Day 5 Gynaecology Flashcards
A 26-year-old woman attends the GP surgery reporting abdominal pains. She missed her last period and had unprotected sexual intercourse 7 weeks ago. She reports no vaginal discharge or per vaginal bleeding. She reports no urinary symptoms.
On examination, her abdomen is soft but there is mild suprapubic tenderness. Her heart rate is 70 beats per minute, blood pressure is 120/80 mmHg and she is apyrexial. You perform a pregnancy test which is positive.
According to current NICE CKS guidance, what is the next most appropriate management step?
(2)
Arrange immediate referral to the early pregnancy assessment unit
According to current NICE CKS guidance, women who have a positive pregnancy test and either abdominal, pelvic or cervical motion tenderness should be immediately referred for assessment. This is to exclude an ectopic pregnancy, which could potentially be fatal.
Bleeding in the first trimester differentials
(4)
miscarriage
ectopic pregnancy
- the most ‘important’ cause as missed ectopics can be potentially life-threatening
implantation bleeding
- a diagnosis of exclusion
miscellaneous conditions
- cervical ectropion
- vaginitis
- trauma
- polyps
A 22-year-old female presents to the Emergency Department with sudden-onset, right-sided lower abdominal pain over the past few hours. She has associated nausea and vomiting. The pain has now reached the point of being unbearable. She denies any fever, vaginal bleeding, dysuria or altered bowel habits. She has no significant past medical history. She does not take any regular medications.
On examination, she appears to be in significant pain, clutching at her right lower abdomen, which is tender on palpation. Normal bowel sounds are present. There is a palpable adnexal mass on pelvic examination. She is slightly tachycardic. A pregnancy test is negative and urinalysis is normal.
What finding on ultrasound would be characteristic of the likely diagnosis?
Whirlpool sign
Ovarian torsion may be associated with a whirlpool sign on ultrasound imaging

An 18 year-old girl presents to the Emergency Department with sudden onset sharp, tearing pelvic pain associated with a small amount of vaginal bleeding. She also complains of shoulder tip pain. On examination she is hypotensive, tachycardic and has marked cervical excitation.
What is the most likely diagnosis?
The history of tearing pain and haemodynamic compromise in a women of child bearing years should prompt a diagnosis of ectopic pregnancy.
A 25 year-old lady presents to her GP complaining of a two day history of right upper quadrant pain, fever and a white vaginal discharge.
She has seen the GP twice in 12 weeks complaining of pelvic pain and dyspareunia.
What is the most likely diagnosis?
(3)
The most likely diagnosis is pelvic inflammatory disease.
Right upper quadrant pain occurs as part of the Fitz Hugh Curtis syndrome in which peri hepatic inflammation occurs.
What is Fitz Hugh Curtis syndrome?
Right upper quadrant pain, associated with pelvic inflammatory disease in which peri hepatic inflammation occurs.
A 16-year-old female presents to the emergency department with a 12 hour history of pelvic discomfort.
She is otherwise well and her last normal menstrual period was 2 weeks ago.
On examination she has a soft abdomen with some mild supra pubic discomfort.
What is the most likely diagnosis?
Mittelschmerz
Mid cycle pain is very common and is due to the small amount of fluid released during ovulation.
Inflammatory markers are usually normal and the pain typically subsides over the next 24-48 hours.
What is Mittelschmerz?
(4)
Mid cycle pain is very common and is due to the small amount of fluid released during ovulation.
Just before an egg is released with ovulation, follicle growth stretches the surface of the ovary, causing pain.
Blood or fluid released from the ruptured follicle irritates the lining of the abdomen (peritoneum), leading to pain.
Inflammatory markers are usually normal and the pain typically subsides over the next 24-48 hours.
A 41-year-old female undergoes a cervical smear at her GP practice as part of the UK cervical screening programme.
Her result comes back as an ‘inadequate sample’.
What is the most appropriate action?
Cervical cancer screening: if smear inadequate then repeat within 3 months
A hirsute 28-year-old lady attends the GP practice complaining that her periods are absent.
What are the diagnostic criteria for polycystic ovarian syndrome (PCOS)?
(3)
PCOS should be diagnosed if 2/3 of the following criteria are present:
Infrequent or no ovulation (thus oligomenorrhoea is the correct answer in this scenario)
Clinical or biochemical signs of hyperandrogenism or elevated levels of total or free testosterone (no mention of ‘low levels of oestrogen’)
Polycystic ovaries on ultrasonography or increased ovarian volume
A 31-year-old woman presents for review in the outpatients’ department. She has a past medical history of polycystic ovarian syndrome and has been unsuccessfully attempting to conceive for the past ten months.
Upon examination she is hirsute.
Height and weight measurements are taken, confirming a body mass index (BMI) of 24kg/m².
What is the most appropriate management option for this patient?
Infertility in PCOS - clomifene is typically used first-line
A 29-year-old female was recently asked by her GP practice to attend for a repeat smear test.
Her initial test results 12 months ago showed that the sample was positive for high risk HPV (hrHPV), but cytologically normal.
The patient felt very anxious about having to be called back and asked the practice nurse what will happen next.
Assuming that the results return as hrHPV negative, which pathway will the patient be advised to follow?
Return in 3 years (normal recal)
Cervical cancer screening: if 1st repeat smear at 12 months is now hrHPV -ve → return to routine recall
The most common ovarian cancer
The correct answer is: Serous carcinoma
An ultrasound done on a 23-year-old female for recurrent urinary tract infections incidentally shows a 3 cm ‘simple cyst’ on the left ovary.
She is asymptomatic
The correct answer is: Follicular cyst
A 25-year-old female has her first cervical screen, the result is positive for high-risk human papillomavirus (hrHPV), cytology is normal.
12 months later she has a repeat test, again the result is positive for hrHPV, cytology is normal.
What action should be taken?
This patient should have a repeat test in 12 months.
