrical signals that leave eye within optic nerve

On and off switches in phototransduction
Need to know: cells of inner retina are used in modifcation of the electrical signal created by transduction

Retinal Disease
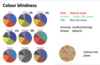
- Colour blindness
- Retinal vascular occlusion
- Diabetes
- Macular degeneration
- Retinal detachment

Colour blindness
Multiple forms depending on which cones affected and if total loss or problem with functioning.
Red-green colour blindness is most common and usually mild (anomaly)
Uusually tested with ishihara test plates
Coronar retinal artery occlusion (CRAO)
If the retina loose blood supply then the retina thins as cells die
Vision is very poor - usually present with sudden/total visual loss and not much can be done

Diabetic Retinopathy
Small blood vessels leak or get blocked
Loose pericytes so vessels expand and leak
Leads to oedema, exudation and haemorrhage in inner retinal layers
Vascular occlusion -> vascular dilation -> haemorrhage
Can see large amount exudste surrounding fovea area and lot shaemorrhages. Can treat with intervitreous injections

Wet Age -related macular degeneration
Often present with distortion

Why do you get distorition with Wet ARMD

Retinal Detahcment
Mor eprone if trauma to eye or diabetic. As we age vitreous retracts as scaffold so retina can move around and can detach from back of eye. but if vitreous remains slightly attached the traction can caue tear to form and fluid from vitreous cavity can lead behind retina and cause detachment.
Retina usually stays in place form vitreous scaffold and continuous pumping of retinl pigment epitheliun keeping potential space fluud free.
Symptoms - flashign lights,lots floaters and potentiall shadow appearing in vision.
Need to reatch retina as soon as possible so the photoreceptors can receive adewuate blood supply