Anatomy Flashcards
What are the 5 vertical lines of the chest wall called?
- Midline (down centre of sternum)
- Mid-clavicular line (taken from middle of clavicle)
- Anterior axillary line (from fold of muscle at anterior of axilla = front of armpit)
- Mid-axillary line (from middle of axilla + usually widest part of thorax)
- Posterior axillary line (from fold of muscle at posterior of axilla)

What is the origin, insertion, innervation and action of the pectoralis major?
- Origin (where muscle starts) = medial third of clavicle, sternum + costal cartilages
- Insertion (where muscle ends) = humerus
- Innervation = medial + lateral pectoral nerves
- Action = adduction + medial rotation of humerus at shoulder

Which vein runs in the groove between the deltoid and pectoralis major?
Cephalic vein

What is the origin, insertion, innervation and action of pectoralis minor?
- Origin = ribs 3-5
- Insertion = coracoid process of scapula
- Innervation = medial pectoral nerve
- Action = protraction of shoulder

What is the origin, insertion, innervation and action of serratus anterior?
- Origin = upper 8 ribs
- Insertion = costal surface of scapula
- Innervation = long thoracic nerve
- Action = protraction of scapula

What is the function of the lungs?
Oxygenates blood by bringing inspired air into contact with O2 poor blood in the pulmonary capillaries
What are the two intercostal muscles? What is the innervation of the intercostal muscles?
- Gap between adjacent ribs is closed by external and internal intercostal muscles. Deep to anterior intercostal membrane, muscle fibres run at 90 degrees to external intercostal muscles = internal intercostal muscles
- Intercostal nerves

What does the internal thoracic artery branch into?
- Musculophrenic - supplies diaphragm
- Superior epigastric arteries - supplies front of abdomen

Chest cavities containing lungs are lined by pleura. What are the 2 types of pleura?
- Visceral pleura = on surface of lung
- Parietal pleura = chest wall

The central placed mediastinum has pleural cavities either side. What is the pleural cavity?
A potential space between visceral + parietal pleura

Name 2 functions of the serious fluid within the pleural cavity?
- Lubricates the pleurae
- Creates a surface tension helping the lungs to expand on inspiration
The lung is ‘connected’ to the mediastinum at the hilum of the lung. What are the 4 main structures found at the hilum of the lung?
- Pulmonary artery x1
- Bronchus x1
- Pulmonary vein x2

- How does the contraction of pectoralis major assist in breathing?
- Which bony structures lie subcutaneously in the anterior chest wall?
- What are the articulations of the clavicle?
- What forms the anterior axillary fold?
- What lies deep to the pectoralis minor muscle?
- The majority of the breast tissue is in the upper outer quadrant of the breast. Where does lymph from this part of the breast drain?
- Which costal cartilage connects to the sternum at the sternal angle (angle of Louis)?
- The two pectoralis muscles form part of a ring of muscles which encircle the thoracic cage; the other muscles forming the ring are the scapula muscles. When the ring contracts the thoracic pressure rises to assist exhalation. This only occurs in disease and during exercise; normal exhalation is a passive process.
- The clavicles and sternum (made up of the manubrium, body and xiphi-sternum). The ribs are deep to muscles so are not subcutaneous.
- At the medial end to the manubrium of the sternum; the sternoclavicular joint and at the lateral end to the acromion of the scapula; the acromioclavicular joint.
- The lower edge of the pectoralis major muscle
- The axilla
- To the axillary lymph nodes
- The second costal cartilage
What other smaller vessels are found at the hilum of the lung?
- Bronchial arteries
- Pulmonary plexus of autonomic nerves
- Lymph nodes
What branch does the right main bronchus give off outside of the right lung?
Superior lobar bronchus
Which lung are inhaled foreign antibodies most likely to be found in and why?
Right lung as right main bronchus is shorter + more vertical
How many lobes does the right lung have? What are they called? What are the two fissures?
- Superior, middle + inferior. Horizontal (extends from mid-axillary line anteriorly along 4th rib) + oblique (along 6th rib)

How many lobes does the left lung have? What are they called? What is the fissure called?
- Superior + inferior. Oblique (lies along 6th rib)

What are the 3 surfaces of the lungs?
- Costal
- Mediastinal
- Diaphragmatic

What are the 3 borders of the lungs?
- Anterior
- Posterior
- Inferior

Describe the innervation of the lungs.
- Parasympathetic innervation derived from vagus nerve
- Sympathetic innervation derived from sympathetic trunks
- Visceral afferent fibres - conducts pain impulses to sensory ganglion
What is the action of parasympathetic innervation in the lung?
Bronchonstriction and vasodilation of pulmonary vessels
What is the action of sympathetic innervation in the lung?
Bronchodilation + vasoconstriction of vessels that are poorly ventilated
What is the surface marking for the apex of the lung?
2 finger breadths (3cm) above the medial clavicle in the neck

What are the surface markings for the lower border of the pleural cavity?
8th rib anteriorly, 10th rib in mid-axillary line + 12th rib posteriorly
What are the surface markings for the lower border of the lung?
6th rib anteriorly, 8th rib in mid-axillary line + 10th rib posteriorly
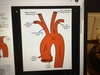
What are the 3 branches of the arch of the aorta?
- Brachiocephalic trunk
- Left common carotid artery
- Left subclavian artery

What are the branches of the brachiocephalic trunk?
Right common carotid (LHS) and right subclavian (RHS)
Where do the phrenic nerves run?
Run just under mediastinal pleura + run downwards anterior to hilum of lung + pierce dome of diaphragm

Describe the anatomical course of the right phrenic nerve.
Runs adjacent to right brachiocephalic vein + superior vena cava and along right side of heart. Crosses in front of root of lung
Describe the anatomical course of the left phrenic nerve.
Crosses arch of aorta + descends in front of root of lung
What spinal roots is the phrenic nerve derived from?
C3, 4 + 5 (cervical plexus)
What does the phrenic nerve supply?
Passes through diaphragm + innervates it with both motor (to diaphragm) + sensory fibres (to pleura, peritoneum + pericardium)
Where does the phrenic nerve enter the diaphragm?
Pierces the central tendon of diaphragm alongside IVC on right (T8)
Describe the anatomical course of the left vagus nerve.
More posterior than phrenic nerve. Crosses aorta + behind root of lung. Breaks up into branches on oesophagus + leaves thorax as anterior gastric nerve

What branch does the left vagus nerve give off as it crosses the arch of the aorta?
Left recurrent laryngeal nerve
Describe the anatomical course of the right vagus nerve.
Lies on trachea + crosses behind the root of lung. Breaks up into branches on the oesophagus + leaves the thorax as posterior gastric nerve
Does the vagus nerve enter the diaphragm? If so, where?
Yes. Through the oesophageal hiatus (T10)
What are the layers of the pericardium?
- Outer fibrous layer
- Parietal serous layer (lines pericardial cavity)
- Visceral pericardium (covers blood vessels + heart)

What are the surfaces of the heart?
- Diaphragmatic (inferior)
- Sterno-costal (anterior)
- Base (posterior)

What is the surface marking for the left apex of the heart?
5th intercostal space in the mid-clavicular line
- What is the developmental significance of the ligamentum ateriosum?
- What are the main branches of the following arteries and what organs/tissues do these vessels supply:
a) left common carotid artery
b) left subclavian artery - What are the nerve roots of the phrenic nerve? Why is this clinically important?
- What structures are supplied by the vagus nerve?
- What are the eight vessels which connect the heart to other structures?
- What is the surface marking for the apex of the heart?
- It is the remnant of a shunt between the pulmonary artery and the aorta. The shunt carries all the blood from the pulmonary artery into the aorta before the lungs have developed and most of the blood after the lungs have developed. At birth is closes so that all right ventricular blood passes to the lungs.
- (a)Left common carotid artery Internal and external carotid arteries External; Left side of the face and head Internal; most of the cerebral hemispheres (b) Left subclavian artery Vertebral, thyro-cervical, axillary Vertebral; cerebellum, brain stem, occipital lobe and the interior temporal lobe Thyro-cervical; Thyroid gland and neck Axillary; upper limb
- Cervical 3, 4 and 5. Painful diseases affecting the diaphragm are felt by the patient in the side of the neck and onto the shoulder tip which is the dermatome supplied by the cervical 3, 4, 5 nerve roots.
- Pharynx, larynx, heart, lungs, fore gut and mid gut.
- Aorta, pulmonary artery, four pulmonary veins, superior vena cava and inferior vena cava.
- 5th intercostal space, midclavicular line
- Which nerves carry sensation from the parietal and visceral pleura?
- What is a bronchopulmonary segment?
- What structures pass through the hilum of the lung?
- How does contraction of the diaphragm assist in blood returning to the heart?
- What is intercostal recession?
- Parietal pleura = spinal nerves; thoracic 1 to thoracic 12. Visceral pleura = vagus and sympathetic
- A bronchopulmonary segment has a feeding artery and bronchus which run together through the centre of the segment and repeatedly branch to reach all parts of the segment
- Main bronchus, pulmonary artery, two pulmonary veins, bronchial artery, lymphatic vessels, branches of the vagus and sympathetic nerves
- Contraction of the diaphragm decreases intra-thoracic pressure and increases intraabdominal pressure. The net effect is for blood to flow from the abdomen into the chest
- When a patient is having difficulty taking a breath in and is having to create very negative pressures in the thorax the intercostal muscles get ‘sucked in’.
What forms the right border of the heart?
Right atrium
Where is the right coronary artery found?
In the right atrioventricular sulcus. The atrioventricular sulcus (groove) separates the atria + ventricles

What are the three main branches of the right coronary artery?
- Sino-atrial nodal branch
- Right marginal branch
- Posterior inter-ventricular branch

In 90% of hearts, where does the posterior inter-ventricular artery arise?
Right coronary artery
In 30% of hearts, where does the posterior inter-ventricular artery arise?
Circumflex artery
In 20% of hearts there are two posterior interventriculs arteries? Where do these arise from?
The right coronary artery + left coronary artery
Name the three main branches of the left coronary artery.
- Circumflex
- Left anterior descending
- Left marginal artery

Where does the circumflex artery lie? What other large vessels can be found here?
Lies in left atrioventricular sulcus (groove between left atrium + left ventricle). The coronary sinus (major venous drainage of heart muscle) can also be found here, it passes posteriorly + drains into the right atrium

Where is the sinoatrial node located?
The upper aspect of the crista terminalis in the right atrium

Where is the atrioventricular node located?
Inter-atrial septum

What might damage to the posterior intraventricular artery cause?
AVN receives blood supply from posterior intraventricular artery, so disease in this may cause an electrical blockage
Name the arteries that supply:
a) the SAN
b) the AVN
a) sinoatrial nodal branch of right coronary artery
b) posterior interventricular branch, usually right coronary artery
Image of heart.

At what phase of the cardiac cycle do the coronary arteries fill?
Diastole as ventricles are relaxed
What two spaces does the crista terminalis divide in the right atrium?
It divides the trabeculated auricle from the smooth walled atrium

Where is the fossa ovalis found? What is it a remnant of?
It lies immediately above the opening for the inferior vena cava. It is remnant of the formamen ovale, which shunted blood from the RA to the LA so as to bypass the lungs in the foetus

In the ventricles, what are the chordae tendinae attached to?
The valves (tricuspid on right + mitral on left) + papillary muscles. 3 cusps on tricuspid, 2 cusps on mitral

How do the mitral and tricuspid valves work?
Open passively when the atria contract + then close afterwards to prevent backflow. Papillary muscles + chordae tendinae work to keep the valves closed during ventricular contraction
How do the atrial and pulmonary valves work?
They open passively when then the ventricles contract. Towards the end of systole they close to prevent the backflow of blood. The pressure of blood on the valves keeps them closed
How would you know if the atrial and pulmonary valves were incompetent?
You would get regurgitation of blood into the ventricles. This would be heard as a diastolic murmur
Where can you hear the pulmonary valve?
Left of the sternum, 2nd intercostal space
Where can you hear the aortic valve?
Right of the sternum, 2nd intercostal space
Describe the conducting system of the heart.
In order for ventricles to contract there has to be a system carrying an electrical impulse. Starts in sinoatrial node, then to AVN. From AVN, Purkinje fibres extend into ventricular septum + travels down to apex of heart. In ventricular septum it divides twice to provide a bundle to right ventricle + two bundles (anterior + posterior) to left ventricle
What is the blood supply of the sinoatrial node and the atrioventricular node?
- Sinoatrial node supplied by right coronary artery in 60%, supplied by left in 40%
- Atrioventricular node supplied by posterior interventricular artery
On a chest X-ray which chambers and vessels form the right and left borders of the cardiac shadow?
- Right heart border = right atrium
- Left heart border = left auricular appendage superiorly + left ventricle
What does the oesophagus run alongside? Where does it enter?
- Oesophagus runs alongside descending aorta + thoracic vertebrae + passes through diaphragm to enter abdomen level with 10th thoracic vertebra

Where does the trachea lie in relation to the oesophagus?
Trachea lies in front of oesophagus

Where is the thoracic duct found? What does it drain?
Underneath the oesophagus. Thoracic duct drains all lymph from lower half of body + bowel back into bloodstream. Drains confluence of left subclavian vein + internal jugular vein in left side of neck

What are the intercostal vessels? What are the veins called on the right and left side?
- Arteries and veins lying horizontally over vertebral bodies of thoracic duct = intercostal vessels
- Right side = azygous system
- Left side = hemi-azygous system, at least one connecting vein between them
Where does the sympathetic chain run across? What is it formed from?
- Runs across the neck of the ribs
- Formed from series of ganglia (neuron cell bodies) connected by nerve fibres (axons + dendrites)
How many ganglia are there in the thorax?
12, one for each vertebra
From the fifth to the twelfth thoracic ganglia there are nerves running over the vertebral bodies to form 3 splanchnic nerves. What do these supply?
- Splanchnic nerves supply bowel
- Greater splanchnic nerve arises from T5 to T9 + supplies foregut
- Lesser splanchnic nerve arises from T10 + T11 + supplies mid-gut
- Least splanchnic nerve from T12 supplies hind gut
What structures are supplied by the three splanchnic nerves and where does a patient appreciate pain felt by these nerves?
- Greater splanchnic nerve; fore gut, epigastrium
- Lesser splanchnic nerve; midgut, round the umbilicus
- Least splanchnic nerve; hind gut, suprapubic area
What structure lies immediately behind the trachea in the upper thorax and the left atria in the lower thorax?
What structures drain blood into the azygous system?
Lateral + posterior chest wall + lateral and posterior abdominal wall
Why is the left recurrent laryngeal nerve at risk from thoracic disease but not the right?
Left recurrent laryngeal nerve passes into thorax, round aortic arch + back into neck. Right recurrent laryngeal does not pass through thorax
Where do the sympathetic nerves attach to the central nervous system?
The thoracic 1-12 and lumbar 1 + 2 spinal segmental nerves
What happens if the sympathetic nerves to the head and neck are damaged?
No sweating on face, eyelid will drop, pupil constricted, slightly withdrawn eyeball = Horner’s syndrome, almost always affects one side
What are the muscles of the neck?
- Platysma (very thin, first layer)
- Sternocleidomastoid
- Sternohyoid
- Omohyoid
- Sternothyroid
- Thyrohyoid (in that order, identify them by their origin etc. Last 4 = infrahyoid muscles)

