Acute ischaemia: Mesenteric Flashcards
Define acute mesenteric ischaemia
Sudden inadequate blood flow through the mesenteric vessels ➔ ischaemia and gangrene of the bowel wall.
Which age group does acute mesenteric ischaemia tend to occur in?
Aged over 50
Categorise the four primary causes of acute mesenteric ischaemia
- Non-occlusive mesenteric ischaemia (NOMI) - 20%
- Acute mesenteric arterial embolism (AMAE) - 50%
- Acute mesenteric arterial thrombosis (AMAT) - 25%
- Mesenteric venous thrombosis (MVT) - <10%
Name two secondary causes of acute mesenteric ischaemia
- Mechanical obstruction
- Tumour compression
- Post-angiograph thrombosis
Give two causes of acute mesenteric arterial embolism
- Cardiac emboli: post-MI; AF; mitral stenosis; endocarditis
- Ruptured proximal atheromatous plaque
- Dislodged atheromatous plaque (iatrogenic)
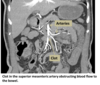
Which vessel is most commonly involved in acute mesenteric arterial embolism?
Superior mesenteric artery (SMA)
Name three causes of acute mesenteric arterial thrombosis
- Atherosclerosis
- Aortic aneurysm
- Aortic dissection
- Arteritis
- Decreased cardiac output
- Dehydration
How does acute mesenteric ischaemia differ between embolic and thrombotic causes?
Embolic events tend to occur in arterial branches ➔ limited ischaemia
Thrombosis typically occurs at the vessel origin ➔ extensive ischaemia
Name two causes of non-occlusive mesenteric ischaemia
- Hypotension (CHF, MI, sepsis etc.)
- Vasopressor drugs
- Ergotamines (migraine Tx)
- Cocaine
- Digitalis (foxglove)
Name two causes of mesenteric venous thrombosis
- Hypercoagulability
- Tumour: venous compression; hypercoagulability
- Infection
- Portal hypertension due to cirrhosis
- Venous trauma
Describe the presentation of acute mesenteric ischaemia
- Moderate-severe colicky or constant diffuse pain
- Disproportionate to physical examination findings
- Especially post-prandial
- NaV (75%)
- Anorexia - avoidance of postprandial pain
- Obstipation (complete severe constipation)
- Early: minimal or no tenderness, no signs of peritonitis
- Later: peritonism, may be a palpable mass
What additional clinical features develop as the bowel becomes gangrenous?
- Rectal bleeding
- Sepsis
Name three potential investigations for acute mesenteric ischaemia
- CT angiography
- FBC and ABG: sepsis; metabolic acidosis
- Clotting
- G+S
- AXR: exclude other causes
- Erect CXR: assess bowel perforation
- Multidetector CT: if SMA occlusion suspected
- ECG: AF or MI
- Echo: embolic source; valvular pathology

Name three differential diagnoses for acute mesenteric ischaemia
- Acute abdomen (cholecystitis, appendicitis, pancreatitis etc.)
- Abdominal aortic aneurysm
- Ectopic pregnancy
- MI
- Testicular torsion
- Sepsis: multiorgan failure
Outline the initial management of acute mesenteric ischaemia
- Fluid and oxygen resuscitation
- Senior support and early ITU input
- NG tube
- Broad spectrum IV antibiotics
- IV heparin
Outline the definitive management of acute mesenteric ischaemia
- Laparotomy if overt peritonitis
- Revascularisation if possible
- Otherwise, resect all non-viable regions
- Preserve all viable bowel
Describe the prognosis of acute mesenteric ischaemia
Give two complications
Poor prognosis
- Missed diagnosis: 90% mortality
- Treated: 50-80% mortality
- Extensive bowel surgery has potential of lifetime disability
Complications: bowel necrosis; perforation; short gut syndrome (malabsorption)


