Diagnosis of disorders of the gut and liver using blood tests Flashcards
What enzymes catalyse these reactions?

Transaminase enzymes – ALT and AST

Where are these enzymes found?


What is the LFT?


Serum activities of ALT and AST are based on which three factors?
- The extent of the damage to the tissue releasing transaminases
- The amount of each transaminase in that tissue
- The rate of clearance of the enzyme from the circulation
The published half-life for ALT is ____h and for AST only ___h
The published half-life for ALT is 47h and for AST only 17h
What are the 2 types of AST in hepatocytes?
Complicating factor – Hepatocytes have two forms of AST – cytosol and mitochondrial.
Does BMI cause ALT to increase or decrease?
Increase
What can change transaminases results?
- Biological variables
- Diurnal variation
- Dietary factors eg coffee
- Race - values higher if African or Hispanic
- Weight - Reference range selection
- Population exclusion criteria - the more rigorous the lower the reference range
- Skewed distribution curve
3.Drugs - both prescribed and over-the-counter
What is ALP?
Alkaline phosphatase (ALP)
catalyzes the hydrolysis of phosphate monoesters.
membrane-bound and mainly found in the liver and bone.
In liver its found in cells which are next to the canaliculi
Upregulated (rather than released due to damage) in response to bile duct obstruction and infiltrative or space-occupying lesions within the liver.
What is GGT?
GGT
mainly found in hepatobillary system
Increase in blood concentration due to induction/increase synthesis:
by alcohol or drugs (anticonvulsants)
biliary obstruction
liver tumours
smaller increase seen in hepatitis
Which tissues contain these enzymes?


Both ____ and ____ may be induced by drugs or alcohol
Also some tumours contain ______
________ sometimes required
NB – Both ALP and GGT may be induced by drugs or alcohol
Also some tumours contain placental ALP
ALP isoenzyme pattern sometimes required
What are Protein Synthesis routine tests and what do they test?
Protein Synthesis routine tests are:
- Serum albumin concentration
- Prothrombin time – INR
- Removal of potentially toxic substances:
- Drugs eg alcohol, paracetamol
- Bilirubin – end product of haem (from Hb) degradation
How is bilirubin produced from haem?
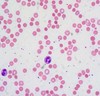
80% of bilirubin is from red cells taken up by the reticuloendothelial system for degradation.
Haem oxygenase releases the iron from the haem molecule to form biliverdin.
Biliverdin is then converted to bilirubin by biliverdin reductase.
Bilirubin released is tightly bound to albumin
What does total bilirubin measure?
Total bilirubin = conjugated + unconjugated
What is the difference between conjugated and unconjuagetd bilirubin?
•Conjugated
oApprox 40% of total
oWater soluble
oExcreted in bile
oIf elevated it appears in the urine giving a dark colour
•Unconjugated
oNot water soluble
oBound to albumin and does not therefore appear in the urine
What are the presenting features of liver disease?
- Jaundice with or without itching
- Pain - constant or colicky
- Non-specific - nausea, fatigue, weight loss
- Incidental laboratory finding
When is jaundice clinically identifiable?
Jaundice is clinically detectable at a serum bilirubin concentration of about 50 mmol/l and obvious to the individual at 100 mmol/l
How is liver disease diagnosed?
- The clinical presentation
- The pattern of routine liver tests
- How these point to more specific tests including diagnostic radiology
Female 49y colicky abdominal pain, RUQ tenderness, later jaundice, pale stools

- Presentation related to her pain
- Early elevation of ALP and GGT – before jaundice
- Then elevated bilirubin – recognising her jaundice
- ALT remaining relatively normal
- Pattern of dark urine and pale stools
The rise in ALP and GGT is due to enzyme induction secondary to obstruction of the biliary tree.
What pattern of LFTs do not occur in the presence of protein synthesis inhibitors?
The rise in ALP and GGT is due to enzyme induction secondary to obstruction of the biliary tree.
Animal studies show this rise in serum ALP and GGT activities does not occur in the presence of inhibitors of protein synthesis.
What are the extrahepatic and intrahepatic causes of obstructive jaundice?
Extrahepatic
- Gallstones – by far the commonest cause
- Malignancy – bile duct, pancreas
- Pancreatitis
Intrahepatic
- Hepatocellular disease (eg, resolving viral hepatitis)
- Drug-induced cholestasis
- Cholangitis
- Cirrhosis

- Clinically generally unwell and no significant pain
- Very raised ALT with raised bilirubin
- Some elevation of ALP and GGT due to swelling of liver tissue causing mild obstruction within the liver.
However these results just show severe hepatocyte damage and not the cause of that damage – that requires additional tests – in this case virology tests showed hepatitis B as the cause.
What does alcoholism do to AST and ALT?
In alcoholic hepatitis the serum activities of these transaminases are much less marked.
However the ratio of AST:ALT is frequently >2
Studies have indicated that in chronic alcohol excess mitochondrial AST is also elevated – NB its much longer half-life