What is the origin of sternocleidomastoid? What is its insertion?
From the sternum (sterno) + clavicle (cleido). Inserted into mastoid process just behind ear (mastoid)

What is the origin and insertion of sternohyoid?
- Origin is sternum
- Insertion is the hyoid bone

What is the origin and insertion of the omohyoid?
- Origin = scapula (omo)
- Insertion = hyoid

What gland is revealed if the sternothyroid muscle is reflected superiorly?
Thyroid gland, in front of trachea

What is the midline connection called of the two lateral thyroid gland lobes?
Isthmus

What tracheal rings does the isthmus of the thyroid gland lie in front of?
2nd, 3rd + 4th
Where do the thyroid arteries arise from?
- Superior thyroid artery - external carotid artery
- Inferior thyroid artery - thyrocervical trunk, a branch of the subclavian artery

How many parathyroid glands are there?
- Difficult to identify
Where are the parathyroid glands located and developed?
- Located on posterior surface of thyroid glands
- Developed from pharyngeal pouches
What nerve(s) are related to the superior thyroid arteries?
External laryngeal nerves

What nerve(s) are related to the inferior thyroid arteries?
Recurrent laryngeal nerve crosses the inferior thyroid artery

Where is the carotid sheath? What vessels does it contain?
- Either side of the larynx + trachea
- Contains common carotid artery, jugular vein + vagus nerve. Common carotid artery bifurcates into internal + external carotid arteries

- What is the function of extrinsic laryngeal muscles (sternothyroid, thyrohyoid etc.)?
- Where may you create an emergency airway?
- Why does the thyroid gland have such a good blood supply?
- Which structure may be compressed by an enlarged thyroid gland?
- What is the location of the parathyroid glands and how many are there?
- What is the only complete cartilage ring around the airway?
- A patient may develop hypocalcaemia after thyroid surgery, why?
- They move the larynx up + down neck + support its central position, this is particularly important for swallowing
- Between thyroid and cricoid cartilage (cricothyroid membrane)
- Iodine is present in very low concentration in blood so gland needs high blood flow to ensure adequate delivery of iodine
- The trachea
- They are positioned on the posterior surface of the thyroid gland, there are four
- Cricoid cartilage
- Parathyroid glands may be removed during thyroid surgery which will cause acute hypoparathyroidism
What is the innervation of the intrinsic laryngeal muscles?
Recurrent laryngeal nerve
What intrinsic laryngeal muscle is not innervated by the recurrent laryngeal nerve?
Cricothyroid
What is the innervation of the cricothyroid muscle?
External branch of the superior laryngeal nerve
What is the function of the cricothyroid muscle?
Stretches + tenses the vocal cords. Important for creation of speech
Where does the pharynx open anteriorly and inferiorly?
- Pharynx opens anteriorly to nasal + oral cavity
- Pharynx opens inferiorly to larynx + oesophagus

Where does the pharynx extend from and to?
Base of skull to cricoid cartilage (C6)

What are the three sections of the pharynx called?
- Nasopharynx
- Oropharynx
- Laryngopharynx

What are the extrinsic muscles of the pharynx?
Suprahyoids, infrahyoids + stylopharyngeus

What is the function of the pharyngeal constrictor muscles?
Contract sequentially to propel food into oesophagus

What is the origin of the superior constrictor?
Pterigord plate and pterygomandibular raphe

What is the origin of the middle constrictor?
Hyoid bone
What is the origin of the inferior constrictor?
Thyroid + cricoid cartilages

What is the innervation of the pharyngeal constrictors?
Pharyngeal branch of the vagus nerve
What are the 3 longitudinal pharyngeal muscles called?
- Stylopharyngeus
- Salpingopharyngeus
- Palatopharyngeus
What is the function of the longitudinal pharyngeal muscles?
Shorten and widen the pharynx. Also elevate pharynx during swallowing

What is the origin of the stylopharyngeus and what is its innervation?
- Origin: Styloid process of temporal bone
- Innervation: Glossopharyngeal (Cn IX)
What is Killian’s dehiscence?
Weakest part of the pharyngeal wall. Located inferiorly in midline. It is the commonest site for a pharyngeal diverticulum

Which chain runs up the neck posterior to the carotid sheath? What are its three ganglia in the neck?
Cervical sympathetic chain. Prominent superior cervical ganglion (just below skull), middle cervical ganglion + inferior ganglion

What vessels are found in the carotid sheath?
- Common carotid artery
- Vagus nerve
- Internal jugular vein

Where is the carotid sinus located?
At the bifurcation of the common carotid artery

What is the carotid sinus innervated by?
Glossopharyngeal nerve
Where does the glossopharyngeal nerve exit the cranial cavity?
Through the jugular foramen

What nerve supplies sensory and taste innervation to the posterior 1/3 on the tongue?
Glossopharyngeal nerve
By following the internal carotid artery upwards and looking in the space between the artery and the mandible, lateral to the carotid sheath, what nerve should you find?
Hypoglossal nerve (Cn XII)
- What forms the ganglia on the sympathetic chains and vagus nerves?
- What is the name of the fused shirts thoracic and lower cervical sympathetic ganglia?
- What structures are supplied by the superior laryngeal nerve?
- What special sensation is carried in the glossopharyngeal nerve?
- What is the location of the carotid sinus and what sensation does it detect?
- Which structures lie immediately behind the pharyngeal wall?
- Which parts of the pharynx lie behind the lower border of the mandible?
- A collection of neuron cell bodies
- Stellate ganglion
- Sensation to the inside of the larynx down to the vocal cords + the cricothyroid muscle
- Taste from the posterior 1/3 of the tongue
- The origin of the internal carotid artery; blood pressure
- A thin layer of loose areolar tissue + then the cervical vertebral bodies
- The hypopharynx
Image of hyoid bone, thyroid notch and thyroid prominence.

What do the two cricothyroid muscles pass between? What is their function?
- Pass between the thyroid + cricoid cartilages
- Alter length + tension of vocal cords by tilting the thyroid cartilage forward on the cricoid cartilage

Make note of the soft palate, uvula, posterior 1/3 of the tongue, epiglottis and aryepiglottic folds, start of oesophagus.

What forms the laryngeal inlet?
Aryepiglottic fold + smooth walled upper larynx

What are the two folds of mucosa separated by? What are the two folds?
- Separated by deep cleft, laryngeal sinus
- Upper fold = superior vestibular (or false vocal) fold, covers a group of mucous glands
- Lower fold = ‘true’ vocal cord, formed by connective tissue + vocalis muscle

What do the superior external and internal laryngeal nerves innervate?
- External = cricothyroid muscle
- Internal = mucosa of larynx above vocal cords, via internal laryngeal nerve

What do the recurrent laryngeal nerves innervate?
Innervate all muscles of larynx except cricothyroid

Image of submandibular and parotid gland.

Name three functions of the larynx.
- Phonation
- Cough reflex
- Protection of the lower respiratory tract
What is the epithelium of the vocal folds? And why?
Stratified squamous epithelium. More robust + can withstand vibrations + wear and tear
What is the blood supply to the larynx?
Superior + inferior laryngeal arteries (branches of the thyroid arteries)
Name the three unpaired cartilages in the larynx.
- Epiglottis (elastic cartilage)
- Thyroid (hyaline cartilage)
- Cricoid (hyaline cartilage)
What do the two sheets of thyroid cartilage form in the midline?
The laryngeal prominence (Adam’s apple)
What do the inferior horns of the thyroid cartilage articulate with? How about the superior horns?
- Form synovial joint with cricoid cartilage
- Hyoid bone
What vertebral level is the inferior border of the larynx at?
C6
Name the three paired cartilages in the larynx.
- Arytenoid
- Cuneiform
- Corniculate

What do the arytenoid cartilages articulate with?
Base articulates with cricoid cartilage + apex articulates with corniculate cartilages

Where are cuneiform cartilages located?
Within the aryepiglottic folds, they strengthen them

What is the space between the vocal cords called?
Rima glottidis

What is the function of the extrinsic muscles of the larynx?
Move larynx superiorly + inferiorly during swallowing
What is the function of the intrinsic muscles of the larynx?
Control shape of rima glottidis + length and tension of vocal cords
What is the function of the cricothyroid muscles?
Stretches + tenses vocal cords, important for creation of speech
What is the function of the thyroarytenoid muscles?
Relaxes vocal ligament, allowing for softer voice
What is the function of the posterior cricoarytenoid muscles?
Abduction of vocal cords; only muscles capable of widening rima glottidis
What is the function of the lateral cricoarytenoid muscles?
Adduction of vocal cords; narrow rima glottidis
What is the function of the transverse arytenoid muscles?
Adduction of the arytenoid cartilages, narrow laryngeal inlet

What nerve passes through the parotid gland?
Facial nerve - Cn 7

What are the five branches of Cn 7?
- Temporal
- Zygomatic
- Buccal
- Mandibular
- Cervical

- Which structure stops liquid refluxing into the back of the nose during swallowing?
- Which nerve carries sensation from the larynx below the vocal cords?
- Describe the histology of the mucosa of the trachea.
- Which nerve travels through the parotid gland?
- Where do the parotid and submandibular ducts enter the mouth?
- Which nerve supplies the muscles of the tongue?
- The soft palate
- The recurrent laryngeal nerves
- Simple, columnar, pseudostratified, ciliated with goblet cells
- Facial nerve (Cn XII)
- Parotid; from cheek adjacent to second upper premolar
Submandibular; under tongue
- Hypoglossal nerve (Cn XII)
What nerve supplies sensory sensation to the anterior 2/3 of the tongue? How about taste sensation?
- Sensory sensation = trigeminal nerve, Cn 5
- Taste sensation = facial nerve, Cn 7

What folds bind to the tonsils fossa?
Palatoglossal (anterior) + palatopharyngeal (posterior) folds

What are the functions of the tonsils? What are four functions of the nasal cavity?
- Tonsils prevent infection by stopping germs entering mouth + nose
- Nasal cavity: warms + humidifies air, olfaction, removes + traps pathogens, drains + clears para-nasal sinuses
What is the function of the nasal conchae?
Increase SA of nose + disrupt fast flow of air. This means the air spends more time in nasal cavity so it can be humidified
What opens into the inferior, middle and superior meatus?
- Inferior meatus = nasolacrimal duct
- Middle meatus = frontal, maxillary + anterior ethmoid sinuses open at hiatus semilunaris. Middle ethmoid sinus opens onto ethmoidal bulla
- Superior meatus = posterior ethmoid sinus

Where does the sphenoid sinus open into the nasal cavity?
At the spheno-ethmoidal recess

What nerve supplies general sensation to the nose?
Branches of the trigeminal nerve
What vertebral level is the tracheal bifurcation?
T4

What is the function of the thoracic duct? What does the thoracic duct drain into?
- Drains all lymph from lower half of body + bowel back into bloodstream
- Drains into confluence between left jugular vein + left subclavian vein
Where does the azygous vein drain into?
Superior vena cava
What are the names of the three splanchnic nerves? What is the function of these nerves?
- Greater (T5-9), the lesser (T10-11) + the least (T12)
- They provide sympathetic innervation to the foregut, midgut + hindgut
Which artery provides the main blood supply to the left ventricle?
Left anterior descending artery

Occlusion of which vessel is most likely to result in a fatal heart attack?
Left main coronary artery

Which vessel is most likely to become occluded without producing any symptoms?
Right marginal artery
What is stenosis?
Narrowing
Which artery most frequently supplies the AVN?
Right main coronary artery

The boundaries of the abdomen are defined by six bony landmarks. What are they?
- Xiphisternum
- Costal margin
- Iliac crest
- Anterior superior iliac spine
- Pubic tubercle
- Pubic symphysis

The abdomen can be divided into 9 anatomical regions. What two vertical lines divide the abdomen into its 9 regions?
Mid-clavicular lines that extend to the mid-inguinal point

What 2 horizontal lines divide the abdomen into its 9 regions?
- Upper = subcostal = joins lower costal margins
- Lower = intertubercular = connects the iliac crests

What are the 9 regions formed?