Patients whose result is positive for hrHPV will have their samples examined cytologically. If the cytology is normal the test is repeated at 12 months. If the repeat test is still hrHPV positive and cytology is still normal they should have a further repeat test 12 months later, as per this patient.
A 52-year-old female has a cervical screen, results are negative for hrHPV.
Previous results have shown normal cytology.
Routine recall - repeat in 5 years
Patients whose test results are negative for hrHPV will not have their samples examined cytologically. They can return to routine recall.
Routine recall is every 3 years for patients aged 25-49 years and every 5 years for patients aged 50-64 years.
A 35-year-old female has a cervical screen, the result is positive for hrHPV with borderline changes in squamous cells.
What action should be taken?
Refer to colposcopy
This patient has abnormal cytology, therefore she should be referred for colposcopy.
A 27-year-old woman presents to the Emergency Department with sharp, right lower abdominal pain, which has been intermittently present for several days.
It does not radiate anywhere. It is not associated with any gastrointestinal upset.
Her last menstrual period was 8 weeks ago. She is sexually active although admits to not using contraception all the time.
Her past medical history includes multiple chlamydial infections. On examination, the abdomen is tender.
An internal examination is also performed; adnexal tenderness is demonstrated. A urine pregnancy test is positive.
Given the likely diagnosis, which of the following is the investigation of choice?
(2)
The investigation of choice for ectopic pregnancy is a transvaginal ultrasound
Transabdominal ultrasound is not ideal, as this is less sensitive than a transvaginal scan.
A 21-year-old female is found to have an ectopic pregnancy and is taken to theatre for surgical management.
When laparoscopy is performed, where is the ectopic pregnancy most likely to be found?
Most common site of ectopic pregnancy is in the ampulla of fallopian tube
A 62-year-old female presents as she feels she is becoming incontinent.
She describes no dysuria or frequency, but commonly leaks urine when she coughs or laughs.
What is the most appropriate initial management?
Pelvic floor muscle training
Urinary incontinence - first-line treatment:
- urge incontinence: bladder retraining
- stress incontinence: pelvic floor muscle training

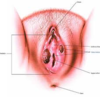
Features of cervical ectropion
(4)
Describes an increased area of columnar epithelium
May result in post-coital bleeding
May result in excessive vaginal discharge
Is more common during pregnancy
A 30-year-old woman comes for review.
She reports always having had heavy periods but over the past six months they have become worse.
There is no history of dysmenorrhoea, intermenstrual or postcoital bleeding.
She has had two children and says she does not want anymore.
Gynaecology examination is normal and her cervical smear is up-to-date. What is the treatment of choice?
Menorrhagia - intrauterine system (Mirena) is first-line
Which medication is used as a short-term option to rapidly stop heavy menstrual bleeding?
Norethisterone 5 mg tds can be used as a short-term option to rapidly stop heavy menstrual bleeding.
You are working in obstetrics & gynaecology. Your patient, a 26-year-old female, has presented to the early pregnancy assessment clinic with a 48-hour history of light vaginal spotting and vague lower abdominal pain.
Approximately 6 weeks previously, she took a home pregnancy test, which she found to be positive. Her last menstrual period was approximately 8 weeks ago.
Transvaginal ultrasound is performed, which fails to detect an intrauterine pregnancy.
Serum βHCG - 3,662 IU per ml
What is the most likely diagnosis in this patient?
Ectopic Pregnancy
In the case of pregnancy of unknown location, serum bHCG levels >1,500 points toward a diagnosis of an ectopic pregnancy
Tabitha is a 78-year-old woman who presents with urinary incontinence. Her incontinence has been ongoing for the past 2 years with no relief. Her symptoms usually occur on laughing and coughing. She has not experienced any episodes of nocturia. She also has not experienced a strong need to pass urine prior to her incontinence.
She has tried pelvic floor exercises and reducing caffeine intake but these failed to improve her symptoms.
Her urinalysis today shows no leukocytes or nitrites. A pelvic examination does not show any evidence of uterine prolapse. On consultation, she declines any surgical intervention.
What is the next most appropriate intervention for her incontinence?
(2)
Duloxetine is correct
Duloxetine may be used in patients with stress incontinence who don’t respond to pelvic floor muscle exercises and decline surgical intervention
Oxybutynin, tolterodine, and solifenacin are often used as 1st-line treatment for urge incontinence and are all antimuscarinic agents. Should these therapies fail, mirabegron, an β3 agonist, can be used as a 2nd-line therapy.
A 25-year-old accountant attends her first cervical smear appointment. She has not yet had any pregnancies, she has a history of pelvic inflammatory disease treated 4 years ago, and she currently has an intrauterine system in situ. There is no other significant past medical or social history. As it is her first smear, she asks you what it is we are testing for.
How would you counsel her?
Cervical smear samples are tested for hrHPV as the first step
A 58-year-old woman presents to her GP due to heavy bleeding from the vagina. Her last menstrual period was when she was 50 and she has had no vaginal bleeding since.
- She has a history of chronic obstructive pulmonary disease and gastro-oesophageal reflux disease.
- She takes a tiotropium/olodaterol inhaler and lansoprazole.
- She took the combined oral contraceptive pill for 25 years but did not use hormone replacement therapy.
- She has never been pregnant.
- She has a 40 pack-year smoking history.
What is the possible diagnosis?
What would be her most significant risk factor?
Endometrial cancer
nulliparity
Which three factors are prtective against endometrial cancer?
Smoking is a protective factor for endometrial cancer. It is however a risk factor for cervical, vulval, breast and many other cancers.
The use of the combined oral contraceptive pill is protective against endometrial cancer. It does, however, increase the risk of breast and cervical cancer.
During pregnancy, the balance of hormones shifts towards progesterone, which is a protective factor.
