8 - Breast Flashcards
How do you do a breast examination?

Introduction: usual, chaperone, position at 45 degrees with blanket
Inspection: hands by side for one inspection, hands on hips for second inspection and leaning forward with hands behind head to accentuate skin dimpling, look for skin changes (puckering, peu d’orange), nipple discharge or inversion, look at axillae too. Squeeze nipple
Palpation: ask patient to place both hands behind head. Palpate all 4 quadrants then Tail of Spence. If you palpate any lumps, note their position, size, shape, consistency, overlying skin changes, and mobility. Palpate axilla lymph nodes and cervical
Complete: thank patient and say you would follow up with mammography and/or US with biopsy if neccessary

What is the breast triple assessment?
Hospital-based assessment clinic that allows for the early and rapid detection of breast cancer. GOLD STANDARD. Referred here if 2 week wait or suspicious changes on routine mammogram
1. History and Examination
2. Imaging (Mammography or US if <35 years old or male)
3. Histology (core biopsy as full histopathology)

Why is there two types of imaging in the triple assessment?
Ultrasound needed if <35 as breast tissue is more dense so will not see microcalcifications or mass lesions on a mammography

Why is a core biopsy taken for breast lesions not FNA?
- Higher specificity and sensitivity than Fine needle aspiration (FNA)
- Allows full histology so can differentiate between in-situ/invasive carcinoma so can stage but FNA is only cytology
- If woman has recurrent cystic disease she can have FNA for symptom relief and cytology

How are the results of each stage of the triple assessment used to grade the suspicion for malignancy?
The key is to decide whether the patient should go onto have a more definitive biopsy and further intervention

Galactorrhoea is copious, bilateral, multi-ductal, milky discharge, not associated with pregnancy or lactation. What is the aetiology for galactorrhoea?
- Hyperprolactinaemia: (see image)
- Normoprolactinaemic galactorrhoea: diagnosis of exclusion. idiopathic and can be reassured and observed

What hormones control lactation, what gland releases prolactin?
- TRH and Oestrogen stimulate Prolactin production
- Dopamine inhibits prolactin production
- Prolactin made by anterior pituitary gland

What should you clarify in the history of a patient presenting with galactorrhea?
- Need to determine if true galactorrhoea (multi-ductal milky white nipple discharge, typically bilateral). Can be done with Sudan IV stain for fat droplet
- Additional features: breast lumps, mastalgia, LMP
- Check for any visual changes (compressive pituitary masses) or features of hypothyroidism
- DHx: including contraception, OTC, recreational
- Breast exam usually remarkable

What investigations are done when a woman presents with galactorrhea?
- Exclude pregnancy if of reproductive age with B-hCG
- Serum prolactin levels (if >1000mU/L in the absence of a drug cause then suggests prolactinoma)
- Check TFTs, LFTs, U+E’s
- If suspect pituitary tumour e.g PRL>1000 MRI with contrast
- If breast lump or lymph nodes then breast imaging

How is galactorrhoea managed?
- Pituitary tumour: dopamine agonist (e.g Cabergoline and Bromocriptine) and referral for possible transphenoidal surgery
Idiopathic normoprolactinaemic galactorrhoea: usually resolves spontaneously but can give low dose dopamine agonist
Intolerant to medication galactorrhoea: bilateral total duct excision

What time of the day should a blood sample for prolactin levels be taken?
First thing in the morning they are highest so need to be taken 3-4 hours after waking
What are the different classifications of mastalgia?
- Cyclical: affects both breasts due to hormonal changes. often starts few days before menstruation and subsides at the end. also women on HRT get this
- Non-cyclical: unrelated to menstrual cycle e.g hormonal contraceptives, anti-depressants (sertraline) or antipsychotics (haloperidol).
- Extra mammary: chest wall or shoulder pain

If a patient presents with mastalgia what are some things you need to find out from the history?
- Any lumps, skin changes, fevers, or discharge?
- Associated with menstrual cycle?
- DHx?
- Pregnancies/Breast-feeding?
- FHx?
- PMH
How is mastalgia investigated and managed?
Ix
- If no other symptoms no imaging
- Pregnancy test
Mx
1st: Reassurance and Pain control: firm bra in day and soft bra at night, oral ibuprofen/paracetamol or topical NSAIDs
2nd: Refer to specialist if above doesn’t work and give Danazol (anti-gonadotrophin agent) but has severe s/e of nausea, dizziness and weight gain

How does mastitis present, what causes it and how is it managed?
Inflammation of the breast tissue, can be acute or chronic. Often due to infection by S.Aureus
Features: tenderness, swelling, induration, erythema, need to check area for abscess formation
Management:
1st Line: Continue breast feeding and analgesics
2nd Line: If systemically unwell or not improved in 24-48 hrs then flucloxacillin
3rd Line: I+D