The transpyloric plane of Addison is a useful landmark. How would you draw it? What vertebral level is it found at? What structures are found on the transpyloric plane?
- Halfway between supersternal notch + pubic symphysis
- L1
- Pylorus of stomach, gall bladder, pancreas, duodenal-jejunal flexure

How would you draw the intertubercular plane? What vertebral level is it found at?
- Joins iliac crests
- L4

What is the intercristal plane? What vertebral level is this found at and why is this important?
- Joins highest point of pelvis at the back (intertubular plane is at front)
- Between L4 + L5 vertebrae. Important for lumbar punctures + epidurals
What is the sub-costal plane and at what vertebral level does it lie? What can this level be a marker for?
- Joins lower points of costal margin
- Lies at L2
- Marker for end of spinal cord + superior mesentric artery

What is McBurney’s point? What is the significance of this point?
- 2/3 of way along a line extending from umbilicus to the right anterior superior iliac spine
- Marks base of appendix + can act as a guide for the location of caecum

Pain arising from internal organs is felt as a poorly localised, diffuse sensation and can be felt somewhere other than where the organ lies. What supplies the foregut, midgut and hindgut, and where is the referred pain felt?
- Foregut supplied by greater splanchnic nerve (arises from T5 - T9). Felt anteriorly, in midline, at T5 - T9 dermatome level, i.e. in the epigastrium
- Midgut supplied by lesser splanchnic nerve (T10 + T11). Referred to periumbilical area
- Hindgut supplied by least splanchnic nerve (T12). Referred to suprapubic area

What is a dermatome?
An area of skin supplied by nerves from a single spinal root
What are the dermatomes of the abdominal wall?
T7 to L1

If a disease process involves the peritoneum of the abdominal wall, then the pain is localised. Why is this?
The peritoneum covering the inside of the abdominal wall has the same sensory nerve supply as the overlying skin
Where the pain from disease in the diaphragm felt?
Under surface of diaphragm supplied by sensory nerves from the phrenic nerve (C 3, 4 + 5). Pain is felt in the shoulder
Where can pain in the kidney be felt?
- Sensory innervation of kidney is via the sympathetic plexus which accompanies the renal artery (T10, 11 + 12). Pain often described as radiating from loin to groin
Name the 3 flat muscles of the abdominal wall.
- External oblique
- Internal oblique
- Transversus abdominis

In what direction do the fibres of the flat muscles run in?
- External oblique - inferiorly + medially (down + in)
- Internal oblique - superiorly + medially (up + in)
- Transversus abdominis - transversely

What is origin and insertion of the external oblique?
- Origin = lower 8 ribs + thoracic-lumbar fascia
- Insertion = pubic crest, pubic tubercle, iliac crest + linea alba

What is the origin and insertion of internal oblique?
- Origin = thoracic-lumbar fascia, iliac crest, lateral 1/2 of the inguinal ligament
- Insertion = linea alba, pubic tubercle

What is the origin and insertion of transversus abdominis?
- Origin = thoracic-lumbar fascia, iliac crest, lateral 1/3 of the inguinal ligament
- Insertion = linea alba, pubic tubercle

What do we reach if we follow the external oblique forwards and downwards?
Aponeurosis of external oblique. Aponeurosis passes in front of rectus abdominis muscle to fuse with aponeurosis of the opposite side in the linea alba (white line)

What do we reach if we make an incision through the anterior rectus sheath?
Rectus abdominis muscles

What are the fibrous intersections of the rectus abdominis called?
Tendinous intersections

What are the attachments of rectus abdominis?
Rectus sheath, pubis, costal cartilages

Name 5 structures contained within the rectus sheath.
- Rectus abdominis
- Superior and inferior epigastric arteries
- Superior and inferior epigastric veins
- Nerves
- Lymphatics

What is the inferior epigastric artery a branch of?
External iliac artery

What is the internal thoracic artery a branch of? What does it supply?
Branch of subclavian artery + supplies anterior chest, abdominal wall + breasts
- What is the upper extent of the abdominal cavity?
- Describe the nerve supply to the skin of the abdominal wall.
- How is the rectus sheath formed?
- What is the surface marking of the aortic bifurcation?
- In which regions of the abdomen is pain from the three parts of the bowel felt?
- Describe the anatomy of a ‘six pack’?
- Anteriorly the under surface of the diaphragm reaches the 5th intercostal space
- Dermatomes of abdominal wall start at T5 in upper epigastrium, with T10 being at umbilicus + T12 being just above hair bearing area in lower suprapubic area. Each dermatome starts at the back at the level of the named vertebra; the dermatomes run downwards as they pass round the trunk to the front
- In upper 2/3 of abdomen the aponeurosis of external oblique muscles passes in front of rectus abdominis + aponeurosis of transversus abdominis passes behind. Aponeurosis of internal oblique sends fibres both in front + behind rectus abdominis. In lower 1/3 of abdomen all 3 aponeuroses pass in front of rectus abdominis
- Level of umbilicus
- Foregut = epigastrium, midgut = umbilical, hindgut = suprapubic
- When exercised, muscle hypertrophies, but tendons stay same. Result is 3 bulges of muscle between tendons. This occurs on either side of the midline; six bulges in all
What is the abdominal cavity lined by?
Simple squamous epithelium, the peritoneum

What are the two types of peritoneum?
- Parietal peritoneum = covers inside of abdominal wall
- Visceral peritoneum = covers the viscera (bowel + mesentery)

What is the peritoneal cavity?
A potential space between visceral + parietal peritoneum. It is filled with peritoneal fluid
What is a retroperitoneal organ?
An organ that only has its anterior surface covered by peritoneum. These organs lie behind the peritoneum
Name 6 retroperitoneal organs.
Duodenum, ascending colon, descending colon, pancreas, oesophagus, kidneys (DADPOK)

What is an intraperitoneal organ?
An organ fully covered in visceral peritoneum. It is suspended in the peritoneal cavity
Name 6 intraperitoneal organs.
Sigmoid colon, appendix, liver, transverse colon, stomach, small intestine (SALTSS)

Picture of organs.

Identify the falciform ligament.

What is the lesser omentum?
Thin fatty sheet of tissue containing blood vessels + nerves. Found if you trace the anterior wall of the stomach upwards + to the right. It attaches the lesser curvature of the stomach to and the first part of the duodenum to the liver. It extends from the diaphragm, next to the oesophagus, down to the porta hepatis

What is the porta hepatis?
Where two major blood vessels enter the liver (portal vein + hepatic artery) + bile leaves liver in bile duct

What connects the lesser sac to the greater sac?
The epiploic foramen

What is found in the right free border of the lesser omentum?
Common bile duct, hepatic artery + hepatic portal vein
What is attached to the greater curvature of the stomach?
The greater omentum

Describe the position and folding of the greater omentum in the peritoneal cavity.
It hangs down + then folds back on itself meaning there are 4 layers. The posterior 2 layers go on to enclose the transverse colon + then form the parietal peritoneum of the posterior abdominal wall
What peritoneal space lies directly behind the stomach?
The lesser sac. The only way from the greater sac to the lesser sac is through the epiploic foramen

What is it called when the peritoneal cavity becomes distended by fluid?
Ascites
Image of small intestine parts.

Organs.

- With the patient in a supine position, where might fluid collect in the abdomen?
- What embryological structure forms the ligamentum teres?
- Where does the base of the appendix lie?
- Which parts of the bowel have a mesentery?
- What structures form the portal triad?
- What is the (greater and lesser omentum)?
- Posterior to liver
- Umbilical vein, returning blood from the placenta to the liver
- 2/3 of the way from the umbilicus to the anterior superior iliac spine, McBurney’s point
- The first 1cm of duodenum, all of the jejunum and ilium, the transverse and sigmoid colon and the appendix
- Hepatic portal vein, bile duct, hepatic artery
- Sheets of tissue covered in both surfaces with peritoneum + containing fat, blood vessels, lymphatics + nerves. The greater omentum attaches to the greater curve of the stomach + the liver. The lesser omentum connects to the lesser curve of the stomach + the liver. Lesser omentum also contains portal triad entering the porta hepatis
A 65 year old gentleman comes to see you in your GP practice with a 4 week history of a dry cough that has some blood in it. You also discover whilst taking a history that his voice has become increasingly hoarse over this time. He tells you that he smokes 20 cigarettes a day and has done so for the last 50 years. You suspect he has lung cancer.
1) Describe the anatomy of the lobes of the lungs and where the lungs extend to i.e. vertebral levels
- Left lung has superior + inferior lobes. Has an area called lingula which is used to denote a projection of the upper lobe of the left lung that serves as the homologue to the middle lobe - this is a remnant of the left middle lobe. Has an oblique fissure
- Right lung has superior, middle + inferior lobe. Has horizontal + oblique fissures. Horizontal = from sternum at level of 4th rib + eventually meets the oblique fissure. Oblique = from inferior border of lung in a superoposterior direction until it meets the horizontal fissure
- Lungs extend to 6th rib anteriorly (mid-clavicular), 8th rib in mid-axillary line, 10th rib posteriorly
- Pleural cavity is commonly considered to extend to the same extent as above but +2 rib spaces i.e. 8th rib anteriorly, 10th rib in mid-axillary line + 12th rib posteriorly
2) Which nerve has been affected to cause his hoarse voice and why?
- A tumour affecting the apex of the lung (Pancoast tumour) can compress the left recurrent laryngeal nerve as it passes around the aortic arch, this results in a hoarse voice
- Pancoast tumour can also compress the sympathetic nerves in the area causing Horner’s syndrome (context)
3) Which structures are in the hila of the lung?
- Pulmonary arteries (A), pulmonary veins (V), bronchus to each lung and subdivisions (B), lymphatic vessels, branches of the vagus and sympathetic nerves
- Right = ABV
- Left = ABABV (bronchus has thickest wall)
- RALS (Right anterior/left superior) - in right hilum the artery is anterior to the bronchus, in the left hilum it’s superior to it
4) At which vertebral level does the trachea bifurcate?
- At T4 (its inferior endplate), this horizontal plane is also called THORACIC PLANE. It divides the mediastinum into superior mediastinum + inferior mediastinum
- All major bifurcations happen at vertebral level 4 (bi-four-cations). Common carotid bifurcation = C4, trachea = T4, aorta = L4
- Thoracic plane transects a few important anatomical structures:
- Bifurcation of the trachea i.e. site of carina
- Aortic arch
- Bifurcation of the pulmonary trunk
- Azygous vein drains into the SVC
- Left recurrent laryngeal nerve loops around the aortic arch
- Cardiac plexus site
Which bronchus is more predisposed to aspiration of foreign bodies? Why is this?
- Right main bronchus as it is wider, shorter + lies more vertically to the left, meaning it is easier for foreign antibodies to lodge there
A 23 year old male presents to the emergency department with shortness of breath and chest pain that occurred during his football try-outs. Upon examination, there is absence of breath and sounds in the right lower lobe of his lung and he is using accessory breathing muscle. He is otherwise healthy and has a BMI of 18. You suspect he is suffering from a spontaneous pneumothorax. You order an X-ray to confirm your diagnosis.
6) What is the innervation of the lung pleura? How does it explain the patient’s chest pain?
- Two layers of pleura have different neurovascular supply
- Parietal pleura (outermost) is innervated by the phrenic + intercostal nerves. It is sensitive to pressure, pain and temperature. It provides well localised pain - sensory innervation
- Visceral pleura (covers lungs; innermost) is innervated by pulmonary plexus (fibres derived from sympathetic fibres and parasympathetic nerve fibres from CN X) which are not sensitive to pain - autonomic innervation
7) The investigation shows a pneumothorax. What would this look like on an X-ray image? Would the affected area be light or dark?
- Pneumothorax would be indicated by a darker (hypodense) area on an X-ray. It is an absence of lung tissue and presence of air, so it appears black.
- The more solid (hyperdense) an object is, the whiter it becomes on X-ray, e.g. tumour would appear white on a chest X-ray as it is very solid and therefore hyperdense
To relieve pneumothroax you need to perform a thoracentesis.
a) Should the needle be inserted above or below the rib?
b) How does this relate to the anatomy of the neurovascular bundle of the ribs?
a) The needle should be inserted above the rib because the neurovascular bundle runs on the underside of each rib
b) Thus inserting the needle above the rib decreases the risk of injuring the neurovascular bundle
What are considered the accessory breathing muscles?
- The accessory muscles are involved in the active breathing process (where you put more effort + energy into breathing as your body is lacking oxygen)
- They act by either:
- Increasing pressure in lungs/thorax to expel air faster by decreasing the volume of the thoracic cavity = anterolateral abdominal wall muscles (external oblique, internal oblique, transversus abdominis), internal intercostal muscles, innermost intercostal muscles
- Increasing the capacity of the lungs/thorax thus decreasing the pressure, allow more air to enter the lungs = scalenes, sternocleidomastoid, pectoralis major + minor, serratus anterior, latissiumus dorsi
- These actions can be brought about by moving the ribs and sternum:
- Elevating the ribs + sternum increases the thoracic volume, thus decreasing the pressure within
- Depressing the ribs + sternum reduces the volume of the thorax, thus increasing the pressure within
- The abdominal muscles can also push the diaphragm upwards by creating an increase in intra-abdominal pressure, thus acting similarly to depressing the ribs
10) How are the intercostal muscles organised?
- External intercostals = organised obliquely and inferomedially - involved in inspiration
- Internal intercostals = organised obliquely and superolaterally - involved in expiration
- Innermost intercostals = same orientation as internal intercostals
- Subcostal muscles = in same plane as innermost intercostals, cover multiple ribs, the same orientation as internal intercostal muscles
A large embolus gets lodged in the main pulmonary artery supplying the left lung, completely blocking it. What are the likely consequences of this? What would it look like on an aterial blood gas result?
- Insufficient oxygenation (low PaO2, type 1 respiratory failure on ABG)
- The heart can’t push blood past the lodged embolus leading to high pressure + backflow into the ventricle. This can cause RV dilation causing acute heart failure
- Less blood gets to alveoli = reduction in perfusion, thus lungs divert air away from this area = V/Q mismatch
Radiology picture.

Radiology pictures.

How is the stomach attached to the liver?
- Stomach attached to liver via lesser omentum (carries hepatic artery, hepatic portal vein + bile duct)

Picture of common hepatic artery, hepatic portal vein.

What lies behind the stomach? What lies behind this structure?
- Lesser sac
- Behind lesser sac lies the pancreas, splenic artery + part of duodenum = gastric bed

What is the coeliac trunk? What are its 3 branches? What does it supply?
- Coeliac trunk = major artery that supplies the foregut, arises from abdominal aorta.
- 3 major branches = left gastric (supplies stomach), common hepatic (supplies liver) + splenic (supplies spleen) arteries
- Supplied from lower third of oesophagus to 2nd part of duodenum
- Liver + part of pancreas develop from fore gut + are supplied by branches of coeliac trunk

Where does the foregut receive its sympathetic and parasympathetic nerve supply?
- Foregut receives sympathetic nerve supply from greater splanchnic nerve (T5 - T9)
- Receives parasympathetic nerve supply from vagal trunks (X cranial nerve)
At what vertebral level does the oesophagus pass through the diaphragm?
T10

What are the parts of the stomach? What is the function of the pyloric sphincter?
- Fundus, body, antrum + pyloric regions
- Pyloric sphincter acts as a valve to control flow of partially digested food from stomach to small intestine

What vertebral level is the coeliac trunk found at?
T12
Which three major vessels emerge from behind the first part of the duodenum and run to the porta hepatis?
Hepatic portal vein, bile duct + hepatic artery
What is the blood supply to the greater curvature of the stomach?
The short gastric, and the right + left gastric-epiploic arteries.