The risk factors for endometrial cancer are as follows*:
(6)
- obesity
- nulliparity/early menarche/late menopause (oestrogen exposure)
- unopposed oestrogen. The addition of a progestogen to oestrogen reduces this risk (e.g. In HRT). The BNF states that the additional risk is eliminated if a progestogen is given continuously
- diabetes mellitus
- tamoxifen
- polycystic ovarian syndrome
- hereditary non-polyposis colorectal carcinoma
A 76-year-old woman presents with post-menopausal bleeding for the past 4 months. She is diagnosed with well-differentiated adenocarcinoma (stage II) on endometrial biopsy. There is no evidence of metastatic disease.
Which is the most appropriate treatment?
(3)
Total abdominal hysterectomy with bilateral salpingo-oophorectomy is the treatment of choice for stage I and II endometrial carcinoma.
Provera is a progesterone used as a hormonal treatment for endometrial carcinoma - it acts by slowing the growth of malignant cells in the endometrium.
Wertheim’s radical hysterectomy includes removal of lymph nodes and is used to treat stage IIB endometrial carcinoma.
A mother attends the GP with her 14-year-old daughter. She is concerned as her daughter has not yet started her periods although suffers cyclical pain. On examination the daughter looks well.
What is the most likely diagnosis?
Imperforate hymen
Causes of primary amenorrhoea:
(7)
- Constitutional delay i.e. a late bloomer, has secondary sexual characteristics
- Anatomical i.e. mullerian agenesis (patient develops secondary sexual characteristics and has variable absence of female sexual organs)
- Imperforate hymen (characterised by cyclical pain and the classic bluish bulging membrane on physical examination)
- Transverse vaginal septae (characterised by cyclical pain and retrograde menstruation)
- Turner syndrome (XO chromosome)
- Testicular feminisation syndrome (XY genotype, no internal female organs)
- Kallmann syndrome (failure to secrete GNRH)
Causes of secondary amenorrhoea:
(8)
- Pregnancy
- Patient is using contraception
- Menopause
- Lactational amenorrhoea
- Hypothalamic amenorrhoea (suppression of GnRH due to stress, excessive exercise, eating disorder)
- Endocrinological (hyperthyroidism, polycystic ovary disease, Cushing’s syndrome, hyperprolactinaemia, hypopituitarism)
- Premature ovarian failure (autoimmune, chemotherapy, radiation therapy)
- Asherman’s syndrome (iatrogenic intrauterine adhesions/cervical stenosis)
Investigations for amenorrhoea
(5)
Pregnancy test
FSH/LH (if FSH is >20 in a woman <40 may suggest premature ovarian failure, if both are low it suggests a hypothalamic cause)
Thyroid function tests
Prolactin
Pelvic USS
Causes of puberty with short stature (3)
Causes of puberty with normal stature (4)
Delayed puberty with short stature
- Turner’s syndrome
- Prader-Willi syndrome
- Noonan’s syndrome
Delayed puberty with normal stature
- polycystic ovarian syndrome
- androgen insensitivity
- Kallman’s syndrome
- Klinefelter’s syndrome
An 80 year-old woman presents to her GP with a 1.5cm ulcerated lesion on her left labium majus.
Her history includes a two year history of vulval itching and soreness, which has failed to respond to topical steroid treatment.
What is the most likely diagnosis?
Vulval carcinomas are commonly ulcerated and can present on the labium majora.
What is the difference between vulval carcinoma and vulval intraepithelial neoplasia?
(2)
The difference between VIN and carcinoma isn’t ulceration, but rather invasion through the basement membrane.

A 36-year-old woman who used to inject heroin has recently been diagnosed HIV positive.
She is offered a cervical smear during one of her first visits to the HIV clinic.
How should she be followed-up as part of the cervical screening program?
Annual cervical cytology
Women who are HIV positive are at an increased risk of cervical intra-epithelial neoplasia (CIN) and cervical cancer due to a decreased immune response and decreased clearance of the human papilloma virus. (1) HIV positive women who have low-grade lesions (CIN1) do not clear these lesions and these can progress to high-grade CIN or cervical cancer. Even those women who are effectively treated with antiretrovirals have a high risk of abnormal cytology and an increased risk of false-negative cytology. (1)
A couple presents to their GP asking for advice about fertility. They have been having unprotected sexual intercourse 3 times a week for 1 year.
The GP suggests semen analysis and measuring serum progesterone levels.
When is the most appropriate time to measure serum progesterone levels?
To confirm ovulation: Take the serum progesterone level 7 days prior to the expected next period
A level >30nmol/l indicates ovulation so other causes of infertility should be considered.
A level below 30nmol/l does not exclude the possibility of ovulation but repeat testing will be required followed by referral to a specialist if it is consistently low.
What must serum progesterone levels indicate ovulation?
A level >30nmol/l indicates ovulation so other causes of infertility should be considered.
A level below 30nmol/l does not exclude the possibility of ovulation but repeat testing will be required followed by referral to a specialist if it is consistently low.
A 56-year-old lady reports incontinence mainly when walking the dog.
A bladder diary is inconclusive.
What is the most appropriate investigation?
Urodynamic studies are indicated when there is diagnostic uncertainty or plans for surgery.
Which tumour, if ruptured, may cause pseudomyxoma peritonei?

The correct answer is: Mucinous cystadenoma
Pseudomyxoma peritonei (PMP) is a very rare type of cancer. It usually begins in your appendix as a small growth, called a polyp. This is different to polyps that cause bowel cancer and is called a Low Grade Appendiceal Mucinous Neoplasm (LAMN).

The most common type of epithelial cell tumour

The correct answer is: Serous cystadenoma
Serous cystadenoma is a benign neoplasm composed of glycogen-rich epithelial cells that form innumerable small thin-walled cysts containing serous fluid

A 69-year-old female arrives in your clinic one morning complaining of recent urgency to pass urine and increased frequency, often followed by leakage of urine.
A urinary dipstick is negative, a vaginal examination is unremarkable and you do not suspect malignancy.
What is the likely diagnosis?
With this in mind, what is the best initial option to manage this patient’s condition?
