11 - T&O General Principles Flashcards
What would be the underlying pathology in the following scenarios:
- Reduced active and passive movements
- Reduced active but full passive
- Joint problem
- Nerve or muscle problem
What is the pathophysiology of OA?
Progressive loss of articular cartilage and remodelling of bone
Chondrocytes in articular cartilage release enzymes to break down collagen and proteoglycans destroying cartilage. Exposure of subchondral bone results in sclerosis and remodelling which causes osteophtes and subchondral bone cysts. Joint space is lost over time

How does OA present and what are some risk factors associated with OA?
Most commonly in hip, knee, small joints of hands and feet
- Insidious gradually worsening pain and stiffness that is worse with activity and relieved by rest
- Deformity
- Reduced range of movement
- Crepitus

What are some differential diagnoses for OA of the hand, hip and knee?
Always consider RA, gout, septic arthritis, fractures, bursitis and malignancy (primary and metastatic)

How is OA investigated and managed?
Ix: often clinical diagnosis but can do radiographs and blood tests to rule out differentials
Conservative: weight loss, physiotherapy, heat/ice packs, joint support
Medical: simple analgesics and topical NSAIDs, intraarticular steroid injections
Surgical: osteotomy, arthrodesis, arthroplasty

What are the 3 main principles of fracture management?
1. Reduce
2. Hold (plaster or surgical)
3. Rehabilatate

What are the principles of reduction in fracture management?

- Restoring anatomical alignment of fracture or dislocation (see image for why)
- Usually done closed in emergency setting
- Ensure patient has sufficient analgesia (sometimes conscious sedation)
- Three people: one to perform reduction, one to provide counter traction, one to apply plaster

What are the principles of ‘hold’ in fracture management?
- Consider if traction needed -when muscle pull strong across fracture site so unstable e.g subtrochanteric NOF, femoral shaft fractures (traction is a pin, screw or wire)
- First 2 weeks non-circumferential plaster cast to allow swelling and not risk compartment syndrome
- If axial instability (fracture able to rotate along its long axis) then plaster should cross joint above and below. If no instability just joint distal to fracture

What are some important safety points to consider during fracture immobilisation?
- Can the patient weight bear? Inform the patient
- Do they need thromboprophylaxis? Yes if non-weight bearing
- Have you given advice on the symptoms of compartment syndrome?
What are the principles of rehabilitation in fracture management?
Intensive period of physiotherapy after immobilisation
Counsel patient of stiffness after cast removal and encourage patient to mobilise any non-immobilised joints from the get go
Very important in elderly patients!
What is the process of fracture healing and how long does it take?
- Haemotoma (lasts 1-2 weeks) = granulation tissue
2. Fibrocartilaginous Tissue = granulation tissue forms
3. Bony Callus (lasts 2-3 weeks) = endochondral ossification forms spongy bone. Can see callus on X-ray 2-3 weeks after injury
4. Bone remodelling (lasts months) = spongy converted to cortical bone. Bone only remodels with stressors so important not to immobilise
BONE HEALING TAKES 6-8 WEEKS ON AVERAGE

How do the following effect fracture healing?
- External fixation
- Intramedullary nails
- Screws and plates
External fixation: secondary bone healing
Intramedullary nail: does not cause full rigidity so still alows some movement at fracture site. Reaming causes disruption to blood supply in inner 2/3rds of diaphysis but doesn’t stop external callus formation. Secondary bone healing
Screws and Plates: primary bone healing

What factors contribute to non and mal-union of bone after a fracture?
Non-union: poor blood supply or bone instability (tobacco use, DM, obesity)
Malunion: bone not properly immobilised, having cast off to early, never having treatment for a fracture

What bones is malunion/non-union more common in and how may this pathology present?