What is the blood supply to the lesser curvature of the stomach?
Left and right gastric arteries

What is the right gastric artery a branch of?
The proper hepatic artery which arises from common hepatic artery from coeliac trunk
What is the right gastrointestinal-epiploic artery a branch of?
Terminal branch of gastroduodenal artery, this arises from common hepatic artery which arises from coeliac trunk
What is the left gastric-epiploic artery a branch of?
Splenic artery which arises from coeliac trunk
What vein does venous blood from the GI tract, liver and spleen drain into?
Hepatic portal vein (goes to liver)
Is the contraction of the stomach sphincters a sympathetic of parasympathetic action?
Sympathetic (parasympathetic = rest + digest)
What structures pass through the diaphragm alongside the oesophagus?
Vagus nerves + the oesophageal arteries and veins
What does the left gastric artery supply?
Superior part of lesser curvature of stomach
What structures lie anterior to the stomach?
Anterior abdominal wall + left lobe of liver
What nerve lies anterior to the abdominal oesophagus and which posterior?
- Left vagus (anterior)
- Right vagus (posterior)
(LARP)
With a patient in a supine (lying down) position, where might fluid collect in the abdomen?
In the right retrohepatic space
What embryological structure forms the ligamentum teres?
Umbilical vein
Which structures surround the epiploic foramen?
- Anteriorly: lesser omentum
- Posteriorly: IVC
- Inferiorly: duodenum
- Superiorly: caudate lobe of liver
What connects the jejunum to the posterior abdominal wall?
Mesentery

What parts of the large intestine are intraperitoneal?
Transverse + sigmoid colon
Define lesser sac.
Peritoneal sac that lies posteriorly to the stomach + lesser omentum. It communicates with the greater sac through the epiploic foramen
What structures lie posteriorly to the stomach?
Pancreas, diaphragm, splenic artery + vein
What vertebral levels does the stomach lie between?
T7 to L3
What are the folds of the internal stomach surface called?
Rugae

Where does the foregut begin and end?
Mouth to 2nd part of duodenum

Radiology images.

What is a porto-systemic anastomosis?
It is a vein which joins to the hepatic portal system (so can carry blood to the liver) to the systemic system. It can take blood from the bowel and bypass the liver to return the blood to the heart
What are the 3 divisions of the small intestine called?
- Duodenum
- Jejunum
- Ileum

The small bowel (intestine) is an organ of nutrient absorption and needs a high surface area. What 4 features enable it do perform this function?
Long, mucosa has multiple mucosal folds (plicae circulares), villi on mucosal folds + microvilli on each individual epithelial cell
Where are plicae circulares more pronounced?
More pronounced in jejunum than ileum
What are Peyer’s patches?
Large, sub-mucosal lymph nodules. Found on ileum
Is the duodenum intraperitoneal or retroperitoneal?
Retroperitoneal
The first part of the duodenum is prone to peptic ulceration. What artery can affect this?
Gastro-duodenal artery. This artery lies in direct contact with the posterior wall of the first part of the duodenum
What is the artery to the mid-gut?
Superior mesenteric artery, branch off aorta just below coeliac trunk. Supplies 3rd part of duodenum to 2/3 way along transverse colon (L1)

Are the jejunum and ileum intraperitoneal or retroperitoneal?
Intraperitoneal
Which part(s) of the small intestine can become twisted? This results in strangulation and ischaemia.
Jejunum + ileum
Describe 5 characteristics of the jejunum.
- Thick intestinal walls
- Longer vasa recta
- Less arterial arcades
- Pronounced plicae circulares
- Red in colour
Describe 5 characteristics of the ileum.
- Thin intestinal walls
- Shorter vasa recta
- More arterial arcades
- Peyer’s patches
- Pink in colour
Where might you find Meckel’s diverticulum? What is this an embryonic remnant of?
1 metre from termination of ileum. Embryonic remnant of attachment of mid-gut loop to yolk sac

Where does the mid-gut begin and end?
3rd part of duodenum to 2/3 along the transverse colon
What is the duodenal-jejunum flexure?
Junction between duodenum and jejunum, has a mesentery
What is the ileo-caecal junction?
Where small bowel joins large bowel (ileum and caecum)
What are the 3 major branches of the superior mesenteric artery? What do they supply?
- Ileo-colic
- Right colic (supplies ascending colon)
- Middle colic (supplies transverse colon)
Into which vein does the blood from the jejunum and ileum drain and what is the final destination of the blood?
Drains into the superior mesenteric vein. This combines with splenic vein to form hepatic portal vein which then goes on to the liver

What is the innervation of the small intestine?
Sympathetic = lesser splanchnic (T10-11). Parasympathetic = vagus
What is the main function of the large intestine?
Water absorption and formation of faeces

State whether the caecum is intraperitoneal or retroperitoneal and describe the blood supply and venous drainage.
- Intraperitoneal
- Ileocolic artery
- Ileocolic vein; drains into superior mesenteric vein
State whether the ascending colon is intraperitoneal or retroperitoneal and describe the blood supply and venous drainage.
- Retroperitoneal
- Ileocolic and right colic arteries
- Ileocolic and right colic veins
State whether the transverse colon is intraperitoneal or retroperitoneal and describe the blood supply and venous drainage.
- Intraperitoneal
- Middle colic artery
- Superior mesenteric vein

State whether the descending colon is intraperitoneal or retroperitoneal and describe the blood supply and venous drainage
- Retroperitoneal
- Left colic and superior sigmoid arteries
- Inferior mesenteric vein

State whether the sigmoid colon is intraperitoneal or retroperitoneal and describe the blood supply and venous drainage.
- Intraperitoneal
- Sigmoid arteries
- Inferior mesenteric vein

What is the marginal artery of Drummond?
An artery that forms important anastomosis between superior mesenteric artery + inferior mesenteric artery
Radiology image.

What vertebral level is the inferior mesenteric artery found at?
L3
Where does the hind gut begin and end? What is its innervation?
- Distal 1/3 of the transverse colon to anal canal.
- Sympathetic: least splanchnic nerve (T12). Parasympathetic: S2-4
What is the importance of the marginal artery of Drummond?
If there is an occlusion to the IMA, blood can still be supplied to the large intestine via the SMA through this artery
- Which vein drains blood from the colon and where does it flow to?
- Where does lymph from the small bowel drain?
- Which foodstuffs are absorbed through the lymphatic system?
- Where is the junction between the mid gut and hind gut?
- How do you distinguish a loop of large intestine from that of small intestine?
- Which part of the bowel is supplied by sacral nerves 2, 3 and 4?
- Inferior mesenteric arteries
- Into cisterna chyli + to thoracic duct
- Lipids
- 2/3 of way along the transverse colon
- Large intestine has appendices epiploicae and tenia coli. The small bowel is centrally located + colon round the sides
- Hind gut
Give 4 functions of the liver.
- Synthesis of bile
- Glycogen storage
- Clotting factors production
- Detoxification of blood

What is the liver an embryological derivative of and in which mesentery does it develop?
Derivative of the foregut. Develops in the ventral mesentery
What structures lie anterior to the liver?
Rib cage and anterior abdominal wall

What structure(s) lie superior to the liver?
Diaphragm
What structure(s) lie posterior to the liver?
Oesophagus, stomach, gall bladder, first part of duodenum (all foregut derived organs)
What aspects of the liver do the diaphragmatic and visceral surface refer to?
- Diaphragmatic = anterior superior aspects, surface smooth + convex
- Visceral = posterior inferior aspects, moulded by shape of surrounding organs so is irregular
Name the 3 liver ligaments.
- Falciform ligament
- Right and left coronary ligaments
- Right and left triangular ligaments

What is the function of the falciform ligament? What is found in the free edge of this ligament?
- Function is to attach liver to anterior abdominal wall
- Ligamentum teres (remnant of umbilical vein)
What is the function of the coronary and triangular ligaments?
They attach superior surface of diaphragm to liver
Name the 4 lobes of the liver.
- Right
- Left
- Caudate
- Quadrate

What structures bind the caudate lobe and where is it located?
- IVC + fossa produced by ligamentum venosum
- Located on upper aspect of right lobe on visceral surface

What structures bind the quadrate lobe and where is it located?
- Gall bladder + fossa produced by ligamentum teres
- Located on lower aspect of right lobe on visceral surface
What divides the liver into left and right lobes?
Falciform ligament

What supplies the liver with deoxygenated blood? How about oxygenated blood?
- Deoxygenated = hepatic portal vein
- Oxygenated = hepatic artery proper
What is the function of the gallbladder?
Temporary storage for bile
What is the storage capacity of the gallbladder?
30-50ml
What are the 3 divisions of the gall bladder?
Fundus, body + neck. Neck is where gallbladder tapers and becomes continuous with cystic duct

Briefly describe the biliary tree.
- Left and right hepatic ducts = common hepatic duct
- Common hepatic duct + cystic duct = common bile duct
- Common bile duct + pancreatic duct = hepatopancreatic amupulla of Vater

What is the orifice called where the bile empties into the duodenum?
Major duodenal papilla

What sphincter regulates the emptying of bile into the duodenum?
Sphincter of Oddi

What artery supplies blood to the gall bladder?
Cystic artery

Does parasympathetic or sympathetic innervation result in contraction of the gall bladder and the secretion of bile?
Parasympathetic
What is the arrangement anterior to posterior of the ducts, artery and portal vein at the porta hepatis?
Anterior: common bile duct, hepatic artery, hepatic portal vein
What is Calot’s triangle?
An anatomic space bounded by the liver superiorly, the cystic duct laterally + common hepatic duct medially

What is the cystic artery a branch of?
Right hepatic artery - hepatic artery proper - common hepatic artery - coeliac trunk

Where is the bare area of the liver?
Under the tendinous part of the right hemi-diaphragm. This area has no peritoneal covering

What is the surface marking for the gall bladder?
Tip of 9th costal cartilage
- Which artery is the cystic artery a branch of?
- Which structures can be found in the porta hepatis?
- What structure degenerates to form the ligamentum venosum?
- Where do the hepatic veins drain?
- Usually in right hepatic artery but can be left hepatic or hepatic artery
- Macroscopically; portal vein, right + left hepatic artery, left + right hepatic duct
- Ductus ateriosus (embryological bypass for liver which exists before liver has fully formed)
- Directly into inferior vena cava
What are the 3 major branches of coeliac trunk? What do they supply?
- Left gastric artery (supplies lesser curvature of stomach + lower oesophagus)
- Common hepatic artery (supplies liver, gallbladder, stomach, first two parts of duodenum + pancreas)
- Splenic artery (supplies pancreas, stomach + spleen)

The majority of the duodenum is retroperitoneal. What is the only part within the lesser omentum?
The duodenal cap (1st part)
What branches does the splenic artery give off?
- Short gastric arteries
- Pancreatic arteries
- Left gastroepiploic artery
- 5 branches just before it reaches the spleen

What does the left gastroepiploic artery supply? What does it anastomose with?
Supplies greater curvature of stomach. Anastomoses with right gastroepiploic artery
What do the short gastric arteries supply?
Greater curvature of the stomach
Name the 2 branches of the common hepatic artery.
- Proper hepatic artery
- Gastroduodenal artery

Name the 2 branches of the gastroduodenal artery.
- Right gastroepiploic artery (supplies greater curvature of the stomach)
- Superior pancreaticduodenal artery (supplies head of pancreas)

Name 3 branches of the proper hepatic artery?
- Right hepatic artery
- Left hepatic artery
- Right gastric artery

What does the right gastric artery supply?
Lesser curvature of the stomach
What is a branch of the right hepatic artery?
Cystic artery (supplies gall bladder)

Name the 4 divisions of the duodenum.
- Superior
- Descending
- Inferior
- Ascending

Where in the duodenum are ulcers most likely? And which artery would they affect?
Most likely in superior duodenum (1st part). If the ulcers erode through the posterior wall they may affect the gastroduodenal artery + cause haemorrhage
What does the descending portion of the duodenum lie posteriorly and anteriorly to?
Posteriorly to transverse colon. Anterior to right kidney

What vessels lie anteriorly to the inferior part of the duodenum (3rd part)?
Superior mesenteric artery + vein
Is the pancreas retroperitoneal or intraperitoneal?
Tail is intraperitoneal but rest of pancreas is retroperitoneal

Name the 5 parts of the pancreas.
- Head
- Uncinate process
- Neck
- Body
- Tail

What does the tail of the pancreas lie in close proximity to?
Hilum of spleen

Why can diseases of the pancreas spread to adjacent tissues?
Because it isn’t contained within a capsule
What is the blood supply to the head of the pancreas?
Superior + inferior pancraticduodenal arteries
What is the superior pancraticduodenal artery a branch of? How about the inferior pancraticduodenal artery?
- Superior pancraticduodenal artery = gastroduodenal artery
- Inferior pancraticduodenal artery = superior mesenteric artery
What is the blood supply to the rest of the pancreas?
Pancreatic branches of the splenic artery
What is the venous drainage of the pancreas?
Head drains into the SMV (drains into hepatic portal vein), pancreatic veins drain rest of pancreas (these drain into the splenic vein)
What is the function of the spleen?
Mainly function as a blood filter, removing old RBC’s from circulation (in adults)

Is the spleen intraperitoneal or retroperitoneal?
Intraperitoneal
What ligaments of the greater omentum connect the spleen to the stomach and kidney?
Gastrosplemic and splenorenal
How far away is the major duodenal papilla from the pylorus of the stomach?
5cm
What is the embryological significance of the major duodenal papilla?
Marks the junction between the foregut + midgut
- Can the spleen be palpated during an abdominal examination?
- What structures might the head of the pancreas involve?
- What structures join to form the common bile duct and what is its course?
- Which artery lies behind the first part of the duodenum?
- What lies between the pancreas and the stomach?
- How many pancreatic ducts are there? What is the embryological significance?
- Normally no, needs to be considerably enlarged or displaced
- Hepatic portal vein, bile duct of pancreatic duct
- Common hepatic and cystic duct. The common bile duct runs in the free edge of lesser omentum + behind the first part of the duodenum, onto the posterior of the pancreas where it enters the pancreas to run alongside the pancreatic duct before opening into the duodenum
- Gastroduodenal artery
- The lesser sac
- Two - one from ventral pancreatic bid and one from dorsal pancreatic bud
Where do the anterior 2/3 and posterior 1/3 of the tongue lie against? What supplies taste sensation to these parts? What supplies sensory sensation to these parts?
- Anterior 2/3 lies against the palate. Taste sensation = facial nerve. Sensory sensation = trigeminal nerve
- Posterior 1/3 lies against posterior wall of oropharynx. Taste sensation = glossopharyngeal. Sensory sensation = glossopharyngeal

What are the muscles of the tongue supplied by?
Hypoglossal nerve
The roof of the mouth is the palate, it separates the oral and nasal cavities. What are the two parts of the palate?
- Anterior 2/3 = hard palate
- Posterior 1/3 = soft palate, muscular

