A/53-71 NEOPLASIA Flashcards
What are the 3 leading causes of mortality in adults and in children?
Adults:
- Cardiovascular diseases
- Cancer
- Cerebrovascular diseases
Children:
- Accidents
- Cancer
- Congenital defects
What is Neoplasia?
an abnormal mass of tissue, the growth of which exceeds and is uncoordinated with that of the normal tissue and persists in the same excessive manner after the cessation of the stimuli which evokes the change.
What are the componants of a tumor?
- parenchyma: made up of transformed or neoplastic cells. determines the biologic behavior
- stroma: the supporting, host-derived non neoplastic stroma: connective tissue, blood vessels and inflammatory cells. crucial for growth → support the neoplastic cells
What are the features of the neoplastic cells? (8+2)
The 8 + 2 features of neoplastic cells:
- autocrine pattern of growing: cell produce the ligand and the receptor for its own growing.
- resistance to apoptosis. The growth and size of the neoplasm is due to rate of proliferation and rate of apoptosis and necrosis.
- unlimited capacity to mitosis
- loss of differentiation
- capacity for angiogenesis by secretion of cytokines and humeral factors
- invasion of surrounding tissue: the property by which malignant tumor can grow into and at the expense of the surrounding tissue
- capacity for making distant metastasis
- Reprograming of cell metabolism
- independence of growth restricting signals
- evade from the immune system
Nomenclature:
- Neoplasm
An abnormal mass of tissue. An overgrowth of a tissue which persists even after the cessation of the stimuli that evoked the change.
Nomenclature:
- tumor
Means swealing as in inflammation but it used as Neoplasm in a common medical usage.
Nomenclature:
- Cancer
a malignant tumor/neoplasm
Nomenclature:
- Benign
A neoplasm which grows in an expansile manner only (not infiltrative) → pushes aside the normal tissue.
Do not metastasizes.
Easily removed surgically.
No recurrency.
–oma
Benign epithelial neoplasms: adenoma (applied to those exhibiting glandular pattern or those derived from glands w/o exhibiting glandular pattern)
papillaryadenoma, cystadenoma
Benign mesenchymal neoplasms: hemangioma, chondroma, osteoma
Mixed cell: epithelial components dispersed in a fibromyxoid strome. Example: pleomorphic adenoma (in the salivary glands), fibroadenoma (female breast)
Germ cells: teratoma. Tumors derived from germ cells and most commonly arise in the testis or ovary. The tumor contains neoplastic tissues derived from all of the three germ cell layers and thus contains diverse types of tissue. Can be also malignant.
Nomenclature:
- malignant
can invade the surrounding tissue.
Metastasizes.
High chance for recurrence.
Epitheial: carcinoma
adenocarcinomas, squamous cell carcinomas, renal cell carcinoma
mesenchymal: sarcoma
osteosarcoma, angiosarcoma, chondrosarcoma
Germ cells: malignant teratoma
Nomenclature:
- Polyp
A mass that projects above the a mucosal surface.
- Can be benign or malignant.
Nomenclature:
- semi-malignant
neoplasms which show some features of malignancy: they locally in an invasive pattern, frequently reoccur but they rarely give metastasis.
There are 2 neoplasms which have this feature:
- pleomorphic adenoma (of the salivary gland):
- basal cell carcinoma
Nomenclature:
- border line
Features are transient between benign and malignant.
Its behavior cannot be predicted by their morphological presentation.
Mostly they don’t metastases but in some cases they do (but one cannot predict which one is which). Shouldn’t reoccur.
The most typical ones are the cystic borderline tumors of the ovary:
- ovarian cystadenoma (benign) ->
- cystadenocarcinoma (malignant)
What are the exceptions of the nomenclature (don’t follow the “rules”):
(3)
-
malignant lymphoma: it is a neoplasm of inflammatory cell which comes only in a malignant form! We can say only lymphoma. Further divided:
- Hodgking’s lymphoma
- Non-Hodgkin’s lymphoma
- melanoma malignum: no benign melanoma. The benign counterpart is nevus
- brain: the anatomical localization is more relevant then the histological appearance.
Astrocytoma: tumor of glial cell (glioblastoma is the high grade form).
What are the features of neoplasm that are assessed histologicaly?
- Type of tumor (bassed on origin)
- Dgree of differentiation
- Evidance of local invasion
- Presence of metastasis
- Presence or absence of other prognostic factors (e.g. estrogen receptors in breast carcinoma cells)
What is anaplesia and what are the features of anaplastic cells?
