CBL_Hernias Flashcards
- Types of hiatus hernia
- structures involved
- how common they are (%)
Hiatus hernia
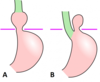
A. Sliding - 80%: gastro-oesophageal junction, cardia of the stomach move through diaphragmatic hiatus into the thorax
B. Rolling (para-oesophageal) - 20%: fundus of the stomach moves up and the stomach protrudes next to the oesophagus -> ‘bubble’ of the stomach in the thorax (peritoneal sac)
Spigelian hernia
- location
- management
Spigelian hernia
- arcuate line (lower lateral edge of rectus andominis)
Mx: urgent surgical repair due to high risk of strangulation

Obturator hernia
- anatomical location and what protrudes
- risk factors
Obturator hernia
Anatomical location: pelvic muscle floor protrudes via the obturator foramen
Risk factors:
- being a woman (wider pelvis)
- elderly
- rapid weight loss (as fat would be lost and more potential space via obturator foramen)
Signs of obturator hernia
Obturator hernia
- mass in the upper medial thigh
- features of small bowel obstruction may be present
- positive Howship - Romberg sign (due to compression of obturator nerve) *
*Howship-Romberg sign: tight extension / medial rotation and abduction -> hip and knee pain exacerbated
Littre’s hernia
- what structure does herniate?
- what’s the location?
- prognosis
Littre’s hernia
Herniation of Meckel’s Diverticulum
Location: inguinal canal
Prognosis: will often become strangulated
Two specific areas of weakness in the posterior lumbar wall that may precipitate lumbar hernias
- Superior lumbar triangle – termed Grynfeltt’s quadrangle
- Inferior lumbar triangle – termed Petit’s triangle

Lumbar hernia
- possible causes
- location
Lumbar hernia
Cause: occur following surgery - either spontaneous or iatrogenic
Location: lumbar posterior wall
Richter’s hernia
- what happens
- signs
- management
Richter’s hernia
what happens: part of the bowel/ anti-mesenteric border protrudes into the hernia and becomes strangulated
signs: tender irreducible mass, bowel obstruction (varying levels - depends on how much of the bowel is involved)
management: emergency surgery
Risk factors for hiatus hernia
A. Age - as the diaphragmatic muscle tone will decrease
B. Anything that will increase abdominal pressure: pregnancy, obesity, ascites, repeated coughing
(possible) Symptoms of hiatus hernia
- most asymptomatic
- GORD - often severe and Rx resistant
- weight loss and vomiting
- anaemia and bleeding - due to possible ulceration of the oesophagus
- hiccups and palpitations - as hernia may irritate diaphragm or pericardial sac
- swallowing difficulties - stricture formation
What may be heard on examination of hiatus hernia?
Bowel sounds in the chest (auscultation) if the hernia is big enough
What’s a gold standard investigation for hiatus hernia?
What are the characteristic findings?
Oesophagogastroduodenoscopy (OGD)
Findings:
upward displacement of gastro-oesophageal junction = ‘ Z line’

Conservative management for hiatus hernia
A. PPI e.g. Omeprazole - to reduce irritation by gastric acid and GORD - like symptoms - take in the morning before food (otherwise ineffective)
B. Lifestyle changes:
- exercise and weight loss - to reduce intraabdominal pressure
- smoking cessation and reduced alcohol intake (as they will decrease the tongue of the gastro-oesophageal sphincter)
C. Diet: low fat and small meals
D. Sleeping on increased number of pillows
Hiatal hernia - what are the indication for the surgery?
- symptomatic despite maximal medical/conservative therapy
- nutritional failure - due to gastric outlet obstruction
- danger of strangulation, volvulus - e.g. in rolling hernia
Patient presenting with the hiatus hernia
What are indications for NG tube decompression of the stomach before the surgery?
- strangulation
- stomach volvulus
- obstruction
Name (only name) two types of surgery used for hiatus hernia
- cruroplasty
- fundoplication
What does cruroplasty surgery involve?
Cruroplasty (hiatus hernia):
Hernia is reduced from the thorax into the abdominal cavity -> then the stomach is fixed to the appropriate size
What does fundoplication surgery involve?
Fundoplication (for hiatus hernia)
Gastric fundus is wrapped around lower oesophagus and fixed in place

What is incarcerated hernia?
Bowel cannot be reduced back into abdominal cavity
What’s the best diagnostic mode for an inguinal hernia?
Clinical suspicion and explorative surgery
Imaging should only be considered in patients with suspected inguinal hernia if there is diagnostic uncertainty or to exclude other pathology
What are the indications for urgent hernia surgery?
Incarcerated, obstructed and strangulated hernia
What are the two main subtypes of inguinal hernia and their prevalence? (just names and %)
A. Direct (20%)
B. Indirect (80%)
Explain direct inguinal hernia
- what structures are involved?
- cause
- epidemiology (population)
Direct: bowel enters the inguinal canal ‘directly’ through the posterior wall of the canal (Hesselbach’s triangle)
Cause: the weakness of the abdominal wall
Population: often in the elderly due to the weakness of the abdominal wall or increased intraabdominal pressure
- Which vessel is important in differentiating between types of inguinal hernias during the surgery?
- Explain
Inferior epigastric vessels
Direct hernia -> medial to the vessels
Indirect hernia -> lateral to the vessels
Indirect inguinal hernia - explain
Location: bowel enters the inguinal canal via deep inguinal ring
Cause: incomplete closure of tunica vaginalis * - congenital in origin
* tunica vaginalis is an outpouching of the peritoneum allowing testicular descent
Risk factors for inguinal hernias
- male
- obesity
- advanced age
- increased intra-abdominal pressure (heavy lifting, chronic cough and constipation)
Clinical features of inguinal hernia (the one that does not require urgent surgery)
- mass in the groin
- mass can be easily reduced (disappear) when a patient lies down
- possible mild-moderate discomfort when the patient is standing or while activity














