Acid-Base Physiology Flashcards
Hyperventilation
increased breathing beyond what is required, given the metabolic production of carbon dioxide, to maintain a normal PaCO2
Normal range of PaCO2
36-44 mm Hg
Hypoventilation
Decreased breathing below that which is required for a given level of carbon dioxide production to maintain a normal PaCO2
Hyperpnea
Increased ventilation with a normal PaCO2 (for example, during mild to moderate exercise), i.e., the increase in ventilation is commensurate with the increase in carbon dioxide production.
Tachypnea
Rapid breathing, i.e., a respiratory rate that is above normal. Although total ventilation tends to be elevated in patients who are tachypneic, alveolar ventilation may be normal or greater/lower than normal depending on the tidal volume and the amount of dead space being ventilated
Carbon dioxide elimination is dependent upon ___ ventilation
Carbon dioxide elimination is dependent upon alveolar ventilation
Not necessarily total or minute ventilation
Total ventilation [VE]
VE = VA + VD
a = alveolar
d = dead space
Tractus solitarius
Group of neurons in the medulla whose firing increases with inspiration.
Nucleus retroambigualis
Group of neurons in the medulla whose firing increases with expiration.
Two ‘phases’ of exhalation
- expiratory neurons fire to “brake” the inpiration
- inspiratory activity is completely absent
Electrical activity in inspiratory motor neurons during unstressed breath cycle

Hering-Breuer Reflex
An inspiratory-inhibitory reflex stimulated by pulmonary stretch receptors in the lung during inspiration. Activity is maintained with a sustained stretch
aka slowly adapting stretch receptors
Irritant receptors
Stimulated by mechanical or chemical irritation in the airways. These receptors may be partly responsible for the hyperventilation seen with acute asthma
aka rapidly adapting stretch receptors
Pulmonary vascular receptors
These receptors are part of a group of non-myelinated fibers called C-fibers
Stimulation of receptors in pulmonary capillaries or the interstitium of the lung (juxtapulmonary-capillary or “J” receptors) lead to increased ventilation. These receptors may be responsible for the hyperpnea associated with pulmonary embolism and congestive heart failure as well as interstitial lung disease
Chest wall receptors
Muscle spindles as well as receptors in joints and tendons may help adjust ventilation under conditions of mechanical loading, e.g., patients with airway obstruction. They may also play a role in the hyperpnea of exercise.
Peripheral chemoreceptors
located in the aortic arch and at the bifurcation of the internal and external carotid arteries (receptors in the aortic arch have relatively minor, if any, role in control of breathing in humans); provide input about the PaO2, PaCO2, and pH.
Central chemoreceptors
Located below the ventral surface of the medulla; detect changes in the PCO2/pH of brainstem interstitial fluid
Ventilatory responses to hypoxemia and hypercapnia are measured in ___ experiments.
Ventilatory responses to hypoxemia and hypercapnia are measured in rebreathing experiments.
Hypoxic Ventilatory Response
Hypoxemia results in minimal stimulation of ventilation until the PaO2 decreased to less than 60 mmHg. Stimulation comes from peripheral chemoreceptors, which appear to respond to PaO2 rather than the overall content of arterial blood.
Ventilatory response to hypoxemia
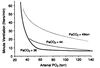
Hypercapnic Ventilatory Response
There is a linear relationship between alveolar ventilation and PaCO2 levels, over a physiologic range.
An increase in PaCO2 results in a much more pronounced increase in ventilation as compared to hypoxemia. Hypercapnia stimulates both peripheral and central chemoreceptors, resulting in an increased drive to breathe.
Hydrogen Ion chemoreceptors
Hydrogen ions cross the blood brain barrier too slowly to have an impact initially on the central chemoreceptors. They do stimulate the peripheral chemoreceptors resulting in an increase in ventilation.
Carbon dioxide diffuses out of CSF as the PaCO2 drops in the systemic circulation with increased ventilation. This lowers CSF carbon dioxide and reduces stimulation of central chemoreceptors. Over time (days), the CSF bicarbonate concentration normalizes.
3 Phases of Ventillation Increase during Exercise
- Neurological Phase - immediate phase
- Metabolic Phase - slowly increasing ventilation during mid-phase of exercise; associated with increasing oxygen consumption
- Compensatory Phase - more pronounced increase in ventilation after anaerobic threshold has been exceeded and metabolic acidosis ensues (the increase in ventilation helps to mitigate the acidosis); more intense exercise.
Neurological Phase of exercise response
Occurs almost instantaneously, far too quickly to be explained by changes in metabolism or blood gases. Felt to be due to “neural mechanisms”- possibly connections from motor cortex to respiratory centers, from skeletal muscle to respiratory centers - or a conditioned reflex or learned response.
Metabolic Phase of exercise response
With exercise up to approximately 40-60% of maximal exercise capacity, ventilation increases linearly with oxygen consumption and carbon dioxide production, although the mechanism by which this occurs is not clear.
There is no known receptor that monitors oxygen consumption or carbon dioxide production directly, and PaO2 and PaCO2 remain in the normal range, which eliminates stimulation of the chemoreceptors as the likely explanation.
Compensatory Phase of exercise response
Above 40-60% of maximal exercise capacity, anaerobic metabolism occurs with resulting accumulation of lactic acid (anaerobic threshold).
This results in further increases in ventilation out of proportion to oxygen consumption. The ventilatory system now must also operate to compensate for the developing metabolic acidosis.
Classic mistake in chronic hypercapnia
These patients are dependent on their “hypoxic drive to breathe” (because they are chronically hypercapnic, the CSF has adapted and has a relatively normal pH; thus, the chronic hypercapnia is not causing ongoing stimulation of the ventilatory centers) and, if they are given supplemental oxygen, they will “stop breathing.”
The above is false. What is really observed: The drive to breathe in these patients is very high (probably as a result of stimulation of irritant receptors in the lung as well as acute hypoxemia and hypercapnia, and behavioral factors, e.g., shortness of breath). While the drive to breathe is reduced slightly by the administration of oxygen, the subsequent rise in PaCO2 is due only in part to the suppression of hypoxic drive. Haldane effect and ventilation/perfusion matching also occur.
Haldane effect
Shift in the carbon dioxide-hemoglobin curve to the right with addition of oxygen; i.e., for the same carbon dioxide content, the PaCO2 is higher because oxygen displaces CO2 from the hemoglobin
Changes in ventilation/perfusion matching in hypercapnic patients or COPD patients
reversal of hypoxic pulmonary vasoconstriction in poorly ventilated regions of lung
volatile vs fixed acids
Volatile acids may be released from the body via respiration
Fixed acids have too low of a vapor pressure for this, and so must be eliminated via the kidneys
Fixed acids in humans
- Phosphates
- Sulfates
___ do the lion’s share of the work when it comes to eliminating acid from the body
The lungs do the lion’s share of the work when it comes to eliminating acid from the body
10,000 - 15,000 mEq carbonic acid eliminated by the lungs per day
50-100 mEq of sulfiric and phosphoric acid eliminated by the kidneys each day
pH of arterial blood
7.40 (range 7.36-7.44)
The body’s initial response to an acute change in pH
Buffers!
The body’s long-term response to a chronic change in pH
compensatory processes
Hyperventilation and hypoventilation effects on blood pH
Hyperventilation eliminates more CO2 in the blood, shifting the bicarbonate equilibrium and increasing pH (alkalosis)
Hypoventilation builds up carbonic acid in the blood, shifting the bicarbonate equilibrium and reducing pH (acidosis).
Protein buffers
Hemoglobin: acts as a major buffer in the blood for respiratory acid (carbonic acid). CO2 diffuses into the red blood cell where, in the presence of carbonic anhydrase, it forms carbonic acid, which dissociates to H+ and HCO3 - . The proton binds to the negatively charged hemoglobin molecule, and the bicarbonate is moved outside the cell.
Thus, the initial buffering of acid resulting from the accumulation of carbon dioxide is done by proteins and leads to a rise in the serum bicarbonate
Henderson-Hasselbalch

