CBL_3 Obstructive and restrictive lung diseases Flashcards
Changes in the airways and alveoli of COPD/obstructive
Airways:
–disruption of the epithelial barrier
–poor mucociliary clearance
–infiltration of the airway walls by inflammatory cells
–deposition of connective tissue in the airway wall
–repair leads to remodelling - thickened airway walls, reduced airway diameter, and restricts the normal increase in diameter when inflating lungs
Alveoli:
–Emphysematous lung destruction is associated with an infiltration of inflammatory cells

Neutrophils in an asthmatic airway is associated with what risk factors? (3)
- sudden-onset, fatal asthma exacerbations
- occupational asthma
- patients who smoke
What happens in the asthamtic airway?
Chronic inflammation ->infiltration of inflammatory cells (neutrophils, eosinophils, mast cells, lymphocytes) -> hyper-responsivness and airflow limitation
Persistent inflammation leads to changes in the airways (on different flashcard)
Changes in asthmatic airway
–changes in airway structure
–sub-basement fibrosis
–mucus hypersecretion
–injury to epithelial cells
–smooth muscle hypertrophy
–angiogenesis

Symptoms of asthma

SYmptoms of COPD

Signs of a patient with an airway disease
Hyper-expansion
–reduced cricosternal distance
–reduced chest expansion
Wheeze
–Polyphonic
–Bilateral
Investigations for asthma/COPD
- Blood tests
FBC – eosinophil count
- Peak Expiratory Flow
Predicted based on age, gender, height
- Spirometry
Obstructive:
–Reduced FEV1
–Reduced FEV1/FVC ratio (<70%)
How does the obstructive pattern look on flow volume loop?

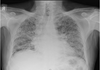
CXR of an asthmatic patient - features
–usually normal
–may be hyperinflated
CXR of a patient with COPD - features
–Hyperinflated
–May be evidence of bullae
–May be evidence of associated disease e.g. pulmonary hypertension

CT of asthma - features
–May be normal
–Gas trapping – mosaicism – in expiration

CT of COPD - features
–Emphysema
–Bullae
–May be changes of associated conditions e.g. pulmonary hypertension
What does this CT show?

Mosaicism in asthma
(air trapping on expiration)
What do these CT scans show?

Emphysema - COPD

What is it?

Emphysema
What is this?

Emphysema with bullae
Initial treatment in asthma
- Smoking cessation
- Short- acting beta-agonist
- Inhaled corticosteroids
- Education
–peak flow monitoring, inhaler technique, asthma management plan
•Influenza/pneumococcal vaccine
Initial treatment of COPD
- Smoking cessation
- Short acting beta-agonist
- Long acting muscarinic antagonist
or
- Long acting beta agonist
- Pulmonary rehabilitation
- Education
- Influenza/pneumococcal vaccine
What organisms are most likely to cause infective exacerbations of asthma?
- Most often Viral (Rhinovirus, Influenza, Respiratory Syncitial Virus
- Bacterial
Consider atypical organisms: Chlamydophila pneumoniae and Mycoplasma pneumoniae
Initial management steps of infective exacerbations of asthma
- Consider sputum culture before starting antibiotics
- Refer to local microbiology guidance
- clarithromycin & doxycycline cover atypicals
Organisms likely to cause infective exacerbation of COPD
A. Viral (approximately 30%)
•Rhinovirus, Influenza, Respiratory Syncitial Virus
B. Bacterial
•Haemophilus influenzae, Streptococcus pneumoniae, Mycoplasma pneumoniae
C. May be bacterial and viral co-infection
D. In more severe COPD consider also: Klebsiella pneumoniae, MRSA, Pseudomonas aeruginosa (PsA)
Initial treatment of acute exacerbation COPD
–Consider sputum culture before starting antibiotics
–Refer to local microbiology guidance
–Amoxicillin/Clarithromycin/Doxycycline
–Ciprofloxacin is only oral agent effective for PsA
What’s the only effective oral agent against Pseudomonas Auerginosa?
Ciprofloxacin *
*Ciprofloxacin belongs to a fluoroquinolone class
NICE guidelines management of acute COPD exacerbation (if 1st line Rx do not work)
- increase frequency of bronchodilator use and consider giving via a nebuliser
- give prednisolone 30 mg daily for 7-14 days
- Oral antibiotics ‘if sputum is purulent or there are clinical signs of pneumonia’
- oral antibiotics first-line: amoxicillin or tetracycline or clarithromycin
Treatments for acute severe asthma attack
- magnesium sulphate recommended as next step for patients who are not responding (e.g. 1.2 - 2g IV over 20 mins)
- IV aminophylline
- if no response consider IV salbutamol
Stepwise management of asthma in adults