- Persistent pain at the fracture site or reduced ROM
- A persistent gap with no bone spanning the fracture site
- No progress in bone healing when repeated imaging studies are compared over several months
- Inadequate healing in a time period that is usually enough for normal healing
- May have OA if malunion occurs near a joint
How is malunion/non-union treated?
Malunion:
Refracture the bone and realign with plates and screws or use a bone graft
Non-union: (FAILURE TO HEAL AFTER 9 MONTHS)
Non-surgical: US stimulator EXOGEN
Surgical: bone graft or biologics (bone morphogenic proteins)

How does smoking affect fracture healing?
Nicotine can slow fracture healing by killing osteoblasts and lowering estrogen effectiveness
- Smoking can counter the antioxidant properties of vitamins C and E.
- Smoking reduces blood supply to healing fracture
- Smoking lowers calcium absorption
-

When a patient presents with an acutely swollen joint, what are some important questions to ask to rule out differentials?
- Establish onset, site, timeframe of swelling
- Ask about any precipitating factors (e.g trauma or surgery) and any exacerbating or relieving factors
- Find out ability to weight bear
- Ask about systemic symptoms
- Has it happened before?
- PMH and DHx

How do you examine an acutely swollen joint?
- A to E assessment
- Look, feel, move
- Look for any redness, skin changes, swelling, temperature changes and compare with contralateral joint
- Check for any focal tenderness and joint effusions
- Look for other joint involvement or systemic signs

What investigations should you do for an acutely swollen joint?

- Routine bloods (FBC, CRP, ESR, serum urate for gout)
- Plain film radiographs (especially if trauma)
- Joint Aspiration (look at opacity, colour and presence of frank pus then sent for WCC and microscopy)

What are some differential diagnoses for an acute monoarthritis?
ALWAYS EXCLUDE SEPTIC ARTHRITIS
- Haemarthrosis
- Crystal arthropathies
- Rheumatological causes
- OA
- MSK injury
- Spondyloarthropathies (reactive arthritis, psoriatic arthritis, ankylosing spondylitis)

Gout and Pseudogout can cause an acutely swollen joint. What are they and how are they managed?
Gout
- Inflammatory arthritis due to monosodium urate crystals in a joint from hyperuricemia.
- Usually in 1st MTP joint and is episodic and triggered by stress, illness and dehydration
- Diagnose with joint aspiration and microscopy
- Treat acute episode with NSAIDs
- Treat multiple episodes or extraarticular features with prophylactics like allopurinol
Pseudogout
- Due to calcium pyrophosphate crystals and often affects more proximal joints (knee and wrist)
- Risk factors of advanced age, hyperparathyroidism, hypophosphatemia
- Positively birefringent rhomboid shaped crystals
- Give NSAIDs and treat any underlying cause

What investigations can show a swollen joint may be due to RA? What management should be initiated?
- Raised inflammatory markers (CRP and ESR)
- Normocytic anaemia
- RF and Anti-CCP levels
- Plain raidiograph with LESS
Give NSAIDs, start DMARDs or biologics

What is the diagnostic criteria for RA?
EULAR classification
Score of 6 or more is definite RA
Looks at joint distribution, serology, symptom duration, acute phase reactants

What are spondyloarthropathies?
Group of seronegative conditions (RF negative) associated with HLA-B27
See image for list of conditions
All can present with axial arthritis or any joint and can cause enthesitis and dactylitis

How is a haemarthrosis formed and how is it managed?
- Traumatic injury (e.g meniscal or ligament injury), bleeding disorders, on anticoagulants
- Ix: routine bloods including clotting, plain film radiographs, joint aspiration
- Mx: conservatively with RICE, analgesia and correcting any underlying coagulopathies

What is the pathophysiology and outcomes of an open fracture?
- Direct communication between fracture site and external environment (includes penetration into rectum and vagina)
- In-to-out or out-to-in mechanism
- Most common open: tibial, phalangeal, forearm, ankle, metacarpal

How are open fractures classified?
Gustillo Anderson Classification
Always check neurovascular status and any evidence of contamination
Identify need for plastic surgery early

How are open fractures investigated?
- Bloods including clotting screen and G+S
- Plain film radiograph
- CT if comminuted or complex
How are open fractures managed initially?