Respiratory Acidosis
Decreases in alveolar ventilation result in increase in alveolar and arterial PCO2, which reacts with water to form carbonic acid and reduce blood pH.
The exact arterial pH depends on the buffers in the blood and the ability of the kidneys to compensate over 48-72 hours from the onset of the primary disturbance
Respiratory Alkalosis
Alveolar ventilation in excess of what is needed to eliminate body’s production of CO2 → leads to a decrease in PaCO2 and a rise in pH
Metabolic Acidosis
Caused by ingestion, infusion, or production of fixed acids, reduced filtration of metabolic acids by the kidney, decreased renal secretion of hydrogen ion, movement of hydrogen ion from the intracellular to the extracellular fluid, or loss of bicarbonate
Metabolic Alkalosis
Caused by excessive loss of fixed acids from the body or ingestion, infusion, or excessive renal absorption of bases such as bicarbonate
Table of the primary acid/base disorders

Respiratory Compensation
The body has the ability to quickly adjust ventilation to compensate for changes in hydrogen ion concentration
Metabolic Compensation
Kidneys instrumental in this process. If respiratory acidosis, the kidneys can excrete excess acid (which secondarily results in increased serum bicarbonate)
Remember, bicarbonate is . . .
Remember, bicarbonate is not an effective buffer for respiratory acidosis
In many cases of acidosis/alkalosis, except in some cases of repsiratory alkalosis, the body . . .
In many cases of acidosis/alkalosis, except in some cases of repsiratory alkalosis, the body does not fully compensate back to a normal pH for any acute acid-base disturbance.
Table of compensatory mechanisms for various primary pH disturbances