1st line (after lifestyle advice) of management of a stable COPD
Bronchodilator therapy
- a short-acting beta2-agonist (SABA) or short-acting muscarinic antagonist (SAMA)
What should be determined for COPD patients who remain breathless after use of SABA/SAMA (1st line)?
for patients who remain breathless or have exacerbations despite using short-acting bronchodilators the next step is determined by whether the patient has ‘asthmatic features/features suggesting steroid responsiveness’
What are the criteria to determine if a patient has asthmatic features/steroid responsiveness?
Criteria NICE suggest to determine whether a patient has asthmatic/steroid responsive features:
- any previous, secure diagnosis of asthma or of atopy
- a higher blood eosinophil count - note that NICE recommend a full blood count for all patients as part of the work-up
- substantial variation in FEV1 over time (at least 400 ml)
- substantial diurnal variation in peak expiratory flow (at least 20%)
What is the 2nd step in the management (after SABA/SAMA) for a COPD patient with no asthmatic features?
No asthmatic features/features suggesting steroid responsiveness
- add a long-acting beta2-agonist (LABA) + long-acting muscarinic antagonist (LAMA)
What to add to the management* of COPD patient with asthmatic features (suggesting steroid responsiveness)?
*after 1st line SABA/SAMA were tried
COPD patient with asthmatic features/features suggesting steroid responsiveness
- LABA + inhaled corticosteroid (ICS)
- if patients remain breathless or have exacerbations offer triple therapy i.e. LAMA + LABA + ICS
- NICE recommend the use of combined inhalers where possible
When an oral theophylline Rx should be prescribed in COPD patient?
Oral theophylline
- NICE only recommends theophylline after trials of short and long-acting bronchodilators or to people who cannot used inhaled therapy
- the dose should be reduced if macrolide or fluoroquinolone antibiotics are co-prescribed
When to consider use of mucolytics in COPD?
Mucolytics
should be ‘considered’ in patients with a chronic productive cough and continued if symptoms improve
Features of cor pulmonare
Cor pulmonale
- fperipheral oedema
- raised jugular venous pressure
- systolic parasternal heave
- loud P2
Drug management of cor pulmonare
Use a loop diuretic for oedema, consider long-term oxygen therapy
ACE-inhibitors, calcium channel blockers and alpha blockers are not recommended by NICE
Risk factors for pulmonary fibrosis
- Smoking
- Family history
- Increasing age
- Men more than women
- Expose to toxins (miner, farmers, construction, ship workers, asbestosis, cotton workers, birds and animal dropping exposure)
- Connectives Tissue Disorder (sarcoidosis, SLE, systemic sclerosis, dermatomyositis and polymyositis)
- Medication (methotrexate, amiodarone, chemotherapy, nitrofurantoin, azathioprine, rituximab)
- Radiation and exposure to radiotherapy
Pathophysiology of Pulmonary Fibrosis

Important differentiation in condition causing lung fibrosis
- conditions causing predominately upper or lower zone fibrosis
* more common causes (idiopathic pulmonary fibrosis, drugs) tend to affect the lower zones
Causes of upper zone fibrosis

Causes of lower zone fibrosis
- idiopathic pulmonary fibrosis
- most connective tissue disorders (except ankylosing spondylitis) e.g. SLE
- drug-induced: amiodarone, bleomycin*, methotrexate
- asbestosis
*bleomycin - anti tumor antibiotic/ cytotoxic
What’s that?