- Resuscitation and stabilisation
- Wound Irrigation, Remove any gross debris and dress with saline-soaked gauze, DO NOT WASH OUT
- Broad spectrum antibiotic cover (CO-AMOXICLAV OR MEROPENEM OR CLINDAMYCIN IF ANAPHYLACTIC P ALLERGY)
Surgical fixation may occur. Most importantly, Surgical debridement
- Tetanus vaccination
- Photograph the wound

What is the definitive management for an open fracture?
- Surgical debridement within 12-24 hours, removing any devitalised tissue. If contaminated debride immediately
(Debridement is a procedure for treating a wound in the skin. It involves thoroughly cleaning the wound and removing all hyperkeratotic (thickened skin or callus), infected, and nonviable (necrotic or dead) tissue, foreign debris, and residual material from dressings.)
- Wash out wound with lots of saline
- Ensure skeletal stabilisation and if not enough soft tissue coverage ask plastics
- If vascular compromise immediate surgical exploration by vascular

What is the mangled extremity severity score?
Estimates viability of an extremity (usually lower) after trauma to determine need for salvage versus empiric primary amputation
Looks at age, ischaemia, mechanism of injury, shock and doubles score if ischaemia > 6 hours
Score of 6 or less then salvage limb!!
What is the pathophysiology of compartment syndrome?
Causes: high energy trauma, crush injuries, fractures with vascular injury, iatrogenic vascular injury, tight casts/splints, DVTs, post reperfusion swelling
Closed fascial compartments cannot distend so fluid causes increase in intra-compartmental pressure. As pressure increases this compresses the veins increasing their hydrostatic pressure causing more fluid to move out of the veins into the interstitium
Next traversing nerves are compressed causing paraesthesia and possible motor weakness
Lastly when intra-compartmental pressure reachs diastolic bp arterial inflow compromised and ischaemia caused (cool, pale, pulseless, paralysed limb)

How does compartment syndrome present?
- Hours to 48 hours post insult
- Severe pain disproportionate to injury which is not improved with initial measures e.g elevation, analgesia
- Pain made worse by passive stretching
- Paraesthesia distally
- If acute arterial insufficiency then 5 P’s

How is compartment syndrome investigated, diagnosed and managed?
Dx: clinical with high suspicion for post-op
Ix: intracompartmental pressure monitor, CK level
Mx:
- Initial management (see image)
- Urgent fasciotomy with incisions left open for 24-48 hours
- Reassess and debride any dead tissue
- Monitor renal function due to risk of rhabdomyolysis or reperfusion injury

What is ischaemia reperfusion injury?
Reperfusion Syndrome
Paradoxical exacerbation of cellular dysfunction and death, following restoration of blood flow to previously ischaemic tissues
How can a fracture cause compartment syndrome?
- Damage to major vessel
- Oedema
- Inflammation
- Tight plaster cast
Nerve ischaemia can be regenerated but muscle ischaemia causes fibrous replacement and scarring

What are some risk factors for developing septic arthritis?
- Age >80
- Preexisting joint disease e.g RA
- DM or immunosuppression
- Chronic renal failure
- Hip or knee joint prosthesis
- IV Drug use

What are the main causative organisms of septic arthritis and where do they come from?
Most common: S.Aureus, Streptococcus sp, Gonorrhoea, Salmonella (especially in sickle cell)
Can come from bacteraemia (e.g recent cellulitis, UTI, chest infection), direct inoculation, spreading from adjacent osteomyelitis
Causes irreversible articular cartilage damage leading to severe OA

What are some complications of septic arthritis?
- Osteomyelitis (inflammation of bone or bone marrow, usually due to infection)
- Osteoarthritis
- Septic shock

What are the clinical features of septic arthritis and what are some differentials?
- Single swollen joint with severe pain
- Pyrexia
- Joint is red, swollen, warm and painful on examining movements
- Joint often rigid and cannot tolerate passive movement, unable to weight bear