Lack of differentiation or loss of differentiation
- Pleomorphism
- Block of maturation
- Abnormal nuclei
- Mitosis
- Loss of polarity
- Metaplasia
What is the rate of growoth of:
- Benign
- Malignant
- Semi-malignant
- Border line
Benign: Generally low
Malignant: Generally high
Semi-malignant: Low
Border line: Low
What determines the rate of tumor growth?
Rate of proliferation <-> rate of necrosis/apoptosis
Give an example of a benign tumor which grows fast.
Leiomyoma - influenced by the circulating levels of estrogens..
**56-57**
What are the tumor suppressor genes?
encode proteins that inhibit cellular proliferation by regulating the cell cycle.
Unlike oncogenes, both copies of the gene must be lost for tumor development → tumor developes when the cell becomes homozygous for the mutant allele or, in other words, loses heterozygosity of the normal RB gene (one is absent, the remaining one is mutated → two-hit theory=Knudston theory)
What are the mechanisms of tumor suppressor gene inactivation?
- deletion
- make stop codon or missense mutation
- epigenetics
- transdominant gene: 1 is mutated and the other is not mutated. The two make a complex which inactivates the non-mutated
- haploinsufficiency: the amount of proteins generated by one gene is just not enough
Based on the tumor suppressor genes there are 2 alternative pathways that generate cancer
- hereditary cancer: children inherit one defective copy of the gene in the germ line, the other copy is normal. A disease develops when the normal copy is mutated due to somatic mutation (described above)
- sporadic cancer: the child inherits 2 normal alleles → 2 somatic mutations are needed for the disease to develop.
Explain what is retinoblastoma gene
- Role
- normal function
- What happens when mutated
Exist in 2 forms:
- Active - hypophosphorylated
- Inactive - hyperphosphorylated
Role: regulates the checkpoint: G1 → S transition.
Background: the initiation of DNA replication requires the activity of cyclin E-CDK2 complex.
- At the beginning of G1, RB is hypophosphorylated and active, and in this form it is bounded to E2F → E2F is inhibited → no transcription of cyclin E.
- Growth factor → cyclin D → cyclinD-CDK4/6 → phosphorylation of RB → release of E2F → cyclin E → progression through the cell cycle.
- During M phase the RB is dephosphorylated by phosphatase and becomes inactive again.
When RB is mutated: E2F is constantly active → cyclin E → transcription of cell cycle is running constantly
Also, mutations in the genes that control RB (CDK4, CyclinD) leads to the same disease.
What is P53 and its relation to cancer?
Important in controlling that everything is fine with the cell or there is a mutagenic effect.
If it detects any abnormality, it sentence the cell to:
- temporary cell cycle arrest (quiescence) → try to repair
- permanent cell cycle arrest (senescence)
- apoptosis
In non-stressed cells: P53 makes a dimer with MDM2 → P53 is destructed
Stressed cells: P53 undergoes post-transcriptional modification → released from MDM2 →
Genes activated by P53:
- P21 (a CDK inhibitor) → inhibits CDK-cyclin complex → no phosphorylation of RB → E2F remains inactive → cell cycle arrest
- GADD45: DNA repair
- Bax/PUMA: push the cell to apoptosis
If P53 is mutated nothing will direct the cell to correction stoppage or apoptosis
The cell can acquire additional mutation
More than 70% of human cancers have defect in this gene.
What is APC gene and its relation to cancer?
Loss of APC (tumor suppressor gene) leads to an hereditary disease called adenomatosis polyposis coli.
This gene exerts an antiproliferative effect by regulating the intracellular levels of β-catenin.
In case of APC mutation: β-catenin remains in the cell → continous cell proliferation
WNT pathway: can active or inactive
- Active: WNT binds to the receptor → signal: no degradation of b-catenin → b-catenin translocates to the nucleus → binding to TCF transcription factor → cell proliferation
- Inactive (in quiescent cells): no WNT → active destruction complex, which includes APC → b catenin is degraded → no proliferation!
List the 3 types of DNA repair proteins that their mutation increase the risk for developing cancer
- Mismatch repair
- Nucleotide excision repair
- Homologue recombination repair
Describe the mismatch repair
The repair system: MSH2+MSH6= MUTSα complex. MSH2+MSH3=MUTSβ complex.
Mutation in any of the gene coding for this proteins → no repair → mutations accumulate in the cell.
Hereditary nonpolyposis colon cancer syndrome: familial carcinomas of the colon is the result of such a mutation.