1. The likely diagnosis is urgency urinary incontinence
2. bladder retraining
Urinary incontinence - first-line treatment:
- urge incontinence: bladder retraining
- stress incontinence: pelvic floor muscle training
A 25-year-old woman presents for her first cervical smear.
Which strains of HPV are most likely to cause cancer?
Cervical cancer:
Human papillomavirus infection (particularly 16,18 & 33) is by far the most important risk factor
A 28-year-old woman presents because she has not had a period for the past 9 months. She also describes fluid leaking from her nipples.
What is the diagnosis?
Prolactinoma
A 26-year-old woman presents 3 months after giving birth to her first child. During labour she had a large post-partum haemorrage. She did not breastfeed but has not had a period since.
What is the diagnosis?
(4)
Sheehan syndrome describes hypopituitarism caused by ischemic necrosis due to blood loss and hypovolaemic shock.
Features may include:
- agalactorrhoea
- amenorrhoea
- symptoms of hypothyroidism
- symptoms of hypoadrenalism
A 25-year-old woman presents 5 months after having dilation and curettage for a miscarriage. Since this procedure she has not had a period. A pregnancy test is negative. Hysteroscopy is performed which reveals the diagnosis.
What is the diagnosis?
Asherman’s syndrome, or intrauterine adhesions, may occur following dilation and curettage. This may prevent the endometrium responding to oestrogen as it normally would.
A 72-year-old woman with ovarian cancer is seen in the gynaecological oncology clinic.
There, the consultant talks through her pre-surgical prognosis, based on her risk malignancy index (RMI).
What are the three components of the RMI?
Risk malignancy index (RMI) prognosis in ovarian cancer is based on:
US findings
menopausal status
CA125 levels
You are going through your daily results and notice a cervical smear test that has come back for one of your patients. She is 34 years old.
The result says: ‘high-risk human papillomavirus (hrHPV) negative’. It states that this was a repeat test.
On reviewing her notes, this is her second repeat test following an abnormal result at a routine screening 2 years ago. Her last test was 12 months ago when she tested “hrHPV positive. Cytologically normal”. She has never been invited for a colposcopy.
What is the most appropriate next step?
Return to routine recall (in 3 years)
Cervical cancer screening: if 2nd repeat smear at 24 months is now hrHPV -ve → return to routine recall
A 25-year-old female student was brought in to the Emergency Department. She complains of a severe abdominal pain. The pain started suddenly 3 hours ago while she was shopping . Further questioning reveals that she has not had her periods for 7 weeks and is currently sexually active. She also reported a history of pelvic inflammatory disease 5 years ago. Abdominal examination reveals generalised guarding and signs of peritonism. An urgent ultrasound scan was ordered and showed free fluid in the pouch of Douglas with an empty uterine cavity. Urine βhCG was positive. Other basic bloods are sent.
While in the emergency department, she suddenly became very ill. Her observations were; Blood pressure 85/50 mmHg, Heart Rate 122/min, Respiratory Rate 20/min, O2 saturation 94%.
What is the next most appropriate action?
Resuscitate and arrange for emergency laparotomy
The clinical picture shows a high suspicion of ruptured ectopic pregnancy.
She turned very ill and went into shock (systolic BP < 90 mmHg). She is cardiovascularly unstable and an emergency laparotomy needs to be considered.
Nancy is a 37-year-old woman who is 19 weeks pregnant. She presents to the emergency department with a 2 day history of sharp abdominal pain.
There is no vaginal bleeding. She also has a low grade fever of 37.8 ºC.
Her pregnancy until now has been unremarkable. On examination, she is haemodynamically stable, but there is tenderness on palpation of the right lower quadrant of her abdomen.
Fetal heart rate was normal. An ultrasound scan was performed which showed a singleton pregnancy, and multiple large fibroids in the uterus.
The ovaries appeared normal and there was no appendix inflammation.
What is the most likely cause of the patient’s symptoms?
Fibroid degeneration may develop during pregnancy, presenting with low-grade fever, pain and vomiting.
A 41-year-old woman has been recalled for a repeat cervical smear by her general practitioner (GP). She previously had her routine cervical smear last year which showed the presence of high-risk human papillomavirus (HPV) but no abnormal cytology. Her repeat cervical smear is still positive for high-risk HPV with no cytological abnormalities.
What is the most appropriate step in this patient’s management?
Repeat cervical smear in 12 months
Cervical cancer screening: if 1st repeat smear at 12 months is still hrHPV +ve → repeat smear 12 months later (i.e. at 24 months)
A woman presents to her GP complaining of bleeding after sexual intercourse. What is the most common identifiable cause of postcoital bleeding?
Cervical ectropion is the most common identifiable cause of postcoital bleeding
A 47-year-old woman presents to her general practitioner (GP) for her routine cervical smear which was performed without any issues. She receives a letter to inform her that her cervical smear was negative for high-risk strains of human papillomavirus (hrHPV).
What is the most appropriate next step?
Repeat cervical smear in 3 years
Cervical cancer screening: if sample is hrHPV -ve → return to routine recall
Ms. Andrews a 24-year-old sales promoter was diagnosed with left tubal ectopic pregnancy 3 weeks ago.
Which medication was she started on?
However, her hCG titres failed to respond adequately.
Surgical treatment was indicated and considered. She has no significant medical history and is medically fit.
Which of the following surgery is mostly likely to be carried out by the surgeon?
- methotrexate
- Salpingectomy
A 72-year-old woman presents to her GP with symptoms of vaginal pain, itching and dyspareunia.
After ruling out other potential causes of her symptoms the GP diagnoses her with atrophic vaginitis.
Which treatment and adjunct therapy would be most appropriate?
in combination with topical oestrogen cream
Lubricants and moisturisers are useful adjuncts to topical oestrogen as first-line treatment of atrophic vaginitis
A 82-year-old woman presents to the general practitioner with a 2-week history of a labial lump. She denies pain but says that it is very itchy and rubs on her underwear. Her past medical history includes hypertension and type 2 diabetes mellitus for which she takes amlodipine, metformin and sitagliptin daily.
