Acute Lung Injury Flashcards
How does the status of cardiopulmonary function deteremine the damage that is done to lung tissue by embolization?
Adequate C/P function:
• Bronchial Artery Supply should be enough to keep tissue distal to the infarction alive.
Inadequate C/P function:
• Infarction
How do you know a clot is premortum?
Lines of Zahn - alternating lines of fibrin and blood clots

What is seen here?


What is seen here?


What happens to lung tissue around 48 hours after infarct?
Tissue becomes a paler red-brown from conversion of hemoglobin to hemosiderin by macrophages that eventually progresses to form a scar

What is seen here?

A non-thrombotic emboli that has resulted from cellulose buildup resulting in plug formation in this small artery
What is seen here?

Bone marrow embolus that may result from bone trauma.
• Note the fat and hypercellularity that are tale-tale signs that this is bone marrow.
What kind of embolus is seen in patients who die as a result of resuscitation?
Bone/Fat emboli from cracking ribs

What is shown here?
• what should you worry about?

Amniotic Fluid Embolus - often results in DIC and death. Note teh keratin debris that can be seen throughout the tissue.
What is seen here?


What are some hemodynamic vs. intrinsic reasons for edema in the lungs?
Hemodynamic:
Heart Failure - edema from increased HYDROSTATIC pressure
Liver Disease - edema from decreased ONCOTIC pressure
Intrinsic - Microvascular Injury:
• Infections
• Inhaled smoke and other gases
• Shock
What key features are highlighted by the arrows in this picture?
• what is it showing?

Right: Alveolar Macrophages
Middle: Exudate (protein stains pink)
Left: Engorged capillaries
This is the microscopic appearance of pulmonary edema.
What causes the formation of heart failure cells?
• In chronic pulmonary congestion as is seen in CHF, alveolar macrophages ingest blood from microhemorrhages that take place from high pressure. These hemosiderin laden macrophages are known as heart failure cells.

How does ARDS manifest histologically?
Histologically we see Diffuse Alveolar Damage (DAD)
What are the steps and key mediators in the formation of hyaline membranes in ARDS?
- endothelial activation and release of TNF
- TNF recruits neutrophis that secrete macrophage inhibitor factor (MIF) which amplifies inflammatory response
- Hyaline Membranes of protein form as a result of Hyaline Membrane damage
- TGF-ß and PDGF are key in the proceeding fibrotic process in which Edema and Hyaline membranes receed only to be replaced by collagen.

What is shown here? Is the process Acute or Chronic?
• how do you know?

Chronic Diffuse Alveolar Damage, we know its chronic because the trichrome stain stains collagen blue. TGF-ß and PDGF cause fibrosis and collagen deposition AFTER the acute phase of the disease is over.
This is from a patient who had ARDS. Was this biopsy taken soon after the attack or later?

This shows hyaline membrane formation so the biopsy was likely taken soon after disease.
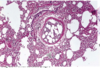
What is shown here?

Neonatal Respiratory Distress Syndrom.
Diffuse Alveolar Damage primarily affect which pulmonary function?
DAD typically affects DIFFUSION OF GASES
How is edematous fluid removed from the lungs?
Via lymphatics, lymphatics always drain the interstitium
Following pulmonary thromboembolism, what is the most important factor in the development of pumonary infarction?
Congestive Heart Failure
What is the most common cause of cor pulmonale?
Pulmonary Emboli