Describe the nucleotide excision repair
- What will a defect in this repair will lead to?
related to UV exposure which leads to the formation of thymidine dimers.
The system corrects the DNA by removing the dimers and synthesizing a new part of the strand.
A defect in this system leads to Xeroderma Pigmentosum, in which the patients developes skin cancer due to UV exposure.
Homologue recombination repair
- Pathway of repair
- Gene defect inheritance pattern
- Defect in which gene will give rise to which cancer?
several genes are responsible for correcting DNA damage which is caused by ionizing radiation and other agents.
ATM recognizes the mutation → phosphorylates BRCA1 → BRCA1 makes a complex with BRCA2 and RAD51 → corrects the mutation
Mutations in each of this genes impairs the system and give rise to cancers:
- Autosomal dominant:
- BRCA1 → breast, ovarian, prostate cancers
- BRCA2 → breast, ovarian, stomach, pancreas
- Autosomal recessive:
- ATM → ataxia teleangiectasia. Breast carcinoma, sporadic neoplasms
What are Telomeres
Telomeres are repeating sequences in the DNA at the end of the chromosome which protect the genetic material.
Every cycle the telomeres are being lost → cells have a limited capacity to divide!
Telomeres are lost → recognized as a break by the DNA repair system → tumor suppressor genes (RB, P53) mediate cell cycle arrest and apoptosis.
Telomerase in case of RB, P53 mutation
The DNA repair system is inappropriately activated → fuses the chromosomes to create a dicentric chromosomes.
Mitosis → chromosomes are pulled apaprt → breaks! → activation of the repair system → fusion to a dicentric chromosome.
The cell undergoes through bridge-fusion-breakage cycle which produces mitotic catastrophe and massive cell death.
However! If during this cycle a cell manages to reactivate the telomerase, the cycle ceases and the cell is able to avoid death. Up to this point, the cell had already accumulated many mutations → malignancy
In which cells telomerase is active?
Telomerase is active in normal stem cells and is absent or very low in most somatic cells
It is active in all types of cancers
What is Epigenetics?
Epigenetics is a term which refers to heritable and reversible changes in gene expression that occur without a mutation. (Do not involve changes in the DNA sequence)
Describe DNA methylation and its role in carcinogenesis.
Effects promoter regions.
Enzyme methyltransferase → hypermethylation → gene silencing.
In organogenesis, it plays a role in the switch-on switch-off modes.
Hypermethylation of tumor suppressor gene and their subsequent silencing plays a role in cancer, for example:
- ARF In colon and stomach cancer
- MLH1 mismatch repair gene in colorectal cancer
Describe the MicroRNAs and thier role in carcinogenesis
Are non-coding single stranded RNAs that function as negative regulators genes (inhibit gene expression).
Process:
- Pre-miRNA is transcribed and exported out of the nucleus.
- In the cytoplasm it is cut by Dicer after which it is considered mature → miRNA, double stranded.
- Next it is unwinded, and each single stranded is incorporated into a multiprotein complex called RISC complex.
- Base pairing between miRNA and mRNA directs the RISC complex to either cleave the mRNA or repress its translation.
MicroRNAs plays a role in carcinogenesis by the following manner:
- if in normal cases they can repress the expression of oncogenes, their reduced activity give rise to excess oncogene proteins.
- On the other hand, over-activity of them might repress tumor suppressor genes.
This has known to be involved in certain leukemias and lymphomas, where downregulation of miRNA result in the increased expression of BCL2, an antiapoptotic protein.
What is ‘Heritable cancer syndromes’?
List the types of heredity.
Genetic predisposing to cancer: the genetic and the environmental both cause cancer, the 2nd more important. the frequency of tumor which are purely related to genetics is 0.1%. The sporadic cancers use the same pathways as the genetic ones.
- Autosomal dominant cancers (inactivation of suppressor genes)
- Autosomal recessive cancers (defect in the repair mechanism)
- Familial cancers (specific gene with a defined inheritance pattern)
What is ‘Autosomal dominant cancers’, and which genes fall into this category?
fall in the category of inactivation of tumor suppressor genes.
The mutation gives rise to uncontrolled cell proliferation and growth.
- they need a double hit. In hereditary cancer syndrome one allele is silenced-inactivated, mostly due to point mutations. the 2nd will be inactivated during life, which is when the cancer develops. The genes that are falling into this category:
- RB gene
- APC gene
- P53 gene
- Hereditary non-polyposis colon cancer syndrome
What is ‘Autosomal recessive cancers’, and what falls into this category?
lower penetrance than the dominant ones.