On examination, there is a 2cm x 3cm firm lump on her left labia majora. The surrounding skin appears normal with no erythema or induration. There is palpable inguinal lymphadenopathy.
What is the most likely diagnosis?
(3)
Older woman with labial lump and inguinal lymphadenopathy → ?vulval carcinoma
A 22-year-old woman presents to the Emergency Department with rapid onset abdominal pain.
The pain comes and goes in waves, is located in the right iliac fossa and is rated at 7/10 severity.
The patient feels nauseous and has vomited twice. Her last menstrual period was 3 weeks ago.
Ultrasound imaging of the abdomen reveals a whirlpool pattern in the right iliac fossa.
What is the most likely diagnosis?
Ovarian torsion may be associated with a whirlpool sign on ultrasound imaging
A 53-year-old woman presents with a 1-year history of involuntary urine leakage when she sneezes or coughs. She has also had similar incidents while exercising in the gym, which has caused significant embarrassment and now wears pads whenever she goes out.
She denies urinary urgency or frequency and opens her bladder once at night. She has no bowel-related symptoms.
What kind of incontinence does she have?
She has tried pelvic floor exercises with support from a women’s health physiotherapist for the past 6 months but still finds the symptoms very debilitating. She denies feeling depressed. She is keen to try further treatment, although is frightened by the prospect of surgery and would prefer alternative measures.
Urinalysis is unremarkable. On vaginal examination, there is no evidence of pelvic organ prolapse.
What is the next most appropriate treatment?
Duloxetine may be used in patients with stress incontinence who don’t respond to pelvic floor muscle exercises and decline surgical intervention
A 30-year-old lady presents to the gynaecological outpatient department after she presented to her GP complaining of inability to conceive despite attempting for 2 years.
A trans-vaginal ultrasound scan is performed, and the report is given below:
TV USSA shows = single 5 cm by 7 cm septated cyst is seen on the superior aspect of the right ovary. The left ovary is normal in size and morphology.
What further management would you suggest for this patient?
Perform a serum CA-125, αFP and βHCG, and book for elective cystectomy
Complex (i.e. multi-loculated) ovarian cysts should be biopsied with high suspicion of ovarian malignancy
Complex cysts - defined as cysts containing a solid mass, or those which are multi-loculated - should be treated as malignant until proven otherwise. The Royal College of Obstetricians and Gynaecologists Green-top Guidelines (No. 62) recommend that a serum CA-125, αFP and βHCG are performed for all pre-menopausal women with complex ovarian cysts. Aspiration of cysts is associated with higher rate of recurrence and increased spillage into the peritoneal cavity, which may disseminate possible malignant cells, hence the guideline prefers cystectomy over aspiration.
Physiological cysts (functional cysts)
(5)
Follicular cysts
- commonest type of ovarian cyst
- due to non-rupture of the dominant follicle or failure of atresia in a non-dominant follicle
- commonly regress after several menstrual cycles
Corpus luteum cyst
- during the menstrual cycle if pregnancy doesn’t occur the corpus luteum usually breaks down and disappears. If this doesn’t occur the corpus luteum may fill with blood or fluid and form a corpus luteal cyst
- more likely to present with intraperitoneal bleeding than follicular cysts
Benign epithelial tumours
(6)
- Arise from the ovarian surface epithelium
Serous cystadenoma
- the most common benign epithelial tumour which bears a resemblance to the most common type of ovarian cancer (serous carcinoma)
- bilateral in around 20%
Mucinous cystadenoma
- second most common benign epithelial tumour
- they are typically large and may become massive
- if ruptures may cause pseudomyxoma peritonei
A 25-year-old woman is investigated for acute pelvic pain and is diagnosed as having pelvic inflammatory disease. What is the most common cause of pelvic inflammatory disease in the UK?
Chlamydia trachomatis is the most common cause of pelvic inflammatory disease
A 30-year-old woman is 24 weeks pregnant and she receives a letter about her routine cervical smear.
She asks her GP if she should make an appointment for her smear.
All her smears in the past have been negative.
What should the GP advise?
NICE guidelines suggest that a woman who has been called for routine screening wait until 12 weeks post-partum for her cervical smear. If a smear has been abnormal in the past and a woman becomes pregnant then specialist advice should be sought. If a previous smear has been abnormal, a cervical smear can be performed mid-trimester as long as there is not a contra-indication, such as a low lying placenta.
Management options for endometriosis
(2)
localised disease is treated with total abdominal hysterectomy with bilateral salpingo-oophorectomy. Patients with high-risk disease may have post-operative radiotherapy
progestogen therapy is sometimes used in frail elderly women not consider suitable for surgery
Which two factors are protective against endometrial cancer?
(2)
*the combined oral contraceptive pill and smoking are protective
You are reviewing a 24-year-old woman who is 10 weeks pregnant.
Unfortunately, she is suffering from excessive vomiting and struggling to keep fluids down.
What is the most appropriate way to assess the severity of her symptoms?
PUQE score
Lydia is a 26-year-old woman who has come to her GP complaining of low mood, sleep disturbance and headaches. She says the symptoms come on around the same time each month and seem to stop just before her period. In between episodes she feel fine but is concerned about how these symptoms are affecting her performance at work. She does not plan to have children for at least the next couple of years.
Given the likely diagnosis which treatment is appropriate for Lydia at this stage?
Premenstrual syndrome: a new-generation combined oral contraceptive pill may be helpful
severe symptoms may benefit from a selective serotonin reuptake inhibitor (SSRI)
this may be taken continuously or just during the luteal phase (for example days 15–28 of the menstrual cycle, depending on its length)
A 23-year-old woman who has been diagnosed with polycystic ovary syndrome (PCOS) is trying to become pregnant.
She has already made any appropriate lifestyle changes and reduced her BMI to 25.
However, she remains anovulatory.
What is the most appropriate next step of treatment? (1)
How does it work? (2)
Clomifene is the traditional first-line ovulation induction drug used.