How do breast abscesses due to mastitis present and how are they managed?
A collection of pus within the breast lined with granulation tissue usually due to acute mastitis
Features: tender, fluctuant, erythematous masses, sometimes with a puncutum. Systemic symptoms like fever and lethargy
Ix: US if diagnosis in doubt
Mx: prompt empirical antibiotics and US-guided needle therapeutic aspiration. if advanced may need I+D under local anaesthetic

What is a complication of draining a non-lactational abscess?
Formation of a mammary duct fistula (a communication between the skin and a subareolar breast duct)
Treated by fistulectomy and antibiotics but can recur

How do breast cysts present and how are they investigated and managed?

Epithelial lined fluid-filled cavities, which form when lobules become distended due to blockage, usually in the perimenopausal age group
Features: distinct smooth masses that can be tender and in both breasts
Ix: halo shape on mammography and diagnosed by US
Mx: often self-resolve so reassure but if large can aspirate

How can you tell whether a breast cyst is malignant or not by US?

Aspirate either free hand or US guided.
Can exclude cancer if lump disappears on US after aspiration or if fluid free of blood. If not then send cystic fluid for cytology

What are some complications of breast cysts?
- 2% have carcinoma at presentation but not related to the cyst
- 2-3X more risk of developing breast cancer in the future if you have had a cyst
- May develop fibroadenosis (fibrocystic change) by multiple small cysts which causes tenderness and asymmetry which can mask malignancy
- Any cyclical pain can be treated with gamolenic acid (GLA) or danazol.

What is mammary duct ectasia, how does it present and how is it investigated and managed?
Dilation and shortening of the major lactiferous duct usually in perimenopausal women
Features: coloured green/yellow nipple discharge (if blood stained needs triple assessment), a palpable mass, or nipple retraction.
Ix: Mammography with calcified dilated ducts and no other signs of malignancy. Can take biopsy which will show multiple plasma cells
Mx: Conservatively if malignancy can be excluded by radiology. If recurring nipple discharge then duct excision

How does fat necrosis of the breast present and how is it investigated and managed?
Acute inflammatory response leading to ischaemic necrosis of fat lobules. Often due to either blunt trauma or previous breast surgery/radiological intervention
Features: usually asymptomatic or painless lump. If acute inflammatory response continues then chronic fibrotic change can occur forming solid irregular lump
Ix: Positive traumatic history and/or hyperechoic mass on US. Look like malignancy on mammogram if fibrotic lesion so core biopsy
Mx: Self limiting so reassure and analgesics

What is the pathophysiology of gynacomastia?
Physiological: in adolescence due to the delay in testosterone surge to oestrogen in puberty and in elderly as testosterone declines
Pathological: due to changes in oestrogen:androgen ratio (see image)

How does gynaecomastia present and what is the differential diagnosis?
Insidious onset, rubbery or firm mass (typically >2cm diameter) that starts from underneath the nipple and spreads over breast
Need to do testicular exam as well, especially if young
Psuedogynaecomastia: due to being overweight. pinch to see if obvious disc of breast tissue

How is gynaecomastia investigated?
- Tests only necessary if cause unknown. Check LFTs and U+E’s then if these are normal take hormone profile of LH and testosterone
- If malignancy suspected then triple assessment

How is gynaecomastia managed after investigations?
- Treat underlying cause
- Reassurance
- Tamoxifen can be given to alleviate tenderness
- If fibrotic changes then surgery is only option if other medical treatments failed

What is breast carcinoma in situ and what are the two types?
Malignancies contained within the basement membrane. Seen as pre-malignant and often asymptomatic as found incidentally on imaging
Ductal (DCIS) or Lobular (LCIS)

What are the subtypes of DCIS and how is it investigated and managed?
Most common type of non-invasive breast cancer. Malignancy of the ductal tissue that turns invasive in 20-30% of cases left untreated
Subtypes: comedo, cribriform, micropapillary, solid, mixed
Ix: often found by microcalcifications on mammography which are confirmed on biopsy
Mx: Localised DCIS complete wide excision ensuring all margins have no residual disease. Multifocal or widespread DCIS needs complete mastectomy

How is LCIS investigated and managed?