CT scan showing advanced pulmonary fibrosis including ‘honeycombing
What happens in Intestinal Pneumonitis? (pathology)
- excessive extracellular matrix deposition
- fibroblast and myofibroblast accumulation
–between vascular and alveolar
endothelium
–disrupt normal lung structure
–“honeycomb” appearance
Symptoms of pulmonary fibrosis
- dry cough
- SOB
- weight loss (sometimes)
Signs of pulmonary fibrosis
- Finger clubbing
- Reduced chest expansion
- Fine end-inspiratory crackles
–usually bilateral
–sound like “velcro”
•Signs of an associated condition
–e.g. Rheumatoid arthritis
Ix in Pulmonary Fibrosis
•Oxygen saturations
–reduced
•Spirometry
–restrictive
–reduced FEV1 and FVC
–normal FEV1/FVC ratio
•Pulmonary function tests
–reduced lung volumes
–reduced transfer factor
Restrictive flow volume loop

Features of pulmonary fibrosis on CXR (2)
- increased interstitial markings
- reduced lung volumes
Features of Primary Fibrosis on CT
- honeycomb appearance
- traction bronchial dilatation (“traction bronchiectasis”)
- thickened interlobular septae
- reduced lung volumes

General management steps in Pulmonary Fibrosis
In general:
–assess for a cause or associated condition
–assess for oxygen
–assess for pulmonary rehabilitation
–consider symptomatic treatments e.g. morphine for breathlessness/cough
What two drugs to use for Idiopathic Pulmonary Fibrosis?
– N-acetylcysteine (but evidence limited)
– Pirfenidone & Nintedanib (nice criteria for use)
What’s Idiopathic Pulmonary Fibrosis?
idiopathic pulmonary fibrosis (IPF, previously termed cryptogenic fibrosing alveolitis)
- progressive fibrosis of the interstitium of the lungs
- idiopathic cause (e.g. not due to asbestos etc)
- IPF is typically seen in patients aged 50-70 years and is twice as common in men
- poor prognosis - usually life expectancy is 3-4 years
Clinical features of Idiopathic Pulmonary Fibrosis
- progressive exertional dyspnoea
- bibasal crackles on auscultation
- dry cough
- clubbing
Ix and results in Idiopathic Pulmonary Fibrosis
- spirometry: classically a restrictive picture (FEV1 normal/decreased, FVC decreased, FEV1/FVC increased)
- impaired gas exchange: reduced transfer factor (TLCO)
- imaging: bilateral interstitial shadowing (typically small, irregular, peripheral opacities - ‘ground-glass’ - later progressing to ‘honeycombing’) may be seen on a chest x-ray but high-resolution CT scanning is the investigation of choice and required to make a diagnosis of IPF
- ANA positive in 30%, rheumatoid factor positive in 10% but this does not necessarily mean that the fibrosis is secondary to a connective tissue disease
Management of Idiopathic Pulmonary FIbrosis
- pulmonary rehabilitation
- very few medications have been shown to give any benefit in IPF. There is some evidence that pirfenidone (an antifibrotic agent) may be useful in selected patients
- many patients will require supplementary oxygen and eventually a lung transplant
What X ray pattern would be seen in interstitial disease?
Ground glass appearance
What on spirometry would be decreased in restrictive disease?
TLCO
What’s BiPAP?
BiPAP (also referred to as BPAP) stands for Bilevel Positive Airway Pressure, and is very similar in function and design to a CPAP machine * (continuous positive airway pressure).
*CPAP is for HF
* Bi PAP for exacerbation of COPD (acidotic patients)
What drug do we need to do yearly CXR with?
Amiodarone
*SE: pulmonary fibrosis
What’s that?

Ground glass appearance
interstitial lung disease