As an antioestrogen, it works by blocking oestrogen receptors in the hypothalamus and pituitary and increasing the release of LH and follicle stimulating hormone (FSH), which are inhibited by oestrogen.
It is only given on days 2 to 6 of each cycle to initiate follicular maturation.
A 31-year-old pregnant woman presents with severe vomiting.
She is currently 8 weeks pregnant and this is her second pregnancy.
Following Royal College of Obstetricians and Gynaecologists (RCOG) guidelines, which one of the following define the diagnostic criteria of hyperemesis gravidarum.?
Hyperemesis gravidarum, diagnostic criteria triad:
- 5% pre-pregnancy weight loss
- dehydration
- electrolyte imbalance
A 24-year-old woman presents to the emergency department with intermittent abdominal pain and vaginal bleeding. She thinks her last period was 6 weeks ago but cannot be certain. She has never been pregnant before and has no previous gynaecological history.
She is systemically well with a blood pressure of 130/85 mmHg and pulse 79 bpm. A pregnancy test performed in the department is positive and transvaginal ultrasound confirms a pregnancy in the adnexa with a fetal heart beat present. What is the most appropriate management in this case?
Surgical management - salpingectomy or salpingotomy
Surgical removal of the ectopic is the most appropriate option here. If the contralateral tube is healthy then salpingectomy may be the best option. However, if the contralateral tube is damaged, salpingotomy preserves the functional tube and helps minimise the risk of future infertility.
A 17-year-old girl presents due to painful periods.
These have been present for the past three years and are associated with a normal amount of blood loss.
Her periods are regular and there is no abnormal bleeding. She is not yet sexually active. What is the most appropriate first-line treatment?
Ibuprofen
NSAIDs are offered first-line as they will inhibit prostaglandin synthesis, one of the main causes of dysmenorrhoea pains.
A woman who is 9 weeks pregnant presents with vaginal bleeding. The cervical os is closed. An ultrasound shows an intrauterine pregnancy with a fetal heart. She has been pregnant once before which resulted in a miscarriage
What is the diagnosis?
The correct answer is: Threatened miscarriage
The possibility of bleeding due to non-pregnancy causes (e.g. cervical ectropion) should also be considered
A 22-year-old woman has a booking ultrasound scan. Her last menstrual period was 8 weeks ago. This shows an intrauterine sac with no fetal pole. These findings are confirmed with a transvaginal ultrasound.
The correct answer is: Missed miscarriage
A missed miscarriage is when a baby has died in the womb, but the mother hasn’t had any symptoms, such as bleeding or pain. Any type of miscarriage can cause shock, but a missed miscarriage can be particularly difficult because of the lack of symptoms.
A woman who is 10 weeks pregnant presents with heavy vaginal bleeding and crampy lower abdominal pains. On examination some clots are seen around an open cervical os
What is the diagnosis?
The correct answer is: Inevitable miscarriage
An 18-year-old presents with amenorrhoea for 6 months.
She previously had irregular periods with a cycle ranging from 25-39 days long and has had instances where a whole cycle was missed.
She is worried about the long-term implications for her ability to conceive.
She denies being sexually active and has no syndromic features on examination.
There is no significant acne or excess body hair. Her BMI is 20 kg/m² and she is training to run a full marathon.
What is the likely aetiology of her condition?
In a very athletic woman, hypothalamic hypogonadism is a common cause of secondary amenorrhoea
This is a case of secondary amenorrhoea in a young woman due to excessive exercise.
She is training for a marathon and has previously had issues with oligomenorrhoea.
Where the body has low levels of fat, the hypothalamus releases less gonadotrophin-releasing hormone which in turn causes hypogonadism.
This is thought to occur because very low-fat levels in a female are incompatible with successful pregnancy.
A 52-year-old woman presents to surgery seeking advice regarding contraception.
She has recently started in a new relationship but is unsure if she requires contraception, as she thinks she may be going through the menopause.
She is experiencing hot flushes and her last period was 7 months ago.
What is the most appropriate advice?
Need for contraception after the menopause
12 months after the last period in women > 50 years
24 months after the last period in women < 50 years
A 32-year-old woman presents to the fertility clinic accompanied by her partner. This is the fourth appointment she is attending.
She has been following all the indications given, such as exercise, weight loss, and regular intercourse, but she is still failing to conceive.
She has a past medical history of polycystic ovarian syndrome and she has a BMI of 20.3 kg/m². The doctor decides to try ovulation induction with this patient.
What medications should be prescribed?
(3)
Letrozole/clomiphene may be used for ovulation induction to treat infertility
Note: Gonadotrophins are considered for women with PCOS after attempts with other treatments have been unsuccessful, usually after weight loss, letrozole, and clomiphene trial.
A 33-year-old woman is reviewed regarding her asthma control.
You notice from her records that she has never had a cervical smear and raise this with her.
She responds that she is a lesbian and has never had sex with a man.
What is the most appropriate advice to give?
She should have cervical screening as per normal
HPV, the causative agent of cervical cancer, can be transmitted during genital contact or oral sex. Lesbian and bisexual women should therefore have cervical screening as normal. Unfortunately, the uptake amongst lesbian women is around 10 times worse than the general female population, sometimes as a consequence of incorrect advice from healthcare professionals.
A 34-year-old patient has attended the smear test clinic at her GP practice for a repeat test. Her last test was performed three months ago.
What would the results of the initial test have shown for the patient be required to have a repeat test 3 months later?
Inadequate sample
Cervical cancer screening: if smear inadequate then repeat within 3 months
If a smear test result comes back as ‘inadequate’ the patient will be asked to return for a repeat test within 3 months. If the second test is also ‘inadequate’, the patient will require colposcopy testing.
A 17-year-old Somali girl has presented to the emergency department with recurrent urinary tract infections.
On examination, with a chaperone, you notice the girl may have had a clitoridectomy.
You believe the girl has been subjected to female genital mutilation (FGM).