Malignancy of secretory lobules of the breast that is contained within the basement membrane. Rarer than DCIS but more likey to turn invasive. Most occur before menopause
Ix: asymptomatic and found on mammogram but not usually microcalcifications, found on biopsy!!
Mx: if low grade then monitor, if invasive Tamoxifen and bilateral prophylactic mastectomy if BRCA1/2

What is the most common to least common histology for breast cancer?
Breast cancer is the most common cancer worldwide Almost all arise in the terminal duct lobular unit.
Invasive Ductal Carcinoma (No Special Type): most common, split into subtypes tubular, cribriform, papillary, mucinous, or medullary with latter two being worst prognoses
Invasive Lobular Carcinoma: second most common and more common in older women, diffuse pattern of spread so hard to diagnose and usually large by diagnosis

What are some risk factors for developing breast cancer?
- Female
- Age (risk doubles every 10 years after menopause)
- BRCA1/2 (tumour suppressor genes)
- FHx in first degree relative
- Previous benign disease
- Obesity
- Alcohol
- Early menarche and Late menopause
- Nulliparous women or first child over 30
- COCP/HRT

What are some visible changes to the breast that can cause a woman to seek medical advice as she is concerned about breast cancer?
- Lump in breast or axilla
- Asymmetry
- Swelling (all or part of breast)
- Abnormal nipple discharge
- Nipple retraction
- Skin changes (dimpling/peau d’orange, or Paget’s-like changes)
- Mastalgia

What is the prognosis with breast cancer?
- Nottingham Prognostic Index (NPI)
- Nodal status is the biggest prognostic factor
- Also look at receptor status (HER2, PR, ER) and vascular invasion for prognosis

What is involved in the NHS Breast Screening Programme?
Woman are invited to have a mammogram every 3 years from 50-70.
Any abnormalities will be sent for triple assessment

What is Paget’s disease of the nipple and how does it present?
Presents as a roughening, reddening, and slight ulceration of the nipple and often has underlying neoplasm
Itching or redness in the nipple and/or areola with flaking and thickened skin. Often painful and sensitive. Can also be flattened

Paget’s disease can often be mistaken for dermatitis/eczema. How can you tell the difference between the two?
Paget’s always involves the nipple but eczema often only affects the areola and spares the nipple

How is Paget’s disease of the nipple investigated and managed?
Ix:
- Biopsy (often whole nipple removed for histology)
- Breast and Axilla exam, Mammogram, US, MRI breast
Mx:
- Surgery: nipple and areola removed
- If underlying malignancy needs radiotherapy

What surgical treatments are available for breast cancer?
Breast Conserving
- Only for local disease with no metastatic spread
- Wide Local Excision (WLE) with 1cm margin of normal tissue
Mastectomy
- Removes all breast tissue and some overlying skin. Amount of skin depends on if reconstruction. Chest wall left intact
- Done in multifocal disease, high tumour:breast tissue ratio, disease recurrence, or patient choice
Axillary Surgery
- Alongside mastectomy and WLE
- Sentinel node biopsy by injecting blue dye in paraareolar area to find which lymph node drains the tumour first and remove them for histology
- Axillary node clearance removes all nodes in the axilla

What are some complications with axillary node clearance surgery?
- Paraesthesia
- Seroma formation
- Lymphoedema of the upper limb

What is a risk-reducing mastectomy and which patients have these?
Removing breast tissue in those at a high risk of developing breast cancer. Often referred to genetic counsellor if at risk

How are the hormone treatments Tamoxifen and Aromatase Inhibtors used to treat breast cancer?
Often given adjuvantly after primary surgery or if elderly/unfit for surgery this is the primary treatment
Tamoxifen (SERM) Blocks oestrogen receptors so prophylactic. Protects bones from osteoporosiss. However increases risk of endometrial cancer and of thromboembolisms during/after surgery and during immobile perioids. Used in pre-menopausal women for 5 years
Aromatase Inhibitors (Anastrozole, Letrozole, or Exemestane): Bind to oestrogen receptors to stop further malignant growth, stop further oestrogren production and stop conversion of androgens to oestrogen in peripheral tissues.
Given as adjuvant therapy in post-menopausal women instead of tamoxifen, but more expensive.
Can cause osteopenia and pathological fractures

When are breast cancer patients offered adjuvant radiotherapy?
Ater WLE and post-mastectomy cases with positive resection margins, tumour size >5cm, or 4 or more pathological nodes in axilla
What is the most common immunotherapy used for breast cancer? What is the major side effect?
Herceptin (Trastuzumab): Monoclonal antibody that targets HER2 positive malignancies
Either used as adjuvant or monotherapy in patients who have received at least two chemotherapy regimens for metastatic breast cancer
SIDE EFFECT OF CARDIOTOXICITY so monitor cardiac function before and during treatment

Oncoplastic management is a new approach to treating breast cancer that works by conserving breast tissue. What is a therapeutic mammoplasty?
WLE with breast reduction
Smaller lifted breast with nipple and areola preserved along with blood supply and nipple moved to suit new breast

Flap formation is another oncoplastic treatment for breast cancer. What are the different techniques that can be used for this treatment?