How do you investigate a suspected septic joint?
- Routine bloods inc FBC, CRP, ESR, urate
- Blood cultures
- Joint aspiration before antibiotics (if prosthetic joint do in theatre)
- Plain radiograph of joint
- Radionuclide scans for septic arthritis in isolate joints e.g SI

How is septic arthritis managed?
- After aspirates give flucloxacillin IV for 2 weeks (vancomycin if penicillin allergy) then switch to oral for 4 weeks so 6 weeks total
- Native joint: surgical irrigation and debridement/washout
- Prosthesis: washout and revision surgery

What organisms cause osteomyelitis and where do the bacteria originate from?
Haematogenous spread, direct innoculation (e.g open fracture or penetrating injury), direct spread from nearby infection
Causes: S.Aureus, Streptococci, Enterobacteur Sp, H.Influenzae, P.Aeruginosa (IV drug users), Salmonella (sickle cell)
Check for mycobacterium and fungal causes in immunosuppressed

What is the pathophysiology of osteomyelitis?
When bacteria enters bone it expresses adhesins that bind to host tissue proteins and produce a polysaccharide extracellular matrix. From this the pathogens propagate, spread and seed
If chronic infection can lead to devascularisation of affected bone so necrosis and resorption. Floating piece of dead bone (sequestrum) which is a reservoir for infection as abx cannot penetrate bone
Involcrum can form where the sequestrum becomes incased in a thick sheath of periosteal new bone

What are some risk factors for developing osteomyelitis?
- Diabetes mellitus
- Immunosuppression (e.g AIDS, long term steroids)
- Alcohol excess
- IV drug use

What are the clinical features of osteomyelitis?
- Severe pain in affected region that is constant and often worse at night
- Low grade pyrexia
- Site will be tender and may have overlying swelling and erythema
- Patient may be unable to weight bear
- Try to find potential sources of infection (e.g cellulitis, wounds, sinuses from drug use)

What are some differential diagnoses for osteomyelitis?
- Septic arthritis
- Traumatic injuries
- Primary or secondary bone tumours
- Potts disease (see image)

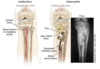
What are some investigations to do if you suspect osteomyelitis?
- Routine bloods (FBC, CRP, ESR)
- Blood cultures
- Plain film radiographs (see image)
- Definitive diagnosis is MRI
- Gold standard is from culture from bone biopsy at debridement

How is osteomyelitis managed?
- >4 weeks antibiotics depending on culture (usually Flucloxacillin or Vancomycin if allergy)
- If evidence of patient deterioration or bone destruction then surgical management with curettage of the area

What are some complications of osteomyelitis?
- Sepsis
- Soft tissue infections
- If in children growth disturbance as can cause premature physeal closure
- Recurrence of infection if stop abx early
- Chronic osteomyelitis

What is chronic osteomyelitis and how is it managed?
- Localised ongoing bone pain
- Non-specific infection symptoms e.g malaise
- May be draining sinus tract
- Often normal inflammatory markers and blood cultures
- Local bone and soft tissue debridement with long term antibiotics. Then a stage reconstruction with prolonged rehabilitation
What are some different bone tumours?
- Divided into primary and secondary
- Divided into benign and malignant
- Most bone tumours are usually metastases

How is metastatic bone cancer managed?
- Most commonly BLTKP spread to spine
- Often palliatively
- Can do prophylactic nailing of long bones at risk of pathological fractures (femur and humerus)

What are some risk factors for developing a primary bone cancer and how do they present?
Risks: genetic association, previous exposure to radiation or alkylating agents in chemotherapy, benign bone conditions e.g Paget’s
Presentation: bone pain that is worse at night and not associated with movement, pathological fracture (no trauma)

What is an osteoid osteoma and how are they managed?
Arise from osteoblasts usually in men aged 10-20 years. Small tumours around the metaphysis of long bones
Localised progressive pain, worse at night, localised swelling/tenderness, limping
Radiolucent nidus with a rim of reactive bone on x-ray
Managed conservatively with imaging every 4-6 months and NSAIDs. If really painful may have surgical resection but most resolve spontaneously

