End of Life Flashcards
The Top 2 Desires in Dying
- Relieve the burden on caregivers
- EX: Mother taken care of by children- not wanted
- Receive adequate pain and symptom management
Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment (1995) that found there was limited communication between physicians and patients, more than 1/3 of those who died spent at least 10 days in ICU, 46% of patients received mechanical ventilation within 3 days of death, and dying patients were in moderate to severe pain at least half of the time.
SUPPORT Study
Previous standard of care for pain control at End of Life was _______, which is now known to cause seizures.
Demerol
To qualify for hospice, the patient must have a life-threatening illness with a life expectancy of less than _______.
6 months
To qualify for hospice, the patient must forego _________.
curative treatment
Hospice care can be provided in ______, ________, or ________.
home, hospital, nursing home
Hospice places an emphasis on ___________ care.
interdisciplinary
***All hospices develop ______ _______ based on the family’s _______.**
shared goals; wishes
The difference between hospice and palliative care is _________.
who can be cared for
In palliative care, patients may still receive _______ treatment.
curative
- Fear
- Lack of experience/understanding
- Health care provider insensitivity
- Sense of guilt for failure to cure patient
- Disagreement with patient/family decisions
- Physical/emotional distance
- Unresolved personal grief issues
- Ethical concerns
Barriers to Communication for Healthcare Providers
An individual instruction or a written statement, witnessed, and governing the withholding or withdrawing of life-prolonging intervention, voluntarily executed by a person
Advanced Directive
Pain that results from infiltration, compression, distention, or stretching of thoracic or abdominal viscera
nociceptive pain
pain that results from injury to the peripheral or central nervous systems as a consequence of the tumor compressing or infiltrating nerves, nerve roots, or the spinal cord
neuropathic pain
At a pain scale of 4 - 6, we can administer _____.
opiods (like codiene)
AT pain scale of 7+, we can administer _______.
Fentanyl
Most EOL patients are ________, meaning they could easily develop respiratory depression.
Opioid naïve
The gold standard opiod medication
Morphine
Opioid Medications given at EOL
- Morphine
- Oxycodone
- Fentanyl
- Methadone
- Hydromorphone (Dilaudid)
Transient exacerbation or flare-up of pain that occurs in patients with otherwise well-controlled baseline pain
Breakthrough Pain
For pain crisis, give ___ mg bolus then every 8 minutes, ______ the dose.
2; double
opiods treat ________ pain
nociceptive
tricyclic antidepressants treat ________ pain
neuropathic
Adverse Effects of opioids
- Constipation
- Sedation
- Respiratory depression
- Nausea and vomiting
- Myoclonus
- Pruritis
- Urinary retention
Meds given to reduce pruritus caused by opioids:
- Embeda
- Narcan (w/ morphine)
Medications given for Palliative Sedation Therapy:
- benzodiazepines
- ketamine
- propofol
Meds given in addition to pain & sedation meds for EOL:
- NSAIDS
- Prednisone
- Anticonvulsants
- Tricyclic antidepressants
- Local anesthetics
- Anticancer therapies
- Bisphosphonates
- Diuretics
medication given at EOL to help w/ nerve pain or inhibit prostaglandin synthesis in uterine cancer
Prednisone
The gold standard of care for dyspnea at EOL
opioids- Morphine
Goal of Treatment of Dyspnea at EOL
treat the cause and relieve the psychological distress and accompanying autonomic response
Medications for Dyspnea at EOL
- Opioids (Morphine)
- O2 and humidified O2
- Anxiolytics (benzodiazepine)
- Inhalers and nebulizers (steroid inhalers/ albuterol)
- Diuretics
- Anticholinergics
Nonpharmacological Interventions for Dyspnea at EOL
- Use a fan to help circulate the air
- Open a window
- Wet cloths
- Restrict the number of people in the room
- Reposition the patient- elevate HOB
Medications for N&V at EOL
- Dopamine antagonists- Phenergen, Haldol, Reglan, Compazine
- Antihistamines- Benadryl, Antivert, Meclizyne
- Anticholinergics- Scopalamine patch
- Serotonin antagonists- Zofran
- Prokinetic agents- Reglan
- Antacids- Dexamethasone