Related to defect in the repair mechanism. This are the:
- Xerodema pigmentosa
- Ataxia genectasia
What is the meaning of ‘Familial cancers’?
virtually all the common types of cancers that occur sporadically have been reported to occur in familial forms.
Examles: carcinomas of the colon, breast, ovary and brain.
The transmission pattern is not clear.
Siblings have a relative risk between 2-3.
Predisposition to the tumor is dominant, but multifactorial inheritance cannot be ruled out.
What are the 2 categories of oncogene viruses?
- Oncogenic RNA viruses
- Oncogenic DNA viruses
Give an example of an oncogenic RNA viruse and explain it.
HTLV1: human T cell leukemia virus
A retrovirus (single stranded RNA which is transcribed to DNA) induces T cell leukemia/lymphoma by the following pathway:
- With its TAX gene, it initially causes polyclonal proliferation of T cells by autocrine and paracrine pathways. Also, TAX affects P53 and other tumor suppressor genes.
- Due to this, the proliferating T cells are at increased risk for secondary mutations, and the result is an outgrowth of a monocolnal neoplastic T cell population.
What are some examples of Oncogenic DNA viruses and what are the modalities for how they can cause cancer?
HPV, EBV, KSHC (Kaposi sarcoma herpesvirus), HBV
There are certain modalities for how the virus can cause cancer:
- Integrating and implanting an oncogene into the host’s DNA
- Integrating into the host’s DNA and up-regulating or down-regulating its genes.
- non-integration of the virus: epizonal: They may have oncogenes that directly act as such or they have regulatory genes, all are working without integrating.
- The presence of the virus leads to its elimination by immune system.
- → increased regeneration of the cells may activated certain genes to cause cancer.
- → inflammatory cells may release ROS, which are genotoxic → mutations in the genes of the cell.
EBV
- Which 3 diseases can it cause? (names only)
Can causes 3 different disease:
- Burkitt’s lymphoma
- a subset of Hodgkin’s lymphoma
- nasopharyngeal carcinoma
What is the pathomechanism of Burkitt’s lymphoma
Burkitt’s lymphoma: EBV integrates into the host’s DNA and exerts several effects:
- by its LMP-1 gene that acts as an oncogene: activates signaling pathways of NFƙB and JAK/STAT → B cell proliferation.
- activates BCL-2 → suspends apoptosis. The clone of infected B cells is proliferating.
- It contains also the EBNA-2 gene that activates host’s genes such as cycling D and the src family
- has viral cytokine that suppresses macrophages and monocytes activation.
- HOWEVER! The aforementioned affects are not enough for developing the disease. Lymphoma cells emerge only when additional mutations, such as the t(8;14) translocation that leads to c-myc regulation, occurs. So it is a multistep pathogenesis when beside the infection of the virus other mutations are needed to develop a cancer. The EBV is the 1st step
HPV: Human Papilloma virus
- what are the 2 options of neoplastic development of HPV?
- What are the 3 genes that are suspected to have oncogenic effect?
There are 2 options:
- To cause a benign squamous papilloma By HPVs 1,2,4,7. Remain epizonal
- Cervix carcinoma, laryngeal carcinoma By HPVs: 16,18,31,33. Integrating.
There are 2 genes which are suspected to have oncogenic effect:
- E7: suspends the action of RB. It makes a complex with it → E2F is released → increased cell proliferation. It also inactivates CDK inhibitors → help the cell proliferation.
- E6: deregulate P53 and Bax (pro-apoptotic) and activates telomerase → suspend apoptosis
*As In the previous case, infection with HPV is not sufficient to develop the disease. Another mutation should be present, for example: mutated RAS gene
How do HBV, HCV exert their oncogenic effect?
- 70-85% of hepatocellular carcinomas are due to such infections.
- the oncogenic effects of the viruses are multifactorial, but the dominant effect seems to be immunologically mediated chronic inflammation, hepatocellular injury, stimulation of hepatocyte proliferation and production of ROS that damage the DNA.
- the viruses contain proteins (HBX of HBV and core protein of HCV) that activate a variety of signal transduction pathways which also contribute to carcinogenesis.
Microbial carcinogenesis
- Describe the 1 example given in the lecture
Infection of Helicobacter Pylori is related to gastric adenocarcinomas and gastric lymphomas.
