17. Inflammatory Bowel Disease Flashcards
What is inflammatory bowel disease an umbrella term for?
What are some associated complaints/diseases?
What are the defining features of IBD?
What is IBS?
Ulcerative colitis, Crohn’s disease, IBDU/CUTE/indeterminate colitis
Arthritis, pyoderma gangrenosum, primary sclerosing cholangitis (progressive cholestasis with bile duct inflammation and strictures), non-thyroidal illness syndrome (NTIS)
Chronic, idiopathic, relapsing and remitting. Inflammatory disorders of the GI tract
Syndrome defined by symptoms - varying abdo pain, diarrhoea + constipation, sometimes due to stress, no actual pathology
Compare the prevalence, incidence, female:male ratio and age of presentation in UC and CD.
List some environmental factors that could contribute to IBD development.
How does smoking play a part in UC and CD?
What kind of diet is effective in making CD better? What are the likely dietary components that might contribute to CD?
[Pic]
Childhood hygeine, smoking (Crohn’s) or not smoking (UC), drugs (NSAIDs), dietary factors, depression, stress, gut microflora
UC: Non-smokers more common, onset of UC commonly follows smoking cessation
CD: Smokers more common, accelerates disease progression, less likely to respond to tx, smoking cessation effective tx
Elemental/polymeric liquid diet.
Likely suspects: high animal fat diet, low fibre, emulsifiers and thickeners, may alter gut microbiome

How might the stress response affect gut immune cells (psychoneuroimmunology)?
Is IBD a genetic disorder?
What 3 things make up the pathogenesis of IBD?
How many bacteria are there in the colon?
[Pic]
It’s a complex polygenetic disorder (>160 candidate genes) with familial aggregation (10%) in UC and CD. NOD2 is the most strongly linked mutation with IBD (terminal ileal disease in CD, but only 20% of pts with CD carry it). CARD15 mutation also found in CD
Environment, gut bacteria, host genetics
1013-14, lots of diff spp

How is the gut flora different in pts with IBD?
Describe the immunology component of IBD.
Where does UC most commonly effect?
They have different and less diverse faecal bacteria.
IBD is a multifactorial disease that is nonetheless driven in part by an exaggerated immune response to gut microbiota that causes defects in epithelial barrier function. See bacterial dysbiosis, barrier function defective, aberrant neutrophil migration, excess TNFa and other pro-inflammatory cytokines, T-cell dysregulation
Colon and rectum only, almost always rectum with variable proximal extent. Continuous inflammation limited to lamina propria. [Pic]

Where does CD most commonly effect?
Which histopathology is UC and CD? Explain why and what the arrows are indicating.
What are some presenting features of IBD?

Any part of GIT from mouth to anus. Segemental transmural inflammation. Strictures, fistulas, abscess formation. Most common areas = terminal ileum and caecum. 40% ileal, 30% colonic, 30% ileocolonic [Pic]
1) UC: superficial, diffuse inflammation, architectural distortion, cryptitis, crypt absecces (UC feature). Arrow = inflammatory cells in crypt = crypt abcesses
2) CD: deep, patchy inflammation, non-caseating granulomas, giant cells (arrow)
Diarrhoea (often bloody), abdo pain, wt loss, malaise, fatigue, relapses and remissions, onset any age, life-long
Distinguish between mucus and pus.
Compare UC and CD with the following:
a) rectal bleeding
b) mucus/pus PR
c) abdo pain
d) wt loss
e) abdo mass/abscess
f) upper GI tract
g) obstruction/strictures
h) fistulas
i) perianal disease
j) colorectal cancer
k) extra-intestinal features
Mucus: clear viscous high protein secreted by goblet cells in nasal mucosae/intestine
Pus: dying/dead white cells and bacteria, looks white/yellow/green
[Table]
UC don’t tend to get progressively worse unlike Crohn’s

By how much does having IBD increase the risk of colorectal cancer? What features of the disease make it more likely?
What are the 2 categories of extra-intestinal features of IBD (6-50% pts)?
How might IBD affect the skin?
1-4x risk.
Duration of disease >10yrs, extensive colitis, chronic inflammation, sclerosing cholangitis. Colonoscopic screening for macro/microscopic dysplasia starts after 8 years
- *Manifestations** (skin, eyes, joints, liver)
- *Complications** (anaemia, thrombosis, urinary stones, gallstones, osteoporosis)
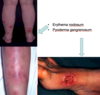
Erythema nodosum (5-10% with acute IBD, swollen fat under the skin causing red bumps and patches), pyoderma gangrenosum (<5% - skin condition causing painful ulcers). [Pic]
How might IBD affect the eyes, joints and liver?
Anaemia is a common complication in IBD (40%). What are the types, and why do they occur?
Eyes: episcleritis (benign, self-limiting inflammatory disease affecting episclera), uveitis (uvea inflammation - visible pus cells in anterior chamber of eye)
Joints: sacroilitis and anklyosing spondylitis, large joint arthropathy, small joint arthropathy
Liver: primary sclerosing cholangitis (bile duct inflammation - itching, jaundice, risk of cancer of bile duct and colon), fatty liver, autoimmune hepatitis. [Pic]
1. Fe deficiency (due to bleeding, malabsorption (mainly absorbed in proximal small bowel), increased amount of hepsidin produced, and lack of appetite)
2. Anaemia of chronic disease
3. B12 and folate deficiency (Crohn’s) (B12 due to disease in terminal ileum where it’s normally absorbed. Folate due to increase in folate turnover)

Why does Crohn’s have a higher mortality than UC?
List some differential diagnoses of IBD.
What investigations would you do to diagnose and assess disease activity in IBS?
What management would a Truelove and Witt’s score of mild, moderate and severe indicate for UC severity?
Partly because of smoking.
Infective colitis (C. diff, salmonella, shigella, camphylobacter, giardia, amoebiasis), IBS, coeliac disease, colorectal cancer, ischaemic colitis, NSAID colitis
Symptoms and signs, blood (CRP, Hb, plts, albumin), stool (microbiology/C diff toxin, fecal calprotectin (1st line before colonoscopy, white cell protein, elevation indicates migration of neutrophils to intestinal mucosa), ileocolonoscopy, AXR/CT/barium follow-through/MRI, capsule endoscopy
Mild: 5-ASA (anti-inflammatory)(OP), Moderate: oral steroids (OP and IP), Severe: IV steroids (IP) [Pic]

What can you see in the plain AXR below?

Toxic megacolon - acute colonic distension, active inflammation, perforation danger (50% mortality)
Which colonoscopy images show UC and CD?
Describe the two stages of IBD tx principles: induction and maintenance of remission.

1 = UC; 2 = severe UC; 3 = CD
Induction: 5-ASA (UC), corticosteroids (SE: delays wound healing, acne, infections, growth retardation, blurred vision, diabetes, HTN, osteoporosis, cateracts/galucoma, cushingoid appearance etc.), ciclosporine (UC), liquid formula diet (CD), anti-TNFa, vedolizumab (anti-integrin), surgery
Maintain remission: 5-ASA (UC), thiopurines, methotrexate, anti-TNFa, vedolizumab
Does the barium follow through and MRI with enhancement show UC or CD?
Why is CT avoided?
When might wireless capsule endoscopy be used?

CD - terminal ileum and caecum inflamed
Cumulative radiation exposure!
Occasionally used to look for CD in pts with equivocal standard imaging


