Acute and Emergency Dermatology Flashcards
describe the properties of skin as an organ?
- The skin is the largest organ in the body
- 10% of body mass of average person
- Like any organ the skin can fail
A

sepsis
B

Hypo- and Hyper- thermia
C

Protein and fluid loss
Renal impairment
Peripheral vasodilation
what is Erythroderma?
Erythroderma is the term used to describe intense and usually widespread reddening of the skin due to inflammatory skin disease
A descriptive term rather than a diagnosis
“Any inflammatory skin disease affecting >90% of total skin surface”

what are the causes of erythroderma?
Psoriasis
Eczema
Drugs
Cutaneous Lymphoma
Hereditary disorders
Unknown
what are the principles of management for erythroderma?
Appropriate setting - ?ITU or burns unit
Remove any offending drugs
Careful fluid balance
Good nutrition
Temperature regulation
Emollients – 50:50 Liquid Paraffin : White Soft Paraffin
Oral and eye care
Anticipate and treat infection
Manage itch
Disease specific therapy; treat underlying cause
are drug reactions common or rare?
Common - 5% of inpatients
when do drug reacitons occur?
Can occur to any drug
Commonly 1-2 weeks after drug - Within 72 hours if re-challenged
what are examples of a mild and severe drug reactions?
- Mild - Morbilliform exanthem
- Severe - Erythroderma, Stevens Johnson Syndrome/Toxic epidermal necrolysis, DRESS
What is Stevens Johnson Syndrome/Toxic Epidermal Necrolysis?
- 2 conditions which are thought to form part of the same spectrum
- Rare:
- 1-2/million/year (SJS)
- 0.4-1.2/million/year (TEN)
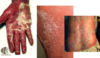
(pictures showing Stevens Johnson Syndrome (SJS) & Toxic Epidermal necrolysis (TEN))

Stevens Johnson Syndrome/Toxic Epidermal Necrolysis can occur secondary to what drugs?
Antibiotics
Anticonvulsants
Allopurinol
NSAIDs
Can be delayed onset
In Stevens Johnson Syndrome/Toxic Epidermal Necrolysis what percentage of skin is usually affected?

what are the clinical features of SJS?
- Fever, malaise, arthralgia (pain in a joint)
- Rash:
- Maculopapular, target lesions, blisters
- Erosions covering <10% of skin surface
• Mouth ulceration:
- Greyish white membrane
- Haemorrhagic crusting
• Ulceration of other mucous membranes
what are the clinical features of Toxic Epidermal Necrolysis?
- Often presents with prodromal febrile illness
- Ulceration of mucous membranes
- Rash:
- May start as macular, purpuric or blistering
- Rapidly becomes confluent
- Sloughing off of large areas of epidermis - ‘desquamation’ (skin peeling) > 30% BSA
- Nikolsky’s sign may be positive

what is the management of SJS and Toxic Epidermal Necrolysis?
- Identify and stop culprit drug as soon as possible
- Supportive therapy
Not common so no high quality trials to see what works:
- ?High dose steroids
- ?IV immunoglobulins
- ?Anti-TNF therapy
- ?Ciclosporin
what is the prognosis of SJS and TEN and how is it determined?
Mortality up to 10% (SJS)/30% (TEN)
SCORTEN:
- Age >40
- Malignancy
- Heart rate >120
- Initial epidermal detachment >10%
- Serum urea >10
- Serum glucose >14
- Serum bicarbonate <20

what are the long term complications of SJS and TEN?
Pigmentary skin changes
Scarring
Eye disease and blindness
Nail and hair loss
Joint contactures
what is Erythema Multiforme?
Hypersensitivity reaction usually triggered by infection - Most commonly HSV, then Mycoplasma pneumonia

SJS and TEN are drug related but this is viral related
how does Erythema Multiforme present?
• Abrupt onset of up to 100s of lesions over 24 hours:
- Distal to proximal
- Palms and soles
- Mucosal surfaces (EM major)
- Evolve over 72 hours
- Pink macules, become elevated and may blister in centre
- “Target” lesions
SJS lesions are atypical target lesion but in this there is typical target lesions

How do you treat Erythema Multiforme?
- Self limiting and resolves over 2 weeks
- Symptomatic and treat underlying cause
How common is Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), what is its prognosis and how long is its onset?
- Incidence estimated between 1 in 1000-10,000
- Mortality up to 10%
- Onset 2-8 weeks after drug exposure
DRESS can be up to 2 months later from drug where as TEN tends to be quite soon after
DRESS and TNE are the 2 most severe type of drug reactions you do not want to miss

what are the clinical features of DRESS?
- Fever and widespread rash
- Eosinophilia and deranged liver function
- Lymphadenopathy
- +/- other organ involvement
what is the treatment of DRESS?
- Stop causative drug
- Symptomatic and supportive
- Systemic steroids
- +/- Immunosuppression or immunoglobulins