What is the function of the soft palate? What does elevation of the soft palate do?
- Soft palate controls orifice between nasal and oral parts of pharynx
- Elevation of the soft palate closes the orifice between the nasopharynx and oropharynx. This occurs during swallowing to stop reflux of food into the nasopharynx + during phonation
What folds bind to the tonsils fossa?
Palatoglossal (anterior) + palatopharyngeal (posterior) folds

What is the function of the tonsils?
Tonsils are consolidation of lymphoid tissue. They prevent infection by stopping germs entering the mouth and nose
Give 4 functions of the nasal cavity.
- Warms and humidifies air
- Olfaction
- Removes and traps pathogens
- Drains and cleans para-nasal sinuses
What are the 4 paranasal sinuses? What are their functions?
- Humidify inhaled air, increase vocal resonance
- Frontal, maxillary, ethmoid + sphenoid

What is the function of the nasal conchae?
Increase SA of nose + disrupt fast flow of air, so air spends more time in nasal cavity to be humidified. Anatomically, they divide the nasal cavity into 4 spaces
What is the inferior meatus? What opens into the inferior meatus?
Space below inferior concha, above floor of nasal cavity. Nasolacrimal duct drains into this space

What is the middle meatus? What drains into the middle meatus?
Space below middle concha, but above inferior concha. Frontal, maxillary, anterior + middle ethmoid sinuses drain into this space

What is the superior meatus? What drains into the superior meatus?
Space below superior concha, but above middle concha. Posterior ethmoid sinus drains into this space

What is the spheno-ethmoidal recess? What drains into the spheno-ethmoidal recess?
Space above superior concha, but below base of skull. Sphenoid sinus + posterior ethmoid sinus drain into this space

What is the cribriform plate?
Sieve-like sheet of bone at the very top of the nasal cavity

What is the Eustachian tube? What does it do? Where does it drain into?
- Tube between nasal cavity + middle ear cavity
- Allows air pressure to equalise in either side of the eardrum
- Drains into the posterior aspect of the nasal cavity, roughy in line with the inferior meatus
- Can get blocked by nasal oedema or mucus

What does the infra-orbital nerve supply sensation to?
Infra-orbital nerve supplies sensation to the skin over the cheek
Why does the nose have a rich vascular supply?
So it can change the humidity + temperature of inspired air
What nerve supplies general sensation to the nose?
Branches of the trigeminal nerve
Radiology picture.

- What is the function of the Eustachian tube?
- Why is the maxillary sinus more prone to infection?
- What is the nerve supply to the anterior 2/3 of the tongue?
- Where do the ducts for the submandibular salivary glands open into the mouth?
- Why may disease in the maxillary sinus cause numbness of the cheek?
- What are the attachments of the muscles of the tongue?
- What structure stops reflux of liquid into the nose during swallowing?
- To equalise air pressure either side of the tympanic membrane (eardrum)
- The opening into the nasal cavity is at the top of the sinus so it doesn’t drain easily
- General sensation = trigeminal nerve, mandibular branch. Taste sensation = facial nerve (Cn VII). Muscles = hypoglossal nerve (Cn XII)
- Below the tongue
- The nerve which gives sensation to the cheek passes in the roof of the maxillary sinus
- The hyoid bone
- The soft palate
Name the 5 superficial back muscles.
- Trapezius
- Latissimus dorsi
- Levator scapuli superioris
- Rhomboid major
- Rhomboid minor

Image of deltoid, trapezius, latissimus dorsi, teres major and teres minor.
Deltoid = top left, trapezius = top right down to middle, latissimus dorsi = bottom left, teres major = in between, teres minor = just below deltoid

What is the innervation of trapezius?
Cn 11 - accessory
What is the action of trapezius?
Elevates the scapula and rotates it during abduction of the arm
Which rhomboid muscle lies most superiorly?
Rhomboid minor lies superiorly to major. Image shows rhomboid major, rhomboid minor and levator scapulae after trapezius has been reflected

Name the 4 rotator cuff muscles.
- Supraspinatus
- Infraspinatus
- Subscapularis
- Teres minor
Image shows teres minor at the bottom, infraspinatus and then supraspinatus

What is the function of the rotator cuff muscles?
To give the shoulder joint additional stability
Where do the rotator cuff muscles originate from and insert?
Origin: scapula, insertion: humeral head
Why can posterior dislocation of the shoulder result in deltoid weakness and numb skin above the deltoid tendon?
Because it can stretch the axillary nerve
What is the insertion of the deltoid?
Deltoid tuberosity of the humerus
What is the function of the deltoid?
To abduct, flex and extend the arm
What is deltoid innervated by?
Axillary nerve
Radiology picture

What are the three heads of the triceps muscle?
Long head, medial head and lateral head. Inserted onto the olecranon process of the ulna (where the pointer is)

Image of the triceps heads.

What nerve is this?
What nerve is this?
Radial nerve
X-ray of the hand.

What is the action of the triceps?
Extension of the forearm
What are the 3 main bone groups in the hand?
- Carpal bones
- Metacarpals
- Phalanges
How many phalanges does each finger have?
3

How many phalanges does the thumb have?
2

How many carpel bones are there?
8

Where are the thenar muscles located? What is their action?
They are located at the base of the thumb. Their action is fine movements of the thumb

Name the 4 thenar muscles.
- Abductor pollicis brevis
- Flexor pollicis brevis
- Opponens pollicis brevis
- Adductor pollicis (supplied by the ulnar nerve)

Where do the abductors pollicis brevis and flexor pollicis brevis insert?
The lateral aspect of the 1st phalanx of the thumb
What is the action of opponens pollicis brevis?
It opposes the thumb by medially rotating and flexing the metacarpal
Where are the hypothenar muscles attached?
The little finger. They are mirror images of the thenar muscles

What nerve innervates the hypothenar muscles?
The ulnar nerve
Name the three hypothenar muscles.
- Abductor digiti minimi
- Flexor digiti minimi
- Opponens digiti minimi

How many lumbrical muscles are there in each hand?
4 - one associated with a finger

What is the origin and action of the lumbricals?
Origin = flexor digitorum profundus tendon, action = flexion of the metacarphophalangeal joint and extension of the interphalangeal joints

What covers the flexor tendons?
A fibrous flexor sheet that fans out into synovial sheaths

What is the importance of the synovial sheath that covers the flexor tendons?
It reduces friction in flexion and extension
What muscles group lies between the metacarpals? What are the two groups?
Interossei. Two groups = palmar and dorsal

Are the palmar interossei muscles adductors or abductors? How about dorsal interossei muscles?
- Palmar interossei ADduct = PAD
- Dorsal interossei ABduct = DAB (PAD DAB)
What are all the interossei muscles supplied by?
Ulnar nerve
What are the lumbrical muscles supplied by?
Lateral two lumbricals supplied by median nerve, medial two lumbricals supplied by the ulnar nerve
What are the LLOAF muscles? What are they supplied by?
Lateral Lumbricals, Opponens pollicis, Abductor pollicis and Flexor pollicis brevis. They are supplied by the median nerve, whereas all the rest of the muscles in the hand are supplied by the ulnar nerve
What are the 8 carpal bones called?
Scaphoid, lunate, triquetral, pisiform, trapezium, trapezioid, capitate, hamate
(Some Lovers Try Positions That They Cannot Handle)

What carpal bone are most prone to injury?
Scaphoid = most prone to fracture, lunate = most prone to dislocation
What are gyri? What are sulci?
- Gyri = rolls of cerebral cortex
- Sulci = grooves/depressions between gyri

Label this diagram.


What sulcus separates the frontal lobe from the parietal? What sulcus separates the temporal lobe from the frontal and parietal lobe?
- Central sulcus
- Lateral sulcus

What are the insula and the opercula?
- Visible when you ease the walls of the lateral sulcus
- Insula = forms the floor of the lateral sulcus
- Opercula (lips) = parts of the temporal, frontal and parietal lobes that overlie the insula

Picture of the operculum.

What divides the brain into the right and left hemisphere?
Longitudinal fissure

What white matter structure holds the hemispheres together?
Corpus callosum

Label this diagram.


More detail on maxillary bodies and the cranial nerves in the inferior aspect.

What are the functions of the parietal lobes?
Somatosensory function. The dominant lobe is involved in perception, interpretation of sesnsory information, language + mathematical operations. The non-dominant is important for visuospatial functions

What are the functions of the frontal lobe? Where is Broca’s area found and what is it important for?
- Involved in motor function, problem solving, spontaneity, memory, language etc. Anterior portion (prefrontal cortex) important for higher cognitive functions + determination of personality. Posterior portion contains motor + premotor areas
- Broca’s area found at inferior frontal gurus, important for language production
Within what lobe is Wernicke’s area located? What is its function?
- Dominant (usually left) temporal lobe
- Involved in the comprehension of written + spoken language

Where is the primary motor cortex located?
In the pre-central gyrus of the frontal lobe

What is the pre-frontal cortex responsible for?
Higher cognitive functions, e.g. personality

Where is the primary somatosensory cortex located?
In the post-central gyrus of the parietal lobe

What cortex is located in the temporal lobe?
Primary auditory cortex

What cortex is located in the temporal lobe?
Primary auditory cortex

What are the functions of the temporal lobe?
Hearing, language comprehension (Wernicke’s area). It also contains the hippocampus and amygdala

What is the function of the hippocampus?
Important in the formation of long term memories

What are the three meningeal layers?
- Dura mater
- Arachnoid mater
- Pia mater
- PAD OUT

What are two layers of the dura mater? What happens when the two layers are not fused together?
- Outer endosteal layer + inner meningeal layer. For the most part, these two layers are fused
- However, in places the inner layer separates from the skull to form dural folds. Where these dural folds attach to the skull there is a system of communicating blood filled spaces, the dural venous sinuses
Image of falx cerebri and tentorium cerebelli.

- Falx cerebri = arched crescent of dura lying in the longitudinal fissure
- Tentorium cerebelli = dura forming a thick fibrous roof over the posterior cranial fossa + the cerebellum
Image of the falx cerebelli.
- Falx cerebelli = a small, vertical, sickle-shaped reflection of dura separating the two lobes of the cerebellum

Diagram of some of the dural venous sinuses.

Diagram of some of the dural venous sinuses.

What does the sigmoid sinus drain into?
The jugular vein

Image of cavernous sinus
Contains 5 cranial nerves as well as the internal carotid artery

What are the spaces between the arachnoid space and pia mater called? What are they full of?
Subarachnoid cisterns. These are full of CSF

What are the foramen of Magendie and the foramen of Lushka?
- Foramen of Magendie = a midline communication between the IVth ventricle + the subarachnoid space
- Foramen of Lushka = a lateral communication between the IVth ventricle and the subarachnoid space
- These allow CSF to flow from the IVth ventricle into the subarachnoid spaces which surround the brain

Is the pia mater visible? Why is it important?
- No
- It forms a part of the blood-brain barrier
What is the blood brain barrier? What are the components of the blood brain barrier?
- A combination of features that limit the ability of molecules to pass between the blood and the CNS
- Components:
- Endothelial cells of the capillaries form ‘tight junctions’
- Basement membrane of CNS lack fenestrations
- Pericytes are embedded in the basement membrane + wrap around endothelial cells, they regulate capillary blood flow
- Astrocytes extend processes called end-feet that restrict flow of molecules
By which two pairs of vessels does arterial blood to the brain arrive within?
Internal carotid and vertebral arteries. Learn the circle of Willis

Another image of the circle of Willis

What do the vertebral arteries supply and what is the overall percentage? How about the internal carotid arteries?
- Vertebral arteries supply posterior cerebrum + contents of the posterior cranial fossa. About 20% of the total
- Internal carotid arteries supply the anterior + middle parts of the cerebrum and diencephalon. Supply the remaining 80%

Where does the internal carotid artery arise at the bifurcation of? What does it split into?
Internal carotid artery arises at the bifurcation of the common carotid. Divides into anterior + middle cerebral arteries

Complete this diagram of the exit foramina and the vessels that pass through them.


The cerebral veins first drain into the dural venous sinuses which are channels formed between the two layers of the dura mater. What are the two groups of cerebral veins?
- Internal cerebral veins = these run within the substance of the brain tissue + end when they reach the surface of the brain when they become external cerebral veins
- External cerebral veins = these run on the surface of the brain crossing the subarachnoid space to drain into the dural venous sinuses

Where is the majority of CSF made? Where does it then go?
- Majority of CSF by the choroid plexus (the invagination of vessels into the ventricles produces a vascular fold of pia mater = choroid plexus). The majority of the choroid plexus is located on the walls of the lateral ventricles along the choroid fissure. Choroid plexus is also present in the roofs of the third and fourth ventricles
- The CSF travels from the lateral ventricles through the foramen of Munro to the third ventricle. The fluid then flows through the cerebral aqueduct into the fourth ventricle where it drains out of the foramen of Lushka and Magendie into the subarachnoid space

How is CSF reabsorbed?
CSF is reabsorbed by the arachnoid villi located in the dural venous sinuses. Aggregations of arachnoid villi are known as arachnoid granulations


B, this infarct closely follows the boundaries of the Middle Cerebral Artery territory

D

A, this is the classic history of an extradural bleed
What are the three planes?
- Sagittal = left and right (median plane, parasagittal plane = parallel but away from midline)
- Transverse/axial = top and bottom
- Coronal = anterior and posterior

What do these terms mean:
- Rostral
- Caudal
- Dorsal
- Ventral?
- Rostral = towards front of animal
- Caudal = towards tail of animal
- Brain stem + spinal cord: ventral = anterior, dorsal = posterior
- Cerebral hemisphere: ventral = inferior, dorsal = superior
What are the three parts of the brain (encephalon)?
- Hindbrain (rhombencephalon)
- Midbrain (mesencephalon)
- Forebrain (prosencephalon)

What are the parts of the hindbrain?
- Medulla oblongata, derived from the myelencephalon
- Pons + cerebellum, both derived from the metencephalon

What are the parts of the midbrain?
- Tegmentum and tectum (mesencephalon)

What are the parts of the forebrain?
- Telencephalon (cerebral cortex, basal ganglia and limbic system)
- Diencephalon (thalamus and hypothalamus)

What is the basal ganglia?
Group of structures thought to be involved in motor function

What is the limbic system made up of?

What are the four parts of the cerebral cortex?
- Cortex = outer surface of the brain and is formed by a flatter sheet of neurones

What is the arterial supply of the brain?