What is an osteochondroma, how does it present and how is it managed?
Benign bony tumours as an outgrowth from the metaphysis of long bones covered with a cartilaginous cap. Usually in men aged 10-120
Often found incidentally as asymptomatic and slow growing but can impinge nerves as they grow
Pedunculated bony outgrowth from meaphysis point away from joint on radiograph
Same management as osteoid osteoma

What is a chondroma, how do they present and how are they managed?
From chondroblasts in the medullary cavity or from the cortical surface. Usually in 20-50 year old long bones of hands, femur and humerus
Usually asymptomatic but can cause pathological fracture
On x-ray well circumscribed oval lucency with intact cortex
If small can just observe. If large or symptomatic removal with curettage and bone grafting as is a small risk of transforming to chondrosarcoma (malignant)

What is a giant cell tumour, how do they present and how are they managed?
Osteoclastomas that come from multinucleated giant cells and stromal cells. Usually in 20-30 year olds in the epiphysis of long bones
Pain, swelling and limitation of joint movement
On x-ray eccentric lytic area (soap bubble appearance)
Surgical resection with potential bone graft

What is an osteosarcoma, how do they present and how are they managed?
Most common malignant bone tumour. Usually 10-14 or >65 years in the metaphysis of the distal femur or proximal tibia
Localised constant pain and tender soft tissue mass
X-ray will show medullary and cortical bone destruction with periosteal reactions (Codman’s triangle/Sunburst pattern)
Tissue biopsy to diagnose then aggressive surgical resection with systemic chemotherapy as known to metastasise to lung

What is Ewing’s sarcoma, how does it present and how is it managed?
Paediatric malignancies, more common in males, affecting the diaphysis of long bones due to poorly differentiated neuroectodermal cells
Enlarging painful mass with tenderness and warmth
X-ray shows lytic lesion with periosteal reaction (onion appearance)
Neoadjuvant chemotherapy and surgical resection

What are chondrosarcomas, how do they present and how are they managed?
Malignant tumours of cartilage usually aged 40-60 and affecting the axial skeleton (pelvis, shoulder, ribs)
Painful and enlarging mass.
X-ray shows lytic lesions with calcification, cortical remodelling and endosteal scalloping
Intralesional curettage

How are bone tumours investigated and how can you tell the difference between benign and malignant lesions on radiograph?
- Plain film radiographs
- MRI to look at soft tissue involvement
- CT to look at cortical involvement
- Bone biopsy for definitive diagnosis

What are some important history questions to ask in a surgical history that differ to a normal history?
- Any steroids or immunosuppressants?
- Any anticoagulants or COCP?
- Any drug allergies?
- Drink or smoke?
- Previous operations and anaesthesia?
ALWAYS ASK ICE

At the end of an OSCE station what are some additional investigations you should offer to do?
- Bedside tests (e.g urinalysis and obs)
- Bloods
- Imaging
- Special tests (e.g aspirate)
If MSK exam offer to look at joint above and below and full neurovascular exam
What is the difference between primary and secondary bone healing?
Primary (Direct Healing - faster)
- Stable anatomical reduction so no gap in bone (usually surgical reduction)
- Healing requires only remodeling of lamellar bone, the Haversian canals and the blood vessels without callus formation. Uses cutting cone
Secondary (Indirect Healing - more common)
- Endochondral ossification
- Haematoma, granulation tissue, soft callus, hard callus, remodelling

How do you describe an x-ray of a fracture?
- State patients name, DOB and date x-ray taken
- Describe view of x-ray and what we’re looking at
- Describe obvious deformity location (e.g metaphysis, diaphysis, epiphysis) fracture type (e.g transverse, oblique), fracture position (e.g shortened, displaces, rotated), simple vs complex

What is the best way to check the motor function of the upper limb muscles?
Rock, Paper, Scissors, Ok