Infection by HP → chronic inflammation/gastritis → gastric atrophy → intestinal metaplasia → dysplasia → cancer
Occurs only in 3% of the infections.
HP is noninvasive, but it contains genes (CagA) that stimulate growth factor pathways.
The chronic atrophic gastritis activates B cell and T cell (which inturn activate B cell) → high proliferation of B cells which also accumulates mutations → MALT lymphoma
Which test can be preformed in order to test whether chemical is carcinogenic or not?
Salmonella → culture → put an agent → see the number of mutations caused in the bacteria by the chemical. Test for mutagenesis of chemicals.
What are the 2 groups of chemical carcinogenes
- directly acting agents: they do not require metabolic conversion to become carcinogenic. They are weak carcinogens that are used as chemotherapeutic drugs. For example: alkylating agents. They might cause cancer.
-
indirect acting agents: require metabolic conversion to become carcinogenic. This is done by the enzyme cytochrome P450 monooxygenase. Examples:
- Polycyclic hydrocarbons, as benzopyrene is transformed into epoxide during the high temperature combustion of tobacco in cigarette smoking → lung cancer. it may also be produced during the smoking process of meat and fish.
- aromatic amines, amides, azo dyes: 2-naphthylamine
- others: nitrites, aflatoxin B1 (produced by a mold)
What is the mechanism of action of chemical carcinogenes?
The carcinogenesis is a multistep event:
- initiation: made by certain chemicals which are genotoxic. Cause the mutational activation of an oncogene
- promotion: another factor stimulate the initiated (mutated) clone for overgrowing. Forced to proliferate, the initiated clone of cells accumulates additional mutations, eventually developing into a malignant tumor. Such chemicals are probably hormone-like substances.
What are the 2 types of radiations in radiations carcinogenesis?
Ionizing: X-ray, gamma ray, corpuscular etc. makes point mutation or double breaks. It is very Important that the homologue recombination system or mismatch repair will work.
Non ionizing: UV-B. Makes the thymidine dimer for which we need the nucleotide excision repair system. Non-melanoma skin cancers are associated with total cumulative exposure to UV radiation, whereas melanoma is associated with intense intermittent exposure, as occurs in sun-bathing.
What are the evidences immune system in cancer protection and development?
- we can see a lymphocytic infiltration around the tumor → mostly T cells
- the degree of infiltration of lymphocytes is related to the degree of progression of the disease. Highly infiltrative tumors → low progression
- Low infiltrative → high progression
- those patients who are immunosuppressed have higher chance for developing cancer, usually in the colon, skin.
- there are cancer-specific genetic alterations. If we test a healthy population for this genes we will definitely find mutations but no evidence for cancers in that patient → transiently we have cancer cells but they are not developing because the immune system eliminates them.
What are the 2 groups of tumor antigens?
Tumor specific antigen (TSA):
- generated and expressed only by tumor cells!
- Arise from products of: β-catenin, RAS, P53, CDK4 genes.
- They are highly immunogenic! No tolerance
Tumor associated antigens:
- Expressed differently on tumor cells
- Low antigenicity (present in normal as well)
- Have certiantolerance
- they become tumor associated in several ways
How do antigens become tumor associated?
- overexpression: example: tyrosinase, an enzyme involved in melanin biosynthesis. They are low immunogenic but are good for diagnostic purposes; Prostate specific Ag (PSA)
- onco-fetal antigens (embryonic antigens): α-fetoprotein for example. In certain neoplasms, such as colon and liver, this proteins are upregulated. Can serve as serum markers for cancers.
- oncospermatogonal antigens: are encoded by genes that are silenced in all adult tissues except the testis → the protein is present in the testis. As sperms don’t have MHC1 antigens, this antigens are not expressed on the cell surface. Thus, those antigens are tumor specific.
- tumor antigens produced by oncogenic viruses: some viruses are associated with cancers. The viruses can produce proteins that are recognized as foreign by the immune system. HBV and HPV have latency antigens which are recognized by CTLs. Those antigens are good for immunization of person.
- cell surface glycoproteins and glycolipids: are expressed in a higher level or in an abnormal forms. In this included: CA-125 expressed in ovarian carcinomas, MUC-1 in breast carcinomas (isn’t it overexpression???)
- differentiation antigens: are specific for particular lineage or differentiation step of various cell types. Example: certain lymphomas may be diagnosed as B cell derived tumors due to the presence of DC10 and CD20 which is characteristic for this lineage. Antibodies against these molecules are used for tumor immunotherapy.