What does the tectum contain?
- Tectum = DORSAL
- Contains:
- Superior collicus = visual processing
- Inferior collicus = auditory processing

What does the tegmentum contain?
- Tegmentum lies between cerebral aqueduct + the substantia nigra
- Includes the red nucleus

What do the cerebral peduncles connect together? What do they contain?
- Connect cerebrum to brainstem
- Contain tegmentum posteriorly, substantia nigra and the crus cerebri most anteriorly

What does the pons connect? What is the medulla responsible for?
- Pons connects medulla + cerebellum to cerebrum
- Medulla = responsible for several functions of the autonomic nervous system:
- Control of ventilation, e.g. ventral respiratory group
- Cardiovascular centre
- Vasomotor centre
- Vomiting, sneezing, swallowing

What is grey matter? What is white matter? What are neurones?
- Grey matter = cell bodies
- White matter = axons
In grey matter, what are the interconnected neuronal processes that occupy the space between neuronal cell bodies called?
Neutropil
What are the three fibres in the white matter?
- Association = connect components of a single hemisphere
- Commissural = connect components of a single hemisphere
- Projection = project downwards through internal capsule

What are the dorsal and ventral streams in the occipital lobe of the forebrain?
- Dorsal stream = WHERE = detect location + motion of objects; to parietal lobe
- Ventral stream = WHAT = detects colours etc; to temporal lobe

Where is the most common site for Berry aneurysm?
- Bifurcation of MCA
- Anterior communicating artery
- At the junction of internal carotid and posterior communicating arteries
- Additional point: there is no functional anastomosis between the internal carotid arteries and the vertebral arteries. This is important clinically as infarction of one area does not automatically mean that supply will be taken up by other vessels

Where can we find haemorrhages?

What are the three cranial fossa? What do they contain?

- Anterior cranial fossa = frontal lobe of brain
- Middle cranial fossa = temporal, parietal + occipital lobes
- Posterior cranial fossa = cerebellum, pons + medulla oblongata

Complete this diagram of the anterior cranial fossa.
Cribriform plate forms the roof of the spheno-ethmoidal recess

Label this diagram of the middle cranial fossa.


Label this diagram.


Label this diagram.


Label this diagram of the posterior cranial fossa.


What is this?

Hypoglossal canal

What is this?

Jugular foramen

What is this?

Internal acoustic meatus

Where do the 12 cranial nerves pass through?
1 - Olfactory = cribriform plate
2 - Optic = optic canal
- 3, 4 + 6 = superior orbital fissure. Ophthalmic division of trigeminal nerve passes through this as well
- Maxillary division of trigeminal nerve = foramen rotundum
- Mandibular division = foramen ovale
- 7 + 8 = internal acoustic meatus
- Facial nerve exits through stylomastoid foramina
- 9, 10 + 11 = jugular foramina
- 12 = hypoglossal canal
- Spinal component of the spinal accessory nerve passes into the cranium through the foramen magnum
Where do the internal carotid arteries enter the cranium?
Pass from the carotid canal, emerging and coursing superior to foramen lacecrum as it exits the carotid canal
Where do the vertebral arteries enter the cranium?
Foramen magnum
Where does the sphenoid sinus exit the cranium? What does it become?
Sigmoid sinus passes out of jugular foramen to become internal jugular vein
Image of cranial fossae.

Image of some of the major foramina.

Image of where cranial nerves pass through.

What is the orbit?
Bony structure that protects the eyeball and its associated structures

Where do the nerves pass through?
Superior orbital fissure. Frontal nerve, supra-orbital nerve, supratrochlear nerve + lacrimal nerve

What are the two branches of the ophthalmic division of the trigeminal nerve?
- Frontal nerve
- Lacrimal nerve, the nasociliary nerve comes off this
What is this?

Levator palpebrae superioris
What is this?

Superior rectus

What is this?

Lateral rectus muscle

What is this?

Inferior rectus

What is this?

Medial rectus. All the rectus muscles control the primary position of the eye

What is this? Why is it important?

Superior oblique muscle. Superior + inferior rectus will cause the eye to rotate, so this muscle corrects for this to maintain binocular vision

What is this?

Trochlear

What are these muscles supplied by:
- lateral rectus muscle
- superior oblique muscle
- all the other muscles?
- abducens nerve
- trochlear nerve
- branches of the occulomotor nerve
What is this?

Optic nerve

What is this?

Frontal nerve

What is this?

Levator palpebrae superioris

What is this?

Superior rectus muscle

What is this?

Superior oblique muscle, passes through trochlear

What is this?
Lateral rectus muscle

What is this?
Medial rectus muscle

Diagram of the orbit.

Diagram of the orbit.

What is this?

Vestibulocochlear nerve entering through the internal acoustic meatus

Diagram of the ear.








Learn this diagram.

What do these terms for eye movements mean:
a) elevation
b) depression
c) abduction
d) adduction
e) intorsion
f) extorsion?
a) moving the pupil superiorly
b) moving the pupil inferiorly
c) moving the pupil laterally
d) moving the pupil medially
e) rotating the upper part of the pupil medially
f) rotating the upper part of the pupil laterally

What do these terms mean:
a) convergence
b) divergence?
a) simultaneous inward movement of both eyes toward each other
b) simultaneous outward movement of both eyes away from each other

What are the seven extraocular muscles?
- Inferior rectus
- Superior rectus
- Medial rectus
- Lateral rectus
- Superior oblique
- Inferior oblique
- Levator palpebrae superioris

What is the origin of all recti muscles?
Common tendinous ring (annulus of Zinn)

Which muscle lifts the upper eye lid?
Levator palpebrae superioris

What do the four recti muscles do?
- Lateral rectus = pulls eye laterally (abduction)
- Medial rectus = pulls eye medially (adduction)
- Superior rectus = pulls eye superiorly, medially + rotates it
- Inferior rectus = pulls eye inferiorly, medially + rotates it

Why do we need the oblique muscles in the eye?
They prevent the eye from rotating when the superior + inferior rectus muscles contract

How do we test the eye?
- Lateral + medial rectus muscles = don’t rely on any other muscles, so tested first. Move finger from left to right, look in each eye
- Superior + inferior recti = put finger out 23 degrees on right, move up + down. This is to make them isolated. Repeat on left. If the lateral rectus muscle doesn’t work, we can’t test this
- Superior + inferior oblique muscles = can’t ever act isolated, so we position to eye to give maximal rotation + check the effectiveness of superior + inferior oblique muscles to correct rotation. Place a finger at about an arms length and go up and down, should be no rotation
What are the three branches of the trigeminal nerve?
- Opthalmic (V1)
- Maxillary (V2)
- Mandibular (V3)
What is the innervation of the seven extra orbital muscles?
Remember LR6-SO4-R3.
- Lateral rectus is 6th CN = abducens nerve
- Superior oblique is 4th CN = trochlear nerve
- Rest are 3rd CN = oculomotor nerve

What can we split the ear into?
- External ear (auricle, external acoustic meatus, directs sound waves onto tympanic membrane)
- Middle ear
- Internal ear

What are the parts of the middle ear? What are the three ear bones?
- Ear bones (remember MIS: malleus, incus, stapes)
- Pharyngotympanic tube
- Oval window
- Round window

What are the two labryinth’s within the internal ear?
Bony labyrinth + membranaceus labyrinth
What does the bony labyrinth contain?
- Lined with periosteum
- Contains perilymph
- Consists of: cochlea, vestibule + semicircular canals (lateral, superior + posterior)

What does the membranaceus labyrinth contain?
- Lies within the bony labyrinth
- Contains endolymph
- Consists of: cochlear duct, utricle, saccule + semicircular ducts (lateral, superior, posterior)

What are the three parts of the brainstem?
- Midbrain = divided into dorsal Tectum + ventral Tegmentum
- Pons = lies between midbrain + medulla
- Medulla oblongata = conical continuation of spinal cord within skull, shunning at foramen magnum. Limited above by caudal border of pons and bulbopontine sulcus

What are these parts of the midbrain called?


What are these parts of the pons?


Diagram of ventral aspect of brain stem.

Diagram of interpeduncular fossa.

What are these parts of the ventral aspect of the medulla?


What carries fibres between:
a) the midbrain and the cerebellum
b) the pons and the cerebellum
c) the medulla and the cerebellum?
a) superior cerebellum peduncle
b) middle cerebellum peduncle
c) inferior cerebellar peduncle

Diagram of the dessucation of the pyramids.

Diagram of dorsal aspect of the brainstem.

What are these on the midbrain?

Cerebellar peduncles

What are these in the midbrain? What do they do?

- Top = inferior colliculi (we are looking at the brain upside down). Part of the auditory system, concerned with reflex of loud noises
- Bottom = superior colliculi. Part of visual system, concerned with eye reflexes

What is this?

Cerebral aqueduct
What’s in front of the cerebral aqueduct? What’s behind the cerebral aqueduct?

What does the tectum contain? What does the tegmentum contain?
- Tectum = superior colliculus, inferior colliculus
- Tegmentum = lies between cerebral aqueduct and substantia nigra, includes the red nucleus

Mid-sagittal cut. Label these parts.


Diagram of colliculi.

Diagram of the midbrain.

Diagram of pons.

Diagram of the medulla.

How can we remember the medial and lateral geniculate body?
MALE. Medial geniculate body = auditory system, lateral geniculate body = visual system
Label the first ten cranial nerves.


Diagram of 11th and 12th cranial nerves.

Another diagram of the cranial nerves.

Summary of cranial nerves. Learn.

What are the component fibres of each cranial nerve?
(Some Say Money Matters But My Brother Says Big Brains Matter Most)

Where do the two optic tracts meet? What happens here?
Optic chiasm. Fibres from the lateral side stay on the same side, fibres from the medial half of the retina cross over to the opposite side

What is this? What happens here?

Lateral geniculate body (part of thalamus). The fibres synapse here
What happens after the fibres have synapses at the lateral geniculate body?
Fibres from the inferior half of the retina (superior visual field) travel through the temporal lobe (Meyer’s loop), fibres from the superior half of the retina (inferior visual field) will travel through the parietal lobe (Baum’s loop)

Diagram of different lesions in the visual pathway.











The cerebellum is the largest part of the hindbrain. What is it involved with? What are the ridges of the cerebellum called?
- Involved in coordination of movement and balance
- Ridges are called folia

What are these structures on the cerebellum?

Tonsils

What are these four structures?


What is this fissure called?

Horizontal fissure
Where is the primary fissure between?
Anterior and posterior lobes

What are these structures?

- Superior cerebellar peduncle = connection to midbrain
- Middle cerebellar peduncle = connection to pons
- Inferior cerebellar peduncle = connection to medulla

What is embedded within this white matter?

Deep cerebellar nuclei
What structure is this?
Dentate nucleus = largest + most lateral of deep cerebellar nuclei, important for movement. It’s major fibre bundles pass into the superior cerebellar peduncle
What structure is this?

Fastigual nucleus = most medial
What are these structures on the inferior surface of the cerebellum?


Diagram of the connections of the cerebellum.

What is the rest of the cerebellum called (i.e. not the vermis)?
Hemisphere

What is the dorsolateral fissure on the cerebellum?
Fissure between posterior + flocculonodular lobes

Superior surface of cerebellum diagram.

Brainstem and the floor of the 4th ventricle. Identify these structures.


Identify these structures.


What is the blood supply to the cerebellum?
- Superior cerebellar arteries
- Anterior inferior cerebellar arteries
- Posterior inferior cerebellar arteries

Label this diagram.


What is this?

Septus pellucidum
Label this diagram of parts of the diencephalon.


Label this diagram of white matter structures on the medial surface of the brain.
Corpus callosum split into 4 parts:
- Genu
- Rostrum
- Body
- Splenium

What is this?

Central sulcus, ends just before it reaches lateral sulcus
Label this diagram.


Label this diagram.


Calcarine sulcus has been cut. Label this diagram of the primary visual cortex.


What do the pre- and post-central gyrus contain?
- Pre-central gyrus contains primary motor cortex
- Post-central gyrus contains primary somatosensory cortex

Label this diagram of the ventricular system.

Responsible for production, transport and removal of CSF

Label this diagram of the posterior aspect of the IV ventricle.

Allow CSF to drain into subarachnoid spaces

What is the sheet between the corpus callosum and the fornix called?
Septus pellucidum, separates the anterior horns of the lateral ventricles

In an intact brain, what is the fluid-filled space called between the two halves of the diencephalon called?
3rd ventricle

What is the opening between the lateral and 3rd ventricles called?
Interventricular foramen, permits flow of CSF

What connects the 3rd ventricle to the 4th ventricle?
Cerebral aqueduct

What is responsible for cerebrospinal fluid production?
Choroid plexus

Different areas of the cortex are connected by myelinated axons. These form the white matter. What are they?
- Association fibres = these link cortical regions within one cerebral hemisphere
- Commissural fibres = these link similar functional areas of the two hemispheres
- Projection fibres = these link the cortex with subcortical structures such as the thalamus and spinal cord via the internal capsule and corona radiata
What are some signs of cerebellar damage?







What are the roles of the Limbic system? What is it closely related to? What is the Papez circuit?
- Limbic system = role in learning + role in regulation and translation of our emotional state into appropriate behaviour
- Closely related to the Olfactory system
- Main parts of Limbic system are connected by the Papez circuit

What are these structures?

What are these structures?


The cingulum bundle an example of what type of fibres?

Association fibres - connect different areas of cerebral cortex of one hemisphere
The internal capsule is an example of what type of fibres?
Projection fibres = between cortical and subcortical structures

What are these structures?


What are these structures?


What are these structures?


What are the parts of the lentiform nucleus?
Globus pallidus and putamen

Anterior horn of lateral ventricle and choroid plexus.

Inferior horn of the lateral ventricle and hippocampus.


This shows the anterior part of the anterior part of the lateral ventricle. What is this structure?

Head of caudate nucleus. Tail of caudate nucleus connects to amygdala

What is this white matter bundle?

Stria terminalis. Connects amygdala to septum and hypothalamus

What are the shallow grooves in the hippocampus called?

Pes hippocampi
What is this structure called? What does it thicken to form?

Fimbria. Formed from efferent fibres from the hippocampus heading to the fornix. Thickens to form the fornix

What is the hippocampus important for? What is the output of the hippocampus?
Processing of long-term memories and emotional responses. Output of hippocampus = fornix
What are these structures?


Basal ganglia structures.




What is this structure?

Amygdala

What is this structure?

Nucleus accumbens = where the caudate nucleus and putamen meet, brain’s reward system

Axial section. What are these structures?


Axial mRI.






Parasagittal diagram of brain.