Latissimus Dorsi Flap: involves a portion of the Latissimus Dorsi muscle and its overlying skin used to reconstruct the removed breast as free or pedicle flap. Only for reconstructing smaller breasts as small muscle
Transverse Rectus Abdominal Muscle (TRAM) Flap: Uses skin, abdominal muscle and fat to reconstruct breast as free or pedicle flap. Advantage of removing abdominal fat but weakens abdominal muscles
Deep Inferior Epigastric Perforator (DIEP) Flap: Tissue from the abdomen and its overlying skin to reconstruct breast but only free flap. Advantage over TRAM is that it doesn’t compromise abdominal muscle strength

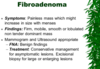
What is a fibroadenoma?
- Usually in those aged below 30. Overgrowth of collagenous mesenchyme of one breast lobule.
- Firm, smooth, mobile lump that is painless
- Observation and reassurance. Can excise if large
How do you screen for distant metastases in breast cancer?
- FBC, U+E’s, LFTs, Calcium
- Tumour markers
- CT Chest/Abdo/Pelvis
- Bone scan
When would you do an MRI breast for a suspected breast carcinoma?
- FHx (High risk or BRCA1/2 carriers)
- Dense breasts
- Young cancers
- Lobular cancers
What are the standard views on mammography?
- Craniocaudal (CC)
- Mediolateral Oblique (MLO)
Use MLO instead of ML as get more tissue involved (upper outer quadrant) for less exposure. Tough to localise lesions though as CC and MLO not 90 degrees to one another

When is US used for breast lesions and how can you tell when youve found a breast cyst on US?
- Under 35’s, guided biopsy, palpable lump with negative mammogram findings, breast implant rupture
- Malignant lesions: power doppler, get patient to say ‘ahh’ and observe the centre of the lesion. if cancer will light up, if benign will not as full of fat

What are the chemotherapy and radiotherapy regimes for breast cancer?
Radiotherapy: 40Gy in 15 fractions
Chemotherapy: 3 weekly combination therapy (Cyclophosphamide, Epirubicin, 5FU) in 6-8 cycles. Use taxanes in high risk patients
What is the abnormality on this mammogram?

Cluster of suspicious calcifications which could indicate DCIS.
Calcification is an early indication that cells in the area are dividing more than normal. Put some guide wires in to help the surgeon
Popcorn calcification and large calcifications are not as suspicious as clusters of random calcification

If a woman has a WLE for a breast malignancy, if there is recurrence what treatment options are available?
- Can only have WLE again if she didn’t have radiotherapy the first time as cannot have radio twice as will cause endarteritis and necrosis
- Mastectomy
What is hormone therapy and what is immunotherapy for breast cancer?
Immuno: Herceptin
Hormone: Tamoxifen and Exemestane
When giving a woman hormone therapy for breast cancer treatment when should you give her bone protection?
Aromatase Inhibitors will need bone protection, not SERMs
- Give all patients Adcal D3
- If <75 do a DEXA scan to see if needs extra bone protection by giving Adcal and Alendronic Acid
- If >75 give extra bone protection regardless
What can cause calcifications on a mammogram that aren’t necessarily indicative of a malignancy?
Previous breast surgery
What surveillance takes place after breast cancer has been given ‘the all clear’?
5 year surveillance before returning to normal screening. Have an annual mammogram and access to an Open Clinic
What might you see on an US of a breast lump that might indicate malignancy?
Lump: skin thickening, poorly defined edges
Lymph nodes: may not see hilum as cancer has taken over
Where are all of the different axillary lymph nodes and how do you palpate them?

Have patient relax over over your opposite arm

Which groups of people is duct ectasia more common in?
Part of normal aging process but more common in perimenopausal smokers
What is the differential for clear nipple discharge?
Intraductal papilloma
What is the definition of gynaecomastia?
Male enlargement of glandular breast tissue (not fatty tissue)
What is the difference between sensitivity and specificity of a screening test?
GO LOOK AT POP SCI
Sensitivity: the ability of a test to correctly identify patients with a disease
Specificity: the ability of a test to correctly identify people without the disease

What are some factors that a disease needs so that a screening test can be developed?
- Common disease
- Must be able to recognised in early stages
- Must do more benefit than harm
- Must have a treatment
What are some harms of breast screening?

What are some factors that determine what treatment option will occur for a patient with breast cancer?
- Patient status (WHO and ASA)
- Tumour status (Size, ER, HER2)
- Operation selection
If a patient has oestrogen positive breast cancer, what hormone therapy are they offered?
- Tamoxifen if pre-menopausal
- Aromatase inhibitors (Leterozole) if post menopausal
What is the cut off size for a WLE breast cancer?
<4cm