*TSA has more role in protecting from tumor development than the TAA, but TAA is better for the detection of the cancer, controlling the affectivity of the treatment and using the epitope for immune therapy.
Waht are the antitumor effector mechanisms?
Cell-mediated immunity is the dominant anti-tumor mechanism.
-
Cytotoxic T lymphocytes: Neoplastic cell has different Ag (TAA or TSA). They are presented by MHC1 molecule on the cell surface and this is recognized by CD8+ T lymphocytes that can kill the cell.
- in some cases, such cells don’t develop spontaneously but they can be generated by immunization with tumor antigen-pulsed DC.
- Natural killer cells: are able to kill tumor cell without prior sensitization → 1st line of defence. Tumors that don’t express MHC1 (hence, cannot be killed by T cells) are killed by this cells. Stress induced Ag: are expressed on tumor cells and cells with a DNA damage. Stressed induced antigens → activation of NK receptors → perforine, granzyme B → killing of the neoplastic cell.
- Macrophages: T cells and NK cells release INFγ → activation of macrophage → ROS, TNF → killing of the tumor cells
- Humoral mechanisms: don’t play a role in the anti-tumor effects, but monoclonal antibodies against tumor cells are used therapeutically. Example: Ab against CD20, a B cell antigen, are used in the treatment of non-Hodgkin’s lymphoma.
Immune surveillance and tumor escape mechanisms:
how does the neoplasm manages to escape the immune surveillance?
- clonal selection mechanism → selective outgrowth of antigen-negative variants: the strongly immunogenic sub clones are eliminated.
- loss or reduced expression of the MHC1 molecules: by that, they escape Tc mediated killing (but are still susceptible to NK cells killing)
- immunosupression: neoplastic cells can release products, such as TNFβ, which is a potent immunosuppressant. Moreover, the immune response induced by the tumor may inhibit tumor immunity, for example, by activation of regulatory T cells
- masking antigens: glycoproteins which covers the antigens → non immunogenic
- neoplastic cells can cause apoptosis. By secreting FAS ligand → apoptosis of T cells
Cancer epidemiology
- Cases of death per year
- Rate of the causes of mortality in the entire world?
15 million cases of death per year from cancer are expected.
Rate of the causes of mortality in the entire world:
- infectious diseases
- cardiovascular disease
- tumor
- **Not sure it’s correct
In devloped countries it is in the 2nd position, as the health system is developing it will become the 1st (already in some countries)
20% of deaths are related to cancer
Distribution of cancer by sex
Men/Women
- Mobidity:
- Prostate/Breast - 25%/26%
- Lung - 15%/14%
- Colon - 10%/10%
- Mortality
- Lung - 30%/26%
- Prostate/Breast - 10%/15%
- Colon - 8%/9%
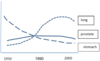
Graph!!
Prostate: related to old age; easier to treat; controlling and screening improved
Breast cancer: good therapy; mammography
Lung: hard to treat; 10-15 years latency; due to smoking
Stomach: the storage of food improved; used to preserve food with smoke (carcinogenic)
Colon: improved with fiber rich food
Distribution of cancer by age
There are 2 peaks oc cancer occurance according to age:
- At the age of 5: small round cell cancers → most probably generated by undifferentiated germ cells (ectodermal blastoma). the major lethal cancers in children are leukemia, neuroblastoma, soft tissues sarcomas, bone sarcomas, tumors of the CNS, lymphomas
- At the ages 65-70: due to accumulation of somatic mutations and decreasing of immunity at that age. After that age, the incidence is declining, as susceptible individuals were selected before.
Geographic distribution of cancer
In japan: stomach cancers
Mid Asia: esophagus (hot drinks)
India: oral (betel plant)
Developing countries: hepatocellular carcinoma
Geographic distribution is rather environmental and is more related to food, diet, habits and infectious diseases in the population.
2/3 of cancers are due to environmental factors
1/3 are related to genetics
The most important environmental exposures linked to cancer include the following:
- Alcohol: cause cirrhosis, liver cancer, oral cavity and laryngeal cancer,
- Infectious diseases: HBV, HCVincrease in the hepatocellular cancers
- Smoking: Oral, laryngeal, kidney, urinary bladder, Pancreas.
- Obesity: Colorectal
- cervial cancer: is expected to disappear from the world due to the widespread use of cytologic smear studies for early detection of the tumor while it is still curable.