Parasagittal diagram of brain.










What are the features of lumbar vertebrae?

What are the features of thoracic vertebrae?

What are the features of thoracic vertebrae (laterally)?

What are the features of cervical vertebrae?

The first and second cervical vertebrae have more extreme variation. What are their features?

What are the three curvatures of the vertebral column?

What are the two parts of intervertebral discs?
- Nucleus pulposus surrounded by an annulus fibrosus
- Nucleus pulposus = well hydrated gel having proteoglycan, collagen + cartilage cells
- Annulus fibrosus = made of 10-12 concentric layers of collagen

What is the ligament called that runs down the front of the vertebral bodies called?
Anterior spinal ligament

What is the ligament called that runs down the back of the vertebral bodies?
Posterior spinal ligament

Which ligament attaches the lamina?
Ligamentum flavum (lamina in white)

Which ligament connects the spinal processes?
Interspinous ligament

Which ligament connects the tips of the spinous processes?
Supraspinous ligament

We have removed the erector spinae muscles to reveal the vertebral column. What is this space called?
Epidural space = the ‘space’ between the vertebrae + dura mater of the spinal cord. It contains small arteries which supply the spinal cord and the vertebral venous plexuses

Diagram of muscles and fasciae of the posterior abdominal wall.

If we cut through the arachnoid mater, what is revealed?
Spinal cord

What is the conus medullaris? What is the filum terminale?
- Tapering end of the spinal cord
- A fibrous strand extending from the conus medullaris to the coccyx

What is this structure called?

- Cauda equine = sensory and motor nerves from the lower part of the cord, the lumbar and sacral nerves, hanging obliquely downwards

What are these structures called?

Dorsal root ganglion - cell bodies of sensory neurons entering spinal cord

Diagram of spinal nerves.

What is the spinal cord comprised of?

Diagram of main tracts of the spinal cord.













What are the movements of the vertebral column?
Forward flexion (40 degrees), extension (15 degrees), lateral flexion (30 degrees) and rotation (40 degrees)
What are intervertebral discs?
Strong fibrocartilagenous structures that can withstand compression forces but are flexible enough to allow movements between the vertebrae
Where does the spinal cord end?
- Spinal cord ends at the interval between the first and second lumbar vertebrae
What is the spinal cord segment?
Area of the spinal cord from which a pair of spinal nerves are given off. The spinal cord has 31 pairs of spinal nerves and hence 31 segments: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral + 1 coccygeal
The spinal nerve level is named from the vertebra above which it leaves the intervertebral foramina. What does this apply to?
- Cervical 1-7
- Thoracic and lumbar exit below their numbered vertebra
What is the inguinal canal?
An oblique passage through the muscles of the anterior abdominal wall. Contents of the inguinal canal consist of the spermatic cord and ilioinguinal nerve (males). Extends from deep inguinal ring to the superficial ring. In both sexes it contains the ilio-inguinal nerve

What is the deep inguinal ring protected by?

Fibres of internal oblique

Can we see the components of the inguinal canal?
No, they are surrounded by a layer of fascia

Where is the spermatic cord formed? What structures does it contain?
- Structures passing through the inguinal canal run from the deep inguinal canal, along the inguinal canal, out of the superficial inguinal ring and down into the scrotum. After leaving the superficial ring there will be three fascia layers, this marks the start of the spermatic cord
- Spermatic cord contains vas deferens, testicular artery, pampiniform plexus of veins, the nerves and lymphatics of the testis and the processes vaginalis
- Vas deferens shown (carries sperm from testis to penis)

What is this structure?

Vas deferens (carries sperm from testis to penis)

What are the three layers of fascia around the testis?
These are pushed through during the movement of the testis from the abdomen during development:
- External spermatic fascia
- Cremasteric fascia
- Internal spermatic fascia

What are the arteries, veins and nerves of the testes?
Arteries:
- Testicular artery
- Vas artery
- Cremasteric artery
Veins:
- Testicular vein
- Vas vein
- Cremasteric vein
Nerves:
- Genitofemoral
- Ilioinguinal
- Sympathetic

What is the testis? What is it surrounded by?
Testes = main male reproductive organs. Covered by three layers of fascia (same as spermatic cord). Partially surrounded by safe derived from peritoneum called tunics vaginalis. The testicular artery and pampiniform plexus of veins may be found entering + leaving the upper pole of the testis

What is the hard part of the testis called?
Epididymis

Diagram of epididymis.


Where does the vas deferens begin?
Starts at the tail of the epididymis and travels up alongside the testis to run with the testicular vessels in the spermatic cord

What is the scrotum?
Pendulous pouch of skin containing the testes, epididymis and lower part of spermatic cord. Scrotal skin is a thin layer of superficial fascia devoid of fat. Superficial fascia extends between the testicles to form a septum dividing the scrotum into right + left halves
What fascia surrounds the penis?
Buck’s fascia

What is this piece of skin called?

Foreskin

The main shaft of the penis is formed from three cylinders of erectile tissue? What are they?
- Two corpora cavernosus
- Copus spongiosus
What is the glans penis formed from?
Corpora spongiosus

Diagram of the three erectile tissue.
- Corpora spongiosus causes penis to become erect
- Corpora cavernosus cause the penis to become hard

What is the superficial inguinal ring?
Lower fibres of external oblique aponeurosis form a triangular gap above + medial to the pubic tubercle
What is a hernia? What are the two types?
- Inguinal canal provides a route from inside of abdomen to external genitalia (both sexes). Common for abdominal contents to pass through the inguinal canal to form a hernia
- Two types of inguinal hernia:
- Indirect = hernia passes along length of canal + passes through each of three layers of abdominal wall at a different position
- Direct = if it passes through transversus fascia of posterior wall, directly through internal oblique layer and directly through external ring
Complete this diagram of the pelvis.


Diagram of peroneum.


What is the triangle between the ischial tuberosities and the coccyx called?
Ano-rectal triangle

What is the column of erectile tissue called?
Crura cavernosus

How many bodies of spongiosus are there in females?
Spongiosus is in 2 bodies of erectile tissue separated by the interoitus
What is the hair bearing bulge which sits over the erectile tissue called in females?
Labia majora

Anterior to this line, what is the skin supplied by? How about posteriorly?

- Anteriorly = L1 ilioinguinal nerve
- Posteriorly = S2 sacral nerve
Which nerve supplies the peroneum?
Peudendal nerve (branch of sacral roots 2, 3 + 4). Comes out of the greater sciatic foramina with the sciatic nerve, enters lesser sciatic foramina to supply posterior 2/3 of external genitalia + area of skin off central buttocks and anal canal









What is this gland? What is the difference between the left and right glands? What is their blood supply and drainage?

- Adrenal gland/suprarenal gland
- Right adrenal gland = tetrahedral and lies behind liver and inferior vena cava
- Left adrenal gland = crescent-shaped and lies behind stomach and pancreas
- Both supplied by three arteries (one from renal artery, one from the aorta and one from an artery to the diaphragm) and drained by renal vein

What is this structure? What does their hilum contain? What are the left and right structures related to anteriorly? How about posteriorly?

- Kidney. Lie outside peritoneum (extra-peritoneal) and behind peritoneal cavity (retro-peritoneal)
- Renal hilum = where renal vessels, nerves, lymphatics + ureter enter or leave the kidney. Renal vein lies most anteriorly, artery immediately behind and ureter most posteriorly
- Anteriorly, right kidney and perinephric fat related to liver, duodenum and coils of intestine. Left kidney and perinephric fat related to stomach, spleen, pancreas and coils of intestine
- Posteriorly, perinephric fat and kidneys are related to muscles of posterior abdominal wall, including the diaphragm, psoas major, quadratus lumborum and the transversus abdominis



Label this diagram of the kidney.

- Tips of medullary pyramids = minor calyx, two or three minor calyx fuse to form major calyx, all major calyces fuse to form renal pelvis which narrows down to become the ureter

Label this diagram.


What is this muscle called?

Quadratus lumborum



What does the aorta bifurcate into?
Common iliac arteries which bifurcate into internal iliac artery and an external iliac artery





Label this diagram.


What nerve is this?

Femoral nerve
What nerve is this?

Genito-femoral nerve
Label this diagram.


What is this nerve?

Lateral cutaneous nerve
What does the pubic bone consist of?


What does the ischium consist of?


What is this?


Complete this diagram.


What is this plane called?

Inter-tubercular plane
What is this plane called?

Intercristal plane
What joint is this?

Sacro-iliac canal
Complete this diagram.


Complete this diagram.


Which nerve passes through here?

Sciatic nerve
Complete this diagram.


What is the first difference between the male and female pelvis?

What is the second difference between the male and female pelvis?


What is the third difference between the male and female pelvis?


Complete this diagram.


Complete this diagram.


What happens when the bladder expands?

Peritoneum comes off the abdominal wall and bladder comes into direct contact with the rectus abdominis muscle

Complete this diagram.


What are the four surfaces of the bladder?
Superior, two laterals and base
What is the bladder lined by?
Rugose

On the base of the bladder, what is on this ridge of tissue?
Orifice for the ureters

What is this area of mucosa called?

Trigone

Complete this diagram.






What is this? What does it do?

Seminal vesicles, secretes thick alkaline fluid which forms the bulk of seminal fluid. Sperm are stored in epididymis
Vas deferens and duct coming from seminal vesicle join prostate. There is then a short common duct through the posterior part of the prostate into the urethra. What is this called?

Ejaculatory duct
What is this plexus of veins surrounding the prostate called?

Prostatic plexus of veins, there are no valves in this venous system

As the prostate surrounds the urethra, what happens if the prostate enlarges?
Cuts off urethra
Complete this diagram.


What are the terms for when the junction between the body and the cervix are tilted forwards or backwards? How about when the body of the uterus is bent forwards or backwards?
- Ante-verted, retro-verted
- Ante-flexed, retro-flexed
What is the uterus divided into?
Fundus, body and cervix
Complete this diagram.


Complete this diagram.


Complete this diagram.


The Fallopian tube gets wider towards its end (the infindibulum). What does it finish in?
Fimbrae = lots of finger-like projections

What is this called?

The ovary. Always sits on the back of the broad ligament
Whwt is the ovary attached to the uterus by?

Round ligament of the ovary

Which ligament enters the deep inguinal ring and then carries on to the labia majora?

Round ligament of the uterus

What is this nerve called?

Obturator nerve
What is this artery called?

Uterine artery, comes off internal iliac artery and feeds onto lateral wall of uterus. Ureter runs directly underneath uterine artery
Which ligaments hold the cervix in its midline position and stop it from falling downwards?
Cardinal ligaments




What is this?

Pectoralis major
What is this?

Pectoralis minor
What is this?
Clavicle

What is this?

Acromioclavicular joint

What is this?

Supraclavicular fossa

What is this?

Platysma

What is this?
Sternocleidomastoid

What is this?

Internal jugular vein
What is this?
Common carotid artery

What is this tunnel called? What does it do?

Axilla, transmits the nerves and blood vessels to and from the upper limb
What is this?

Top end of the humerus

What is this? What does it drain into?

Cephalic vein, this drains into the axillary vein

Label this diagram.


What are the boundaries of the axilla?
- Anterior wall = pectoralis major + pectoralis minor
- Posterior wall = subscapularis, teres major + latissimus dorsi muscles
- Lateral wall = upper end of the humerus with the biceps brachii + the coracobrachialis muscles
- Medial wall = the serrated anterior muscle covering the ribs and the intercostal spaces
- Apex = formed by the 1st rib medially with the clavicle and scapula behind, it is the channel of communication between the posterior triangle of the neck and the axilla
- Base = skin and fascia extending between the chest wall and the arm

What does the axilla contain?
- Fat and lymph nodes
- Axillary artery which is the major artery supplying the upper limb
- Axillary vein = the major venous drainage of the arm
- Brachial plexus = nerve plexus supplying the limb

What is the clinical importance of the lymph nodes in the axilla?
They drain lymph from the upper limb, chest wall (front and back) and the abdominal wall as far as the umbilicus
Where does the brachial plexus arise from?

C5, C6, C7, C8 and T1 through the intervertebral foramina
- Read That Damn Cadaver Book = roots, trunks, divisions, cords, branches
- Branches of the brachial plexus (superior to inferior) = Most Alcoholics Must Readily Urinate = musculocutaneous, axillary, median, radial, ulnar
What nerve is this?

Phrenic nerve

What is this? What happens behind this?

Scalenus anterior, it is from behind this that the roots of the brachial plexus arise to enter the axilla

What is this?

Subclavian artery

What is this?

Scalenus anterior

What is this?

Phrenic nerve

What is this?

C5 nerve root

What is this?

C6 nerve root

What is this?

C7 nerve root

What is this?

C8 nerve root

What is this?

T1

What do C5 and C6 nerve roots form?
The upper trunk

What does C7 form?
The middle trunk

What do C8 and T1 form?
The lower trunk

Complete this diagram. What is the axillary artery the blood supply to?

Axillary artery is the blood supply to the upper limb

What does the posterior cord give rise to?
Radial nerve and axillary nerve

What does the lateral cord give rise to?
Musculocuataneous and a lateral part which will become the median nerve

What does the medial cord split into?
Ulnar nerve and the medial part of the median nerve

What is this?

Cephalic vein, runs in the groove between the anterior compartment and the posterior compartment

What is this?

Antecubital fossa

What is this? What does this become?

Basilic vein, joins the artery to become the brachial vein –> axillary vein –> subclavian vein –> brachiocephalic vein –> superior vena cava

Which nerve runs between the biceps muscle and the brachialis muscle? What does this supply?

Musculocutaneous nerve, this supplies the anterior compartment of the arm

What is the origin of the long head of the biceps muscle?

Superior aspect of the glenoid fossa

What is the origin of the triceps muscle?
Inferior aspect of the glenoid fossa
What is the origin of pectoralis minor? What else has its origin here?

Coracoid. The short head of the biceps muscle also has its origin here along with the coracobrachialis muscle

Complete this diagram.


Picture of the antecubital fossa. Complete the diagram.


Complete this diagram.








Radiology picture.


Diagram of veins in the anterior forearm.


What is this?

Pronator teres

Complete this diagram.

- Remember PFPF (lateral to medial): pronator teres, flexor carpi radialis, palmaris longus and flexor carpi ulnaris
- Flexor carpi ulnaris is the only one to be innervated by the ulnar nerve, the rest are innervated by the radial nerve

What is this?

Flexor digitorum superficialis

What is this? What is it supplied by? What are the deep anterior forearm muscles?