She asks for antibiotics and for no one else to be informed.
As well as treating the infection, what should you do?
Inform the medical team and the police
A 24-year-old woman presents to the emergency department with a 1 day history of nausea and severe constant pain localised since onset to the left iliac fossa. She had vomited once but has no other symptoms. She has a 28 day menstrual cycle, her last menstrual period started 7 days ago. She is sexually active and has always used condoms for contraception. There is no vaginal bleeding. What is the most likely diagnosis?
Ovarian torsion
A 28-year-old woman who is 11 weeks pregnant is referred to the early pregnancy assessment unit with a one day history of abdominal pain and vaginal bleeding. A trans-vaginal ultrasound scan confirms a failed intra-uterine pregnancy. The patient is currently afebrile and haemodynamically stable, but has a past medical history of Von Willebrand disease.
What is the most appropriate initial management of this patients miscarriage?
Medical management of a miscarriage involves giving vaginal misoprostol alone
According to NICE guidelines published in 2018, vaginal misoprostol is most appropriate as the patients past medical history of coagulopathy (Von Willebrand disease) is a contra-indication to expectant management, but not medical management.
A 65-year-old post-menopausal lady presents with bloating, unintentional weight loss, dyspareunia, and a raised CA-125.
Given the likely diagnosis, which of the following terms best describes how this cancer spreads initially?
Ovarian cancer initially spreads by local invasion
The stages of ovarian cancer are as follows:
- Confined to the ovaries (Stage 1)
- Local spread within the pelvis (Stage 2)
- Spread beyond the pelvis to the abdomen (Stage 3)
Stages of ovarian cancer
The stages of ovarian cancer are as follows:
- Confined to the ovaries (Stage 1)
- Local spread within the pelvis (Stage 2)
- Spread beyond the pelvis to the abdomen (Stage 3)
Which one of the following is the most common cause of recurrent first trimester spontaneous miscarriage?
Antiphospholipid syndrome
Antiphospholipid antibodies (aPL) are present in 15% of women with recurrent miscarriage, but in comparison, the prevalence of aPL in women with a low risk obstetric history is less than 2%
Recurrent miscarriage definition (2)
Recurrent miscarriage causes (5)
Recurrent miscarriage is defined as 3 or more consecutive spontaneous abortions. It occurs in around 1% of women
Causes
- antiphospholipid syndrome
- endocrine disorders: poorly controlled diabetes mellitus/thyroid disorders. Polycystic ovarian syndrome
- uterine abnormality: e.g. uterine septum
- parental chromosomal abnormalities
- smoking
A 29-year-old female undergoes a cervical smear test as part of the UK cervical screening programme.
Her results come back as hrHPV positive.
The sample is examined cytologically, which is reported as normal.
What is the most appropriate action?
Repeat the test in 12 months
A 33-year-old patient has received a letter from her local hospital regarding her recent smear test.
She is aware that she has had two consecutive inadequate sample results.
Due to the two inadequate sample results, what will the next step be for this patient?
Cervical cancer screening: if two consecutive inadequate samples then → colposcopy
A 36-year-old primigravida woman, at 9 weeks gestation, presents to the emergency department due to heavy vaginal bleeding. She reports bleeding large clots associated with cramping over the last 3 hours.
On examination, she is hypotensive at 80/60 mmHg and has a heart rate of 110 beats/minute. Pelvic examination revealed blood clots around her vagina. A speculum exam revealed active vaginal bleeding, with a dilated cervical os and a uterus consistent in size with an 8-week gestation. Pelvic ultrasonography showed small amounts of fluid in the endometrium with an intrauterine sac with a crown-rump length of 20mm and no fetal cardiac activity.
Which of the following is the most appropriate next step in management?
Dilation and curettage
This patient presents with first-trimester vaginal bleeding, with a dilated cervical os and an intrauterine sac that has no cardiac fetal activity. This is diagnostic of an inevitable miscarriage.
A 30-year-old woman who is investigated for obesity, hirsutism and oligomenorrhoea is diagnosed as having polycystic ovarian syndrome (PCOS) following an ultrasound scan. She is hoping to start a family and her doctor starts metformin to try and improve her fertility.
What is the mechanism of action of metformin in PCOS?
Increases peripheral insulin sensitivity
The majority of patients with polycystic ovarian syndrome have a degree of insulin resistence which in turn can lead to complicated changes in the hypothalamic-pituitary-ovarian axis.
A 25-year-old woman presents with a 3 year history of dysmenorrhoea and deep dyspareunia.
The pain she experiences during her period can be severe and is associated with nausea.
She also states that she and her partner have now been trying for a baby for 24 months with no success.
What is the likely diagnosis?
The classic symptoms of endometriosis are pelvic pain, dysmenorrhoea, dyspareunia and subfertility
Define Adenomyosis
Adenomyosis (ad-uh-no-my-O-sis) occurs when the tissue that normally lines the uterus (endometrial tissue) grows into the muscular wall of the uterus. The displaced tissue continues to act normally — thickening, breaking down and bleeding — during each menstrual cycle.

A 33-year-old woman is investigated for infertility. Laparoscopy is essentially normal. Hysterosalpingography shows blocked fallopian tubes bilaterally.
What is the diagnosis?
The correct answer is: Pelvic inflammatory disease
A 27-year-old woman with a BMI of 18 is referred to a fertility clinic after failing to become pregnant after 2 years of trying with her partner. Male factor infertility has been ruled out and you suspect the patient’s low BMI may mean she is not ovulating.
Which hormone could you measure on day 21 of her menstrual cycle to test for ovulation?
Which range is implicative of a repeat test?
Progesterone

Key counselling points for conception
folic acid
aim for BMI 20-25
advise regular sexual intercourse every 2 to 3 days
smoking/drinking advice
A 25-year-old female is found to have an unruptured ectopic pregnancy. The decision is made to progress with medical management of the ectopic pregnancy.
What drug is used for this?