- prostate and colon: the occurrence should decrease as there is a good screening technology and there is a good treatement
- Lung cancer should decrease because of the strong restriction of cancer
Preneoplastic lesion state development
- What are the 3 possible outcomes of a precancerous lesion?
Reversible state: dysplasia → indicates high chance for cancer
It is a precancerous state that may:
- Remain as it is, without changing
- May regress to normal if the stressful agent is removed
- May proceed to cancer
What are the two types of precancerous states?
- Obligae: 100% for developing a cancer. In this group falls the autosomal dominant hereditary cancers, for example: adenomatous polyposis coli.
- Facultative: genetic and environmental factors both contribute for the developing of the cancer.
List the conditions which are considered as precancerous states
-
increased regeneration:
- cirrhosis → increased regeneration → hepatocellular carcinoma
- Squamous cell carcinoma in the margins of a chronic skin fistula
- Pajet disease: there is a continuous osteoclastic and osteoblastic activity → reorganization of the trabecular bone → osteogenic sarcoma
-
hyperplasia:
- high estrogenic effect → hyperplasia of uterus → cancer
- Smoke → hyperplasia of mucus membrane → metaplasia → dysplasia → cancer
-
infectious disease: invasion of inflammatory cells that
- secret ROS → mutation in the DNA
- secret IL, IFNγ, cytokines → push the cell to proliferate (initiation-promotion)
- Example: ulcerative colitis → colon cancer, helicobacter pylori infection → gastric carcinoma
-
immunedeficiency:
- AIDS patient tend to suffer from lymphoma, astrocytoma
- Transplanted patients: suffer PTLD (post-transplant-lymphoproliferative-disorder) which have different lymphomas, skin cancers.
-
benign neoplasm: has a chance to transform to malignant. There is a grading method which evaluates the risk for transforming into malignant tumors (never, low, intermediate, high)
- high chance are the polyps adenoma of the skin and intestine.
- Intermediate: hepatocellular adenoma
- Low: leiomyoma (1-2% to become sarcoma)
- Never: hypophysial adenoma
Morphology of precancerous states:
- intraepithelial neoplasia
Cervical intraepithelial neoplasia (CIN):
in the cervix there is the squamo-columnar junction.
Layers:
- basement membrane-basal
- layer-polygonal
- layer-planocellular
Based on the degree of replacement:
- If 1/3 of the epithelium is replaced by the basal cells -> CIN1
- If 2/3 of the epithelium is replaced by the basal cells -> CIN2
- If is fills the entire epithelium -> CIN3
- If it disrupts the basement membrane and infiltrate the deeper structures -> carcinoma
Other terminology: SIR (squamous intraepithelial lesion). 2 grades:
Low-SIR: low chance for transformation into cancer (CIN 1+2)
High-SIR: high chance for transformation into cancer (CIN3)

What is PAP smear
a doctor scratches cells of the squamo-columnar junction with a stick. The smear is analyzed cytologically:
- P1-P2: means normal. The difference between the 2 is based on the state of the woman (pre/post menopausal)
- P3: un-certainty, the examination should be repeated
- P4: dysplasia
- P5: cancer
Any lady who has active sexual life or is after it should visit gynecologist once a year to make PAP smear. If:
- P1/P2: the lady should return next year
- P3: repeat 1 month later
- P4,P5: make cone resection. Analyze the histology of the resected area.
- Based on this, grading: CIN1/2/3, high-SIL, low-SIL.
- If the category is CIN1-3, than this is non-invasive and there is no chance for reoccurrence (“problem is solved”). However if it is invasive (infiltrative), chemotherapy should be performed.
Morphology of precancerous states:
- Leukoplastia
Leukoplastia= white spot.
May occur in the oral cavity, vulva, glans of penis. Considered as potential precancerous state, because based on the macroscopy we cannot say it is cancer, just by histology.
In order to have a proper evaluation of the state of the patient what should be done?
We have to grade and stage the cancer according to: how much the tumor is differentiated, anaplastic, spread.
Explain grading and staging
Grading: to assess the aggressiveness of the tumor and the level of malignancy based on the degree of differentiation or anaplasia.
- Differentiated = better prognosis
- Less differentiated/anaplastic = worse prognosis
Grade I, II, III, IV. Problems with this grading system:
- Has a low correlation with the real biological behavior of the tumor because there are exceptions: highly differentiated cancers with very aggressive behavior and also the opposite way around.
- Subjective
- Still this system is used.
Staging: the degree of spreading of the cancer.