- Flexor digitorum profundus
- Lateral half supplied by the median nerve and the medial half is supplied by the ulnar nerve
- Deep anterior forearm muscles = flexor digitorum profundus, flexor pollicis longus, and pronator quadratus

What is this?

Flexor pollicis longus

What is this?

Pronator quadratus

Which nerve is this?

Median nerve

What is this?

Ulnar artery and nerve

Which artery is this?

Radial artery

What is this?

Cephalic vein

What is the anterior compartment of the arm applied solely by?
Musculocutaneous nerve
What are the posterior compartment of the arm and the posterior compartment of the forearm supplied by?
Radial nerve
Which two nerves is the anterior compartment of the forearm supplied by?
- Majority = median nerve
- Flexor carpi ulnar is and medial 1/2 of flexor digitorum profundus
Summary of the nerve supply of the muscles of the upper limb.






What is this?

Tibial plateau
What is immediately under the subcutaneous fat? What does this split the thigh into?
Fascia lata, this splits the thigh into three compartments: anterior, medial and posterior

What is this muscle? Where does it run from and to?

Sartorius, runs from the anterior superior iliac spine, across the front of the thigh, down the medial aspect of the thigh and attaches to the tibia
What is this? What does it do?

Tensor fascia lata, it tenses fascia lata
Which quadriceps muscle is this?

Rectus femoris
Which quadriceps muscle is this?

Vastus lateralis
Which quadriceps muscle is medial to rectus femoris?

Vastus medialis
Which quadriceps muscle is deep to rectus abdominis?

Vastus intermedius
What is the origin of the three vastus muscles?
Femur
What are the two origins of rectus femoris? What are the two heads?
Pelvis:
- Directly above the hip joint on the lip of the acetabulum
- Other is slightly lateral to this
- This means that there is a reflected and straight head of rectus femoris
What happens when rectus femoris contracts? What is the role of the three vastus muscles?
- Flexes the hip and straightens the knee
- Vastus muscles extend the knee
Complete this diagram.


Complete this diagram.

The knee is bent inwards, a valgus direction. It changes the movement of the patella (laterally) when the quadriceps muscles contract

Which two mechanisms prevents the patella from dislocating when the quadriceps muscles contract?

- Medial fibres of vastus medialis - these contract and counteract the movement = active mechanism
- Lateral groove for patella is much more prominent than the medial part = passive mechanism

Which vein is this?

Long saphenous vein
Complete this diagram.


Which muscle is this at the floor of the femoral triangle?

Pectoneus muscle
Which muscle is this?

Iliopsoas muscle (fibres from the iliacus muscle)
Complete this diagram.


Complete this diagram.


Which muscle is this?

Femur adductor brevis
Which nerve is this?

Obturator nerve
What are the two origins of adductor magnus? What are its insertions?
- Pubis bone and ischial tuberosity
- Pubic component inserts onto the shaft of the femur, the hamstring portion inserts onto the adductor tubercle on the medial condyle of the femur
What is this ‘v’ shaped defect called?

Adductor hiatus
What is this?

Superficial femoral artery (vein is below it)
Which muscle is this?

Pectineus
Which muscle lies underneath adductor longus?

Adductor brevis
Which nerve is this? Where does it arise from?

Obturator nerve, arises from the obturator canal
Radiology picture that demonstrates how the lateral groove is larger than the medial groove.




What is the anterior compartment of the leg supplied by?

Anterior tibial artery and the deep peroneal nerve
What is the lateral compartment of the leg supplied by?

Peroneal artery and the superficial peroneal nerve
What is the posterior compartment of the leg supplied by?
Posterior tibial artery and the tibial nerve
What is this? What does it do?

Extensor retinaculum, holds the tendons against the ankle joint
What is this? What is it connected to medially and laterally?

Anterior compartment fascia, connected to the tibia medially + the fibula laterally
What is this?

Lateral malleolus
What is this? Where does it extend from and to?

Peroneus longus, goes from the top of the fibula to attach to the base of the first metatarsal
What is this muscle? What does it attach to?

- Peroneus brevis
- Attaches to the base of the fifth metatarsus
What are peroneus longus and peroneus brevis supplied by? What is their action?
Superficial branch of the peroneal nerve, they flex the ankle joint

What is this?

Head of the fibula
Which nerve is this?

Common peroneal nerve
What does the common peroneal nerve go into? What does this then become?

Superficial peroneal nerve, this then becomes the cutaneous branch supplying the lateral aspect of the foot
Which nerve is this?

Deep peroneal nerve
What does the common peroneal nerve supply?
All the muscles which lift the foot and toes up
Complete this diagram.


What are the anterior muscles of the leg supplied by?
Deep branch of the peroneal nerve and blood supply is the anterior tibial artery

What lies between extensor hallucis longus and extensor digitorum? What is this a continuation of?
- Dorsalis pedis pulse = blood vessel
- Continuation of the anterior tibial artery (1st division of the popliteal artery, peroneal is also a branch of the peroneal artery)

Diagram of the anterior compartment of the leg.


Diagram of the foot muscles.






Label this diagram.


What is this?

Ischial tuberosity
What are these structures?

Inferior gluteal vessels and nerves
What is found here?

Superior gluteal vessels and nerves
What is the origin of gluteus maximum?

Sacrum, iliac crest and the sacrotuberous ligament

What is the insertion of gluteus maximus?
Ileo-tibial tract

What is this nerve?

Sciatic nerve
What passes through the greater sciatic foramina?
Sciatic nerve and piriformus muscle

What is this muscle?

Piriformus
What is this?

Ischial tuberosity
What is this muscle?

Gluteus medius
What is this muscle?

Quadratus femoris
What is this muscle?

Superior gemellus
What is this muscle?

Inferior gemellus
What runs between inferior gemellus and superior gemellus?
Obturator internus
What can we see underneath gluteus medius?

Gluteus minimus
What is the innervation of gluteus maximus, gluteus medius, and gluteus minimus?
- Gluteus maximus = inferior gluteal nerve
- Gluteus medius = superior gluteal nerve
- Gluteus minimus = superior gluteal nerve

What are the actions of gluteus maximus, gluteus medius, and gluteus minimus?
- Gluteus maximus = extends thigh during exercise
- Gluteus medius = abducts and medially rotates lower limb
- Gluteus minimus = abducts and medially rotates lower limb

What is a pelvic drop?
- Both gluteus medius + minimus have an important role in stabilising the pelvis during walking
- If the superior gluteal nerve which supplies them is injured, it results in a pelvis drop

What is a Trendelenburg test?
Involves asking the patient to stand on each leg unassisted. If the test is positive, pelvic drop will be seen on the unsupported leg and is suggestive of superior gluteal nerve injury

What is the innervation and action of the deep gluteal muscles?

Why is the piriformus muscle an important landmark in the gluteal region?
- It travels through through the greater sciatic foramen which means it divides the region into a superior and inferior portion
- This is important as it forms the basis of why the superior and inferior gluteal nerves are named accordingly. Also, piriformus is useful to locate the sciatic nerve

What are the parts of the femur?

What is the socket that the head of the femur sits in called?
Acetabulum

What are the posterior thigh muscles collectively known as? What are they innervated by? What do they do?
- The hamstrings
- Innervated by the sciatic nerve
- Act to extend the hip and flex the knee

What is this muscle?

Biceps femoris

What is this muscle?

Semitendinosus
What is this muscle?

Semimembranosus
What is this muscle?

Adductor magnus
What is this nerve? What does it split into?

Sciatic nerve, splits into tibial nerve (above) and common peroneal nerve (below)
What are the actions of biceps femoris, semitendinosus, semimembranosus and the posterior portion of adductor magnus?
- Biceps femoris = flexes the knee
- Semitendinosus = flexes knee and extends hip
- Semimembranosus = flexes knee and extends hip
- Posterior portion of adductor magnus = mixed action, but generally helps to extend the hip

What forms the superomedial and superolateral border of the popliteal fossa?
- Superimedial border = semimembranosus
- Superolateral border = biceps femoris

What are these muscles?

- Gastrocnemius (medial head)
- Gastrocnemius (lateral head)

What makes up the inferomedial and inferolateral border of the popliteal fossa?
- Inferomedial border = medial head of gastrocnemius
- Inferolateral border = lateral head of gastrocnemius and plantaris

Complete this diagram.


Complete this diagram.

What are the contents of the popliteal fossa?
- Popliteal artery
- Popliteal vein
- Tibial nerve
- Common fibular nerve (common peroneal nerve)



Which nerve lies next to biceps femoris?
Common peroneal nerve

What is this muscle?

Which structures pass between the lateral and medial heads of gastrocnemius?

Popliteal artery, popliteal vein and tibial nerve
Which muscle lies below the lateral head of gastrocnemius?

Plantaris
Which muscle is this?

Soleus
What is this structure?


What is this muscle?

Popliteus
What are these two muscles?

- Fibrularis longus (white)
- Fibrularis brevis
What are the actions of fibrularis longus and fibrularis brevis? What do the lateral leg muscles do? What are they innervated by? What is their arterial supply?
- Fibrularis longus = plantarflexes and everts foot
- Fibrularis brevis = everts foot
- Lateral leg muscles evert the foot
- Innervated by superficial fibular nerve
- Arterial supply = fibular artery

What muscle is this?

Flexor hallucis longus
What is this muscle called?

Flexor digitorum longus
What muscle is this?

Tibialis posterior
Which artery is this?

Posterior tibial artery (along with vein and nerve)
What are the actions of the posterior leg muscles?
- Gastrocnemius = plantarflexes ankle and flexes the knee as it crosses if
- Plantaris = plantarflexes ankle and flexes the knee as it crosses it
- Soleus = plantarflexes ankle
- Popliteus = laterally rotates femur on tibia (unlocks knee)
- Tibialis posterior = inverts and plantarflexes foot
- Flexor digitorum longus = flexes lateral 4 toes
- Flexor hallucis longus = flexes big toe

What are the posterior leg muscles innervated by? Where do they receive their blood supply from?
- Innervated by the tibial nerve
- Arterial supply from the posterior tibial artery

Why is soleus known as the main skeletal muscle pump?
Soleus surrounds big veins in the leg so when it contracts it forces blood back towards the heart

What makes up the superficial group of posterior leg muscles?
Gastrocnemius, plantaris and soleus

How is the tarsal tunnel formed?
A band of flexor retinaculum lies over the medial malleolus of the ankle and forms the tarsal tunnel

Which 6 structures pass through the tarsal tunnel?
(Remember ‘Tom Dick And Very Naughty Harry’)
- Tibialis posterior tendon
- Flexor digitorum longus tendon
- Posterior tibial artery
- Posterior tibial vein
- Tibial nerve
- Flexor hallucis longus

What happens if the tarsal tunnel compresses the tibial nerve?
Causes tarsal tunnel syndrome


What is this?

Flexor hallucis longus
What are these?

4 tendons of flexor digitorum longus
Complete this diagram.


What are the 3 groups of bone in the foot?




What are the posterior forearm muscles?
- Remember: Big Chocolate Chips Double Dip Cherries
- Brachioradialis
- Extensor carpi radialis longus and brevis
- Extensor digitorum
- Extensor digiti minimi
- Extensort carpi ulnaris
- Anconeus

What are the posterior forearm muscles all innervated by?
Radial nerve
What are the actions of the superficial posterior forearm muscles?

What are the deep posterior forearm muscles?
- Remember: Syrup And Peanuts Preferably Included
- Supinator
- Abductor pollicis longus
- Abductor pollicis longus and brevis
- Extensor indicis

What are the actions of the deep posterior forearm muscles?

When does wrist drop occur?
When the radial nerve is damaged, resulting in paralysis of the extensor muscles so there is unopposed flexion of the wrist, the 2 most common causes are shoulder dislocation or a humeral shaft fracture

What are the thenar muscles? What is their action? What are they innervated by?

What are the hypothenar muscles? What are their actions? What are they innervated by?

Where does adductor pollicis lie? What is its action? What is it innervated by?
- Adductor pollicis sits in the palm
- Adducts the thumb
- Innervated by ulnar nerve

What are the lumbrical muscles? What are their actions? What are the lateral lumbricals supplied by? How about the median lumbricals?

What are the two sets of interossei muscles? What are their actions? What are they all innervated by?

Which hand muscles are supplied by the median nerve?

What are the nail beds generally supplied by?
Median nerve

What does damage to the median nerve cause? What does damage to the ulnar nerve cause?

What are the borders of the anatomical snuffbox? What are the contents?

Where is pain felt if we damage the scaphoid? Why is this important?

In carpal tunnel syndrome, which nerve is affected?
Median nerve

What is a Colles’ fracture? What are scaphoid and Colles’ fracture usually a result of?
- Colles’ fracture is a very common fracture of the distal radius that is associated with osteoporosis
- Both scaphoid and Colles’ fractures commonly occur as the result of falling over and landing on an outstretched hand

What are the borders of the antecubital fossa? What are its contents?

What is the most common site for venipuncture?

What are the bones of the elbow?

What is the olecranon an important attachment for? Why is hitting the olecranon very painful?

What are the carpal ‘wrist’ bones?
- Remember: Some Lovers Try Positiosns That They Cannot Handle
- Scaphoid
- Lunate
- Triquetrum
- Pisiform
- Trapezium
- Trapezoid
- Capitate
- Hamate

What type of bone is the pisiform? What does this mean?
- Sesamoid
- This means it is a bone that develops inside a tendon after birth and exists to aid the action of muscles

What are the bones of the hand?

What are the joints between the phalanges known as? What are the ‘knuckle’ joints known as?
- Joints in between the phalanges are known as the distal/proximal interphalangeal joint
- The ‘knuckle’ joints are known as the metacarpophalangeal joints

What are the rotator cuff muscles? What are their attachments? What are their innervations? What are their actions?

What can a fracture to the humeral head damage? What is this commonly caused by? What can this lead to?

What are the muscles of the arm? What are their innervations? What are their actions?

What can a fracture of the humeral shaft damage?
Radial nerve

Is the biceps brachii the strongest supinator of the arm?
Only when the elbow is flexed at 90 degrees



What are the three ligaments of the hip joint?
- Ileofemoral ligament
- Pubofemoral ligament
- Ischiofemoral ligament

Diagram of the femur.

What is the socket called that the head of the femur sits in?
Acetabulum

What are the ligaments, bursae and menisci of the knee?

What are the actions of fibrularis longus and fibrularis brevis?

What is the action of the lateral leg muscles? What are they innervated by? Where do they receive their arterial supply from?