Methotrexate is the drug of choice for medical management of ectopic pregnancy
A 33-year-old woman and her husband present to their general practitioner (GP) complaining of difficulty conceiving. They have been having regular unprotected intercourse for 14 months and have not conceived yet. Semen analysis from the husband was normal. The GP requests a serum progesterone to check for ovulation.
When should this blood test be taken?
To confirm ovulation: Take the serum progesterone level 7 days prior to the expected next period
While working on a gynaecology ward you are looking after a 67-year-old female who has had an endometrial biopsy for post-menopausal bleeding.
Which of the following ovarian tumours is associated with the development of endometrial hyperplasia?
Granulosa cell tumours
Atyplical hyperplasia of the endometrium is classified as a premalignant condition
A 34-year-old woman presents to her GP. She is 14 weeks pregnant and, although her pregnancy has been uncomplicated so far, she has noted left-sided pelvic pain and deep dyspareunia over the last week. She denies vaginal bleeding, discharge or dysuria.
Her abdomen is soft and non-tender with a gravid uterus that is large for her dates. Her temperature is 37.1ºC, with a blood pressure of 110/70mmHg, a heart rate of 70 beats/min and a respiratory rate of 18 breaths/minute.
Prior to conception, she had an intrauterine system due to menorrhagia. She has no other medical history.
What is the most likely cause of her symptoms?
Uterine fibroids may grow during pregnancy
Uterine fibroids are sensitive to oestrogen and can therefore grow during pregnancy. If growth outstrips their blood supply, they can undergo red or ‘carneous’ degeneration. This usually presents with low-grade fever, pain and vomiting. The condition is usually managed conservatively with rest and analgesia and should resolve within 4-7 days.
You are an FY-1 doctor working on a gynaecology ward.
One of your patients has just been diagnosed with atypical endometrial hyperplasia. She is post-menopausal and otherwise fit and well.
What is the ideal management of this condition?
A total hysterectomy with bilateral salpingo-oophorectomy, in addition, is advisable for all postmenopausal women with atypical endometrial hyperplasia, due to the risk of malignant progression
A 54-year-old woman telephones her GP complaining of light, infrequent periods. She is also suffering from vaginal dryness, low mood and irritability, and hot flushes at night. The patient believes she is experiencing the perimenopause and is keen to start treatment for this. However, she has also been reading articles on the internet and is worried about the risk of endometrial cancer.
Which of the following therapies are likely to increase the risk of this condition?
HRT: unopposed oestrogen increases risk of endometrial cancer
A 16-year-old female presents with concerns that her periods have not started. Her sisters’ menarche was at age 13. On examination, the patient is short, showing no signs of development of secondary sexual characteristics and has widely spaced nipples. A systolic murmur was also noted to be present under the left clavicle.
Which finding is keeping with the most likely diagnosis of this patient?
Raised FSH/LH in primary amenorrhoea - consider gonadal dysgenesis (e.g. Turner’s syndrome)
The patient presents with widely spaced nipples and primary amenorrhoea which are characteristics seen in Turner’s syndrome. Turner’s syndrome is caused by the presence of only one sex chromosome (X) or a deletion of the short arm of one of the X chromosomes which results in the characteristics which commonly are manifested.
A 39-year-old woman presents with bloating and mild lower abdominal pain. The pain started 2 hours ago, and the bloating has been increasing for 6 hours.
On examination, there is abdominal tenderness, ascites but no guarding. She has no vaginal bleeding. Her vital signs include a heart rate of 97/minute, a blood pressure of 89/52 mmHg and a respiratory rate of 24/minute.
She is currently undergoing IVF treatment and received her final hCG injection 6 days ago. Whilst undergoing treatment, she has been having regular, unprotected sex.
A urinary pregnancy test is positive.
What is the most likely diagnosis?
OHSS
Risk factors for miscarriage
(7)

A 23-year-old female patient presents to her general practitioner with white, thick vaginal discharge which is itchy and is distracting her from her university work. She reports having tried over-the-counter remedies before for these symptoms as she has had 2 previous episodes of this in the past 5 months. She is sexually active and uses condoms and oral contraceptives. Her urine dip in the surgery is negative for pregnancy and protein, leucocytes and nitrites are also negative.
What would be the best management option for this patient with her recurrent symptoms?
An induction-maintenance regime of oral fluconazole should be considered for recurrent vaginal candidiasis
A 23-year-old woman presents to the GP requesting advice after having unprotected sexual intercourse the previous night. She took a dose of levonorgestrel 1.5mg (Levonelle) as emergency contraception approximately 12 hours after having intercourse. It is currently day 12 of her menstrual cycle.
She is very anxious that she may fall pregnant and would like to start taking a combined oral contraceptive pill (COCP) to avoid similar situations in the future.
How soon can she commence taking a COCP?
Hormonal contraception can be started immediately after using levonorgestrel (Levonelle) for emergency contraception
A 23-year-old woman presents to the GP requesting advice after having unprotected sexual intercourse the previous night. She took a dose of levonorgestrel 1.5mg (Levonelle) as emergency contraception approximately 12 hours after having intercourse. It is currently day 12 of her menstrual cycle.
She is very anxious that she may fall pregnant and would like to start taking a combined oral contraceptive pill (COCP) to avoid similar situations in the future.
How soon can she commence taking a COCP?
Hormonal contraception can be started immediately after using levonorgestrel (Levonelle) for emergency contraception
A 37-year-old woman presents to her GP to request emergency contraception after having unprotected sexual intercourse approximately 96 hours ago. She is currently completing a course of antibiotics to treat her recently diagnosed pelvic inflammatory disease (PID).
What is the most appropriate choice of emergency contraceptive for this patient?
Ulipristal (EllaOne) - a type of emergency hormonal contraception, can be used up to 120 hours post UPSI
Ulipristal acetate is the correct option, and is effective up to 120 hours post-unprotected sexual intercourse (UPSI). Its primary mechanism of action is thought to be the inhibition of ovulation.