- T: the size of the tumor (how big/deep) T1-T4
- N: how many lymph nodes are affected N0-N3 (NX - don’t know)
- M: metastasis M0-M1 (MX - don’t know)
THERE IS NO RELATION BETWEEN GRADING AND STAGING!
Explain the staging of colon cancer
Layers of the colon (from the innermost to the outermost):
- Mucosa (with the crypts)
- Muscularis muscosa
- Submucosa
- Muscularis propria
- Peritoneum
T1= affects the mucosa, but does not reach the muscularis mucosa
T2= affecting submucosa, does not reach the muscularis propria
T3= affecting the muscularis propria, does not reach the peritoneum
T4= penetrating through the peritoneum
Nx= don’t know
N0= none
N1= 1-3 lymph nodes are involved
N2= more than 4 lymph nodes are involved
Mx= unknown
M0= no
M1= yes
Stage, TNM, survival, treatment table
Stage | TNM | survival | treatment
I | T1-T2 N0 M0 | 95% | Surgery
II | T3-T4 N0 M0 | 75-85% | Surgery
III | T1-T4 N1 M0 | 40% | Surgery
IV | M1 | 10% | Chemotherapy

Which other staging system do you know? or at least need to know
Mostly used for solid tumors, the TNM is used.
Some tumors cannot be classified according to this method, thus, other staging systems are used:
- Rai staging (lymph node involvement, organ involvement): CLL (chronic lymphoid leukemia)
- An-Harbor staging: Hodgking’s lymphoma
What are the local effecets of tumor
related to the local growth and expansion of the primary tumor or the metastatic tumor.
They can lead to death by:
- Ulceration which may cause bleeding or infection (and sepsis)
- Infarcts due to vessels compression
- Intussusception and intestinal obstruction or infarction
**70**
Cancer pathology, genetic, immunologic and molecular diagnostics:
- Morphologic methods
-
excision or biopsy: for biopsy, one should be aware that the margins are not representative and the center might be necrotic.
- Frozen-section: sample is quickly frozen and sectioned. Enables rapid evaluation.
- fine needle aspiration: involves aspiration of cells from a mass followed by cytologic examination of the smear. Used most commonly with palpable lesions, although modern imaging techniques permit detection of deeper structures (liver, pancreas, pelvic lymph nodes).
- cytologic smears: neoplastic cells are less cohesive, thus they are shed into fluids or secretions. The shed cells are then evaluated for features of anaplasia indicative of their origin from a tumor.
-
immunocytochemistry: using labeled monoclonal antibodies, this method enables:
- detection of PSA (prostate-specific antigen) in a metastatic depositsdiagnosis of a primary tumor in the prostate
- detection of estrogen receptors: for prognSaveostication and therapy intervension in breast cancer
- diagnosis of undifferentiated carcinoma from large-cell lymphoma based on the presence of cytokeratin
- flow cytometry: used for classification of leukemia and lymphoma. Fluorescent antibodies against cell surface molecules and differentiation antigens are used to obtain the phenotype of the malignant cell.
Cancer pathology, genetic, immunologic and molecular diagnostics:
- Tumor markers
- PSA: is used to screen for prostatic adenocarcinoma. Problems: may be elevated in benign prostatic hyperplasia. No cut-off level that tells if the patient has cancer or not.
- CEA: Carcinoembryonic antigen is elaborated by carcinoma of the breast, pancreas, stomach and colon.
- α-fetoprotein: produced by hepatocellular carcinoma, yolk sac remnants in the gonads and embrional cell carcinoma.
Cancer pathology, genetic, immunologic and molecular diagnostics:
- Molecular diagnosis
- diagnosis of malignancy: several neoplasms are defined by particular translocations, on which the diagnosis is based. They can be detected by FISH or PCR. For example: PCR based detection of BCR-ABL transcripts provide the molecular diagnosis of chronic myeloid leukemia.
- prognosis and behavior: FISH and PCR are used for detection of genetic alterations associated with poor prognosis. For example: amplification of oncogenes such as HER-2/NEU and N-Myc in breast cancer and neuroblastoma.
- detection of minimal residual disease after treatment: for example: BCR-ABL detection by PCR after treatment of chornic myeloid leukemia.
- diagnosis of hereditary predisposition to cancer: detection of germ line mutations of tumor suppressor genes such as BRCA1.
Molecular profiling of tumors
By DNA microarray analysis, a technique which enables simultaneous measurments of the co-expression levels of several genes.
Process: in the notes



