2 - General and T&O Imaging Flashcards
(71 cards)
What are the different types of imaging that can be done for abdominal pathology and what are they used for?
AXR: suspected bowel obstruction, suspected perforation (erect CXR), moderate to severe undifferentiated abdominal pain, suspect foreign body, renal tract calculi follow up
CT: abdominal trauma, suspected intra-abdominal collection, malignancy
US: RUQ
Endoscopy: acute upper GI bleed

How should you present any x-ray in general?

How should you read an abdominal x-ray?
AbdoX
A: air - where it should and should not be- Should only be in the lumen, erect x rays are more sensitive
B: bowel - position, size and wall thickness- 3-6-9 rule
D: dense structures, calcification and bones- calcified renal tract/ gallstones
O: organs and soft tissues- remember lung bases
X: eXternal objects and artifacts

How should you read a CXR?
Assess image quality RIPE
R- Rotation- The medial aspect of each clavicle should be equidistant from the spinous processes. The spinous processes should also be in vertically orientated against the vertebral bodies
I- Inspiration- The 5-6 anterior ribs, lung apices, both costophrenic angles and the lateral rib edges should be visible.
P- Projection- Note if the film is AP or PA: if there is no label, then assume it’s a PA film (if the scapulae are not projected within the chest, it’s PA).
E- Exposure- The left hemidiaphragm should be visible to the spine and the vertebrae should be visible behind the heart.

How can you tell the difference between small and large bowel on an AXR?

- In ascites bowel loops are clustered centrally
- 3/6/9 rule
- Thumbprinting when large bowel inflammation

What are some of the causes of pneumoperitoneum and what would you see on imaging this?
Erect CXR: free air under diaphragm, leaping dolphin sign, cupola sign when supine, continuous diaphragm sign
AXR: Rigler sign, Telltale triangle sign

What is Rigler’s sign?
Double wall sign where gas is on both sides of the bowel forming crisp line on bowel that you could draw around.
Sign of pneumoperitoneum

What are the aims of imaging in a bowel obstruction?
- differentiate true mechanical obstruction from ileus or constipation
- find site of obstruction
- identify cause
- assess for complications (e.g. ischaemia or perforation)
- assess the viability of bowel segments involved
What would you find on imaging a bowel obstruction?
AXR:
- Dilated bowel loops 3/6/9
- Perforation
- String of Pearl’s sign
CT:
- Transition point
- Collapsed or normal bowel past transition but dilated before
- Bowel wall thickening
- Surrounding mesenteric fat if inflammation
- Volvulus

What does this AXR show and why does this occur?

Thumbprinting
Sign of large bowel wall thickening usually due to oedema. Haustra become thickened
Causes: UC, Crohn’s, Infection, diverticulutis, lymphoma
What would you use when imaging urolithiasis?
CT KUB non-contrast is gold standard
How can you tell the difference between a sigmoid and caecal volvulus and what are the different aetiologies of these two pathologies?

Sigmoid: chronic constipation, colonic distension, elderly, bed bounds
Caecal: congenital long mesentry, congenital malrotation, congential defect in fixation of the right colon to peritoneum

What does this CT show around the kidney and what does this indicate?

Fat stranding which shows inflammation
What is Rigler’s triad?
Sign of gallstone ileus
- pneumobilia
- small bowel obstruction
- ectopic calcified gallstone, usually in the right iliac fossa
What are the main causes of small and large bowel obstruction?

How does a CT abdomen scan work and what are the advantages and disadvantages of this imaging?
- check renal function
- lie patient supine on CT table
- scout image to plan study
- IV contrast injected via pump-injector
- 60-second delay
- scan from dome of diaphragms to symphysis pubis

What should you look for on a CT with a bowel obstruction?
- Find obstruction
- Find dilated loops before obstruction
- Find collapsed area after obstruction
What are some of the different phases than can be used in CT?
- Non contrast: CT KUB for renal stones or allergic to contrast
- Systemic arterial (35 seconds): vascular imaging can made 3D angiogram
- Portal venous (70 seconds): intravenous contrast, good for acute abdomen imaging and outpatients
- Delayed (depends): urological imaging takes 7-10 minutes
Systemic arterial and portal venous together can see bleeding

When is contrast for CT given orally and through the bladder?
- Orally: to look for leaks and fistulas in the upper GI
- Foley catheter: after pelvic trauma to determine if bladder rupture (extra/intra peritoneal rupture)
How long does contrast take to get to different vessels in the body?

When should you avoid enteric contrast for CT?
Enteric contrast, such as oral or rectal contrast agents used to enhance visualization of the gastrointestinal tract in CT imaging, should be avoided in certain situations, including:
- Known or suspected gastrointestinal perforation: The use of enteric contrast can exacerbate peritoneal irritation and potentially lead to peritonitis if there is a pre-existing gastrointestinal perforation.
- Impaired swallowing or risk of aspiration: Patients who are unable to swallow safely or are at risk of aspiration should not be given oral contrast agents to avoid the risk of aspiration pneumonia.
- Severe dehydration or electrolyte imbalances: In patients with severe dehydration or electrolyte imbalances, the administration of enteric contrast may further compromise fluid and electrolyte balance.
- History of severe allergic reactions to contrast agents: Although enteric contrast agents are generally safe and not absorbed systemically, patients with a history of severe allergic reactions to contrast agents may prefer to avoid them altogether.
- Known intolerance or contraindication to specific enteric contrast agents: Some patients may have specific intolerances or contraindications to certain types of enteric contrast agents, such as iodine-based agents, and alternative agents should be used in these cases.
Always assess the patient’s clinical history and consider the potential risks and benefits before administering enteric contrast for CT imaging. In some cases, alternative imaging modalities or non-contrast CT scans may be more appropriate.
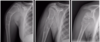
When requesting x-rays for MSK, what do you need to consider?
- Which structures?
- Which views? (two views 90 degrees apart)
- Compare both sides and review previous images
- Correlation with clinical and other imaging findings
How do you review an MSK x-ray?
- Name, Age, Date and Time of X-rays
- What is being imaged and the most obvious abnormality
- Is the image quality and angles satisfactory?
- See image (Bones, Soft tissue, Joint, Anything else)

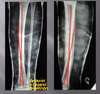
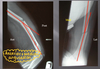
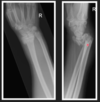
How do you describe a fracture on an x-ray?
- What type of fracture (oblique, transverse etc)
- Where is the fracture (diaphysis, metaphysis, epiphysis)
- Is it displaced (rotation, translation, angulation, length)
- Say where the distal frament is compared to proximal (e.g displaced anteriorly and medially)
- Anything else? (joint involvement, bone lesions, anothe fracture)