Because of the delay in the response of the renal system to primary acid-base abnormalities of the respiratory system, one can categorize respiratory system acid-base disorders as . . .
Because of the delay in the response of the renal system to primary acid-base abnormalities of the respiratory system, one can categorize respiratory system acid-base disorders as acute or chronic.
In an acute respiratory system disturbance, the pH changes by 0.08 units for every change of 10 mm Hg in the PaCO2; for a chronic respiratory disorder, the pH changes by 0.03 units for every 10 mm Hg change in the PaCO2.
When analyzing an acid-base problem, you should ask yourself. . .
- Is the pH abnormal? In what direction?
- Is the change in PaCO2 in the direction expected for a primary respiratory disturbance?
- If a primary respiratory disturbance is present, is it acute (0.08 pH units / 10 mm Hg PaCO2) or chronic (0.03 pH units / 10 mm Hg PaCO2)?
- If a primary metabolic disturbance is present, is there an appropriate respiratory system response?
Stimulation of flow receptors in the airways has ___ effect on ventilation
Stimulation of flow receptors in the airways has an inhibitory effect on ventilation
Inflation of the lung has ___ on the controller. Deflation of the lung has ___ on the controller.
Inflation of the lung, which stimulates slowly adapting stretch receptors, has an inhibitory effect on the controller. Deflation of the lung has a stimulatory effect on the controller.
The peripheral chemoreceptors . . .
The peripheral chemoreceptors are located in the carotid bodies and are stimulated by low PaO2, high PaCO2, and low arterial pH.
The central chemoreceptor . . .
The central chemoreceptor is located in the medulla and is activated by high PaCO2 and low arterial pH.
___ results in a counterbalancing role for the central chemoreceptor relative to the peripheral chemoreceptor when the latter is responding to acute changes in arterial pH.
The differential permeability of the blood-brain barrier for carbon dioxide and hydrogen ions results in a counterbalancing role for the central chemoreceptor relative to the peripheral chemoreceptor when the latter is responding to acute changes in arterial pH.
Patients with chronic hypercapnia are ___ in order to breathe any more than healthy individuals
Patients with chronic hypercapnia are NOT dependent upon hypoxemia in order to breathe any more than healthy individuals
A respiratory acidosis is characterized by. . .
. . . an increased PaCO2, a decreased pH, and ultimately an increase in the serum bicarbonate concentration as protons are secreted in the renal tubule
A respiratory alkalosis is characterized by. . .
. . . a decreased PaCO2, an increased pH, and a mild decrease in the serum bicarbonate concentration.
A metabolic acidosis is characterized by . . .
. . . a reduced bicarbonate concentration and a low pH
A metabolic alkalosis is characterized by. . .
. . . an increased bicarbonate concentration and an elevated pH
If there is evidence of an abnormal pH but the PaCO2 has moved in a direction that is opposite of what you expect for a primary respiratory disorder, . . .
. . . you are dealing with a primary metabolic disturbance with respiratory compensation.
Because the lung relies on stored potential energy to exhale when at rest, if the compliance of the lung is high, then . . .
. . . it will not have enough elastic recoil and stored potential energy to push the air out again without exerting energy from the exhalatory muscles.
This is the case in emphysema
Respiratory acidosis caused by high alveolar compliance diagram

Total blood CO2
PCO2 + CO2 bound to hemoglobin
Remember that PCO2 does not capture this bound CO2!
Even though ventilation-perfusion mismatch is very common (many COPD patients, etc), . . .
. . . hypercapnia secondary to ventilation-perfusion mismatch is relatively rare.
That is because the body can usually adapt by increasing ventilation rate and effectively eliminating more CO2 per minute from its still functioning alveoli.
Symptoms of respiratory alkalosis
painful tingling in the hands and feet, numbness and sweating of the hands, and cerebral symptoms following voluntary hyperventilation.
Normal PaO2
80-100 mmHg
You are evaluating a 75-year-old woman with chronic obstructive pulmonary disease (COPD) for a chief complain of months of shortness of breath. She describes her shortness of breath as being constantly present, but worse with exertion. As part of her evaluation, an arterial blood gas (ABG) on room air is performed, demonstrating a pH of 7.31, PaCO2 of 68mm Hg, and a PaO2 of 65mm Hg. Which of the following is most accurate interpretation of her ABG?
Chronic respiratory acidosis
A patient with diffuse lung disease has led to severe ventilation/perfusion mismatch. She has chronically elevated PaCO2. Suffering from an acute bronchitis, her PaO2 falls to 50 mm Hg. She is being evaluated in the Emergency Department and is given supplemental oxygen (100%) to breathe via a mask. You predict:
the PaCO2 will rise, but she will not stop or severely decrease her breathing.
Administration of supplemental oxygen to a patient with severe V/Q mismatch may lead to . . .
a rise in the PaCO2 due to worsening of the V/Q mismatch (more blood being sent to poorly ventilated units due to reversal of hypoxic pulmonary vasoconstriction as alveolar O2 rises with the supplemental oxygen), the Haldane effect, and a small drop in ventilation mediated by the chemoreceptors as arterial O2 rises. The patient will not stop breathing completely, however, because we do not breathe from minute to minute due to hypoxemia.
An ‘acute exacerbation’ of COPD results in . . .
acute increase in dead space
Hyperventilation vs Hyperpnea
Hyperventilation refers specifically to abnormal PaCO2, so you can have adaptive or pathological hyperventilation.
Hyperpnea refers specifically to increased breathing rate with normal PaCO2, so you basically only ever ahve adaptive hyperpnea.
Physiologic range of bicarbonate
~24 mEq / u


