advance histopath Flashcards
what is a teratoma
type of germ cell tumour
what types of tissue can teratomas contain
ectoderm
mesoderm
endoderm
where do teratomas form
Common in ovary and testes but can occur in other places
can occur from germ cells that were left behind during embryonic migration from the posterior dorsal ridge
ie in the middle of the body: pineal, base of the skull, mediastinum, retroperitoneum and sacro-coccygeal area

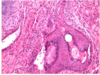
ectoderm teratoma
squamous epithelium
hair follicles

mesoderm teratoma
cartilage surrounded by metabolically active spindle cells

GI epithelium
endoderm teratoma
different types of ovarian tumour
from the surface epithelium ie mesothelial lining
Sex cord/stroma – graffian follicle and supporting cell (not ovum in centre)
Germ cell tumour
- including teratoma
- Yolk sac and chorio are from the trophoblasts
testicular germ cell tumours

classification of teratomas
- Divided into mature and immature
- Mature – mature tissue
- mature either solid or cystic (ie dermoid cyst)
- can become malignant – any type of tumour because any type of tissue can be present
- Immature – embryonic or fetal tissue – bad prognosis - because the tissue can proliferate because have the stem cells
- Also contain mixed elements
can be monodermal - ie one layer

epidemiology of teratomas
more common in ovary than testes
in ovary - more ‘‘benign’’ ie more mature = act benign
in testes more ‘‘malignant’’ - ie more immature = act malignant
Subtle difference in genetics that make this difference
Incidence is increasing

testicular teratoma
Variable looking because have a lot of different tissues

mixed germ cell tumour
70% teratoma 30% embryonal ca
Solid
Immature

- Teratoma
- Extra-dermal elements – skin, teeth, hair
- Mature cystic
- A lot of ovarian are cystic – more commonly known as dermoid cyst
grading of teratomas
look at how much immature neural tissue there is

immature nerual tumour
neuroectoderm
primitive – making spinal cord and brain
where are neuroendocrine tumours found
every tissue of the body
GIT - very common, SI and rectum most common
- Foregut, mid and hindgut
- foregut - thymus, oesophagus, lung stomach, duodenum, pancreas
- migut - appendix, ileum, cecum, ascending colon
- hindgut - distal bowel, rectum
- Hindgut tumours – low grade
- Mid gut – highgrade
lung and bronchus - common
L is GIT, R is pancreas
red granular cytoplasm cells

electron microscopy of normal neuroendocrine cells
See the granules

immunohistochemical markers for neuroendocrine tumours
chromogramin – core of the neurosecretory granules – marker for these tumours
synaptophysin - specific marker for neuroendocrine tumours
CD56 also mark NK cells
Also mark tumour for the hormone that it produces ie gastrin, serotonin, insulin

neuroendocrine tumour
grading of neuroendocrine tumour
Ki-67 is a marker for the cells that are actively proliferating – more = high grade. <3% low grade well differentiated neuroendocrine tumour
Number of mitoses

neuroendocrine tumour behaviour
Grade determines behaviour – high = more aggressive – chemo, may have met – need more aggressive therapy
Imaging – low grade – measure uptake of chemical processed by neuroendocrine cell – when v malig – less diff so just use PET
staging of neuroendocrine tumour
TNM system – staging system depends on the site of the tumour
syndromes associated with hypersecretion
zollinger-ellison = tumour of the pancreas or duodenum – gastrin = gastroin hypersecretion by parietal cell = acid = peptic ulcer of stomach, duodenum, jejunum
carcinoid = serotonin
hypoglycaemia = insulin


