Cook - Diabetes Rx Flashcards
1
Q
What is HbA1C?
A
- Test for long-term control of blood glucose (glycosylation assay using a mass spec)
- Higher average blood glucose = more extensive glycosylation of hemoglobin
1. HbA1c is the fraction of Hb measured - RBCs live 3-4 mos, allowing testing of long-term glycosylation
- Normal (non-diabetic) HbA1c about 6%; over 8% for a diabetic is not good, over 10% is dangerous
1. ADA recommends A1C target of <6.5%
2
Q
In brief, what is T1D?
A
- A wasting disease: loss of glycogen, body fat, and muscle mass
- Excretion of glucose and ketone bodies into the urine
3
Q
What are the stimulants, amplifiers, and INH of insulin release?
A
- STIMULANTS of insulin release:
1. Glucose, mannose
2. Leucine
3. Vagal stimulation
4. Sulfonyl ureas - AMPLIFIERS of insulin release:
1. Enteric hormones: cholecystokinin, secretin, gastrin
2. Neural stimulation: beta-adrenergic - INHIBITORS of insulin release:
1. Somatostatin
2. Some drugs, i.e., diazoxide
3. Catecholamines
4
Q
What are the most important insulin actions in the liver, adipose, and skeletal/cardiac muscle?
A
- LIVER: stimulates conversion of glu to glycogen
1. Stimulates conversion of glu to FA, TAG - ADIPOSE: stimulates transport of glu into cells
1. Stimulates conversion of glu to FA, TAG
2. INH hormone sensitive lipase (release of free fatty acids) - SKELETAL and CARDIAC MUSCLE: stimulates transport of glucose into cells (passive transport via GLUT 4)
5
Q
Short-acting insulin
A
- Soluble, clear, crystalline zinc-insulin
- Aka, regular insulin: only preparation that can be injected IV -> all others SC or IM
1. Regular means soluble: Humulin, Novolin - All other preparations have been modified to provide prolonged action and are dispensed as turbid suspensions
- Animal insulins work just as well as the recombinant variations, but are now only available by special request
6
Q
Intermediate-acting insulin
A
- NPH insulin: Neutral, Protamine, Hagedorn
- Long-acting = large crystals = slow absorption
1. Depot of insulin with a longer 1/2 life
7
Q
Provide an example of insulin replacement therapy.
A
-
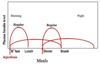
4 equivalent meals per day (high-carb snack before bedtime is fourth meal):
1. Measurements of glu before each meal
2. Injections of regular insulin (short half-life) and NPH or Lente insulin (longer half-life) combo at breakfast, dinner (after glu msmt)
a. Regular insulin for postprandial glucose rise after breakfast and after dinner
b. NPH or Lente insulin for postprandial glu rise after lunch and bedtime snack - Snack before bedtime helps the patient keep blood glucose in control
- Pt will have to make sure all of the different food intakes are pretty much the same to help regulate glucose levels and insulin injection
8
Q
How should insulin admin be adjusted?
A
- Msmts 4x/day, BEFORE each meal -> 2 insulin injections e/day
- Based on patient measurement of blood glucose, the following adjustments should be made:
1. Pre-lunch glu reflects AM REG dose; if too high, INC AM REG dose
2. Pre-supper glu reflects AM NPH dose; if too high, INC AM NPH dose
3. Pre-bedtime glu reflects PM REG dose; if too high, INC PM REG dose
4. Pre-breakfast glu reflects PM NPH dose; if too high, INC PM NPH dose - DEC insulin if glucose is too low
9
Q
How does an insulin pump work? Who is it good for?
A
- T1D: mechanical pump administers insulin through catheter into abdominal fat (also convenient for some T2D pts)
- Meal bolus injections, continuous infusion, variable infusion rates all possible
- Glucose monitoring REQUIRED
- Useful for young children and infants (even as young as 2-3 months old)
- Can only use regular insulin
10
Q
What are the two types of human insulin?
A
- Humulin: made using recombinant DNA to produce the hormone in bacteria or yeast
- Novolin: recombinant human insulin
-
11
Q
Recombinant glucagon
A
- Available for severe hypoglycemia (esp. in pts w/difficulty controlling blood glucose, aka brittle diabetics)
- Glucagon is a 29 AA peptide secreted by α-cells of the pancreas
1. Opposite effects to those of insulin
2. Elevated in fasting and diabetes
3. Used for hypoglycemia, usually because of unbalanced insulin/carbohydrate - Need friends/family capable of administration
- Dogs for Diabetics (D4D): dog smells acetone, carries kit, goes for help
12
Q
Rapid-acting insulin
A
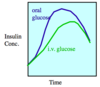
- Insulin in circulation forms hexamers with Zn2+ that don’t bind insulin receptor until dissociation
- Insulin lispro (Humalog®): analogue of Humulin® in which the normal Proline B28 and Lysine B29 are switched (by modified rDNA)
- Insulin aspart (NovoLog®): Asp substituted for Pro; also exists only as a monomer
- Insulin glulisine (Apidra®): AA asparagine at B3 is replaced by lysine and lysine in B29 replaced by glutamic acid (does NOT form hexamers)
- Same pharmacokinetic properties: faster onset of action and shorter half-life because MONOMERS (soluble)
1. Only monomers bind the insulin receptor
13
Q
Long-actin insulin
A
- Insulin glargine (Lantus®): modified recombinant human insulin analog -> altered isoelectric point
- Insulin detemir (Levemir®) is similar
- Long-acting (up to 24-hour duration of action), so can be injected once a day
1. When injected, acidic solution is neutralized, causing crystals to precipitate = slow absorption= long-acting (like NPH) - Low peak insulin concentration DEC chances of nocturnal hypoglycemia
- Bottle with pH 4.0 buffer (soluble at this pH): if you are administering this, there is a note on the glargine to let you know it is NOT for IV injection
14
Q
What are the various types of insulin and their duration (image)?
A
- Ultralente: larger, longer-acting crystal
- Glargine: can sometimes be a single injection each day (this is rare; most pts on combo of insulins)

15
Q
Human insulin powder
A
- 1st type was Exubera®, but Afrezza® currently available -> may be used in T1D or T2D patients
-
Short-acting human insulin from rDNA (dry powder); use before meals
1. Not a complete replacement for insulin therapy, but replaces meal-time injections - Admin by inhalation into lungs through the mouth using an inhaler (1-3 micron-sized insulin particles)
- Less difficult, more expensive than injected insulin; not used often, but some patients prefer it
- Obviously, not good for people with pulmonary problems
16
Q
Ketoacidosis
A
- Ketoacidosis (diabetic coma): caused by LOW INSULIN
- Catecholamines, GH, cortisol, and glucagon (all elevated in diabetes) exaggerate metabolic effects of low insulin in diabetic patient
1. INC release of fatty acids causes increased ketone bodies and decreased pH
2. Hyperglycemia bc hepatic gluconeogenesis - Treatment: INSULIN
17
Q
Hypoglycemic coma
A
- Hypoglycemic coma: usually caused by INSULIN OVERDOSE
- So common that all comatose pts given GLUCOSE first while blood glucose is being measured
- Treatment: GLUCOSE
18
Q
How are the results of a glucose tolerance test different in diabetics?
A