- Others- Marijuana
Medications for Constipation at EOL
- Laxatives (stimulants and osmotics)
- Stool softeners
- Lubricants
- Enemas
- Prokinetic agents
Medications for Diarrhea at EOL
- Loperamide (Immodium)
- Diphenoxylate/atropine (Lomotil)
- Tincture of opium (Paregoric)
- Octreotide
Medications for Anorexia at EOL
- alcohol (Eldertonic)
- dexamethasone
- megastrol acetate (Megase)
- THC
Medications for Fatigue at EOL
- steroids
- low-dose stimulants
Nonpharmagological Interventions for Insomnia at EOL
- Encourage a regular sleep schedule
- Avoid staying in bed
- Avoid caffeine and alcohol intake
- Avoid overstimulation (need 8 hours of “lights out”)
- Control pain during the night
Medications for Insomnia at EOL
- anxiolytic/hypnotics
- benzodiazepines
- sedating antidepressants
EOL condition consisting of confusion, anxiety, restlessness, hallucinations, and agitation caused by antianxiety meds, opioid toxicity, metabolic disorders, full bowel or bladder (urinary retention), or impending death with symptoms of moaning and picking at air/sheets
Terminal Delirium
Goal of EOL care
comfort and peaceful death
The 5 Tasks for the Patient & Family at EOL
- To ask forgiveness
- To forgive
- To say “thank you”
- To say “I love you”
- To say “goodbye”
Stage of EOL characterized by the person beginning to withdraw, hyponatremia, decreased pain (natural endorphins), decreased food intake, confusion, increased sleep (separating from life), and less need to communicate with others
1 - 3 months before death
In 1 - 3 months prior to death, discourage ____ and ____ because systems are shutting down so food will stay in stomach longer causing distress & potential for aspiration
IVs & tube feedings
Stage of EOL characterized by “actively dying”, sleeping most of the time, visions occurring, agitation (picking), decreased BP, decreased urine output, increased perspiration, changing skin color, and breathing changes/ “death rattle”
1 - 2 weeks prior to death
Interventions for “Death Rattle”
- Anticholinergics- Scopalamine
- Positioning
- Mouth care (do not suction)
stage of EOL characterized by surge of energy, increased intensity of symptoms like restlessness & congestion, open or semi-open eyes, mottles hands/feet, irregular breathing, weakened pulse, decreased urine output, incontinence of urine and stool, and cardiac dysrhythmias
1 - 2 days prior to death
If cardiac dysrhythmias develop during EOL, the nurse should discuss shutting down an _____ if the patient has one.
ICD
At 1 - 2 days prior to death, for irregular breathing, the nurse should _____________.
raise HOB but do not give O2
EOL Respirations
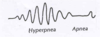
Cheyne Stokes Respirations
stage of death lasting minutes characterized by “fish out of water breathing” in which the patient cannot be awakened
actual death
The total cessation of life processes that eventually occurs in all living organisms (Encyclopedia Britannica) or…
The cessation of integrated tissue and organ function, manifested by cessation of heartbeat, absence of spontaneous respirations, or irreversible brain dysfunction
Death Definition
How to document death
no breath sounds, no audible heart tones, pupils fixed & dilated
The most definitive sign of death
pupils fixed & dilated
Signs of Death
- Breathing stops
- Heart stops beating
- Pupils become fixed and dilated
- Body color becomes pale and waxen
- Body temperature drops
- Muscles and sphincters relax
- Urine and stool may be released
- Eyes may remain open and there is no blinking
- Jaw may fall open
- May hear trickling of fluids internally
Steps to Pronouncing Death
- Identify the patient
- Test for response to verbal/tactile stimuli
- Listen for absence of heart sounds; feel for absence of carotid pulse
- Look, listen for absence of spontaneous respirations
- Document the position of the pupils and absence of pupillary light reflex
- Document the time at which the assessment was completed
Rigamortis sets in at ___ to ___ hours.
4 - 6
According to the IOM, a good death is:
- free from avoidable distress & suffering for patients, families, & caregivers
- in accordance with the wishes of the patient and his family
- consistent with clinical, cultural, and ethical standards


