11. Upper GI Pathology Flashcards
What is Barrett’s oesophagus?
What are the arrows indicating in the oesophageal images?
What is the connection between Barrett’s oesophagus and oesophageal carcinoma?

Metaplasia of oesophageal stratified squamous epithelium -> gastric type columnar epithelium, due to prolonged gastro-oesophageal reflux. Any age, M>F. Can be: classical = ≥3cm, short segment = <3cm, ultra short = <1cm
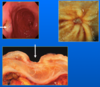
L: top = Barrett’s glandular epithelium; bottom = normal stratified squamous epithelium
R: top = normal stratified squamous epithelium; bottom = Barrett’s glandular epithelium. Intestinal metaplasia within oesophageal glandular mucosa
30x increased risk of developing epithelial dysplasia and adenocarcinoma. Risk persists even after successful treatment of the reflux
What are the arrows pointing to in the oesophageal image?
What is the epidemiology of oesophageal carcinoma?
What are some predisposing factors?
What are some presenting features?

Top: normal squamous mucosa. Bottom: large polypoid leision (carcinoma, extending through full thickness of oesophageal wall)
High and low incidence areas, M:F = 3-4:1, age >50
Diet (decreased vit A & C), oesophageal disorders (e.g. Barrett’s oesophagus), genetic/racial, smoking, alcohol, obesity, nitrosamine exposure, other conditions e.g. Plummer-Vinson syndrome
Progressive dysphagia, anorexia, weight loss, aspiration pneumonia, fistula formation. Retrosternal chest pain
What are the % chances of carcinoma occuring in the upper, middle and lower thirds of the oesophagus?
Describe the macroscopic appearance of an oesophageal carcinoma.
What are the most common microscopic appearances of oesophageal carcinoma?
What are 2 methods of oesophageal carcinoma spread?
Upper = 20%, middle = 50%, lower = 30%
Upper + middle almost exclusively squamous cell carcinoma; lower = adenocarcinoma most common
Polypoid fungating, ulcerating (pic - ulcerating mass, may present with haematemesis), annular constricting, diffuse infiltrating
Squamous cell carcinoma = 85%; adenocarcinoma = 10%; undifferentiated carcinoma = 5%
Direct or via lymphatics
(The site determines LNs e.g. upper 1/3 = cervical, middle 1/3 = mediastinal, lower 1/3 = perigastric and coeliac)

Where does adenocarcinoma usually arise, at what age, and what is the M:F ratio like?
Describe what each of the histologies below show, and what the arrows are indicating.
How is oesophageal cancer investigated and treated?
What is the prognosis for oesophageal carcinoma?

Foci of Barrett’s metaplasia. Usually elderly. M:F = 5:1
Left: squamous cell carcinoma; arrow = infiltrating islands of squamous cells
Right: adenocarcinoma; top arrow = normal glandular epithelium, small nuclei; bottom arrow = nuclei larger, haphazard, irregular shaped gland. Moderately differentiated adenocarcinoma
Ix: oesophagoscopy + biopsy +/- EUS, CT/MRI for staging, or laparoscopy if significant intra-diaphragmatic component
Tx: If localised T1/T2 = radical curative oesophagectomy. If surgery not an option then chemoradiotherapy may be better than just radiotherapy
5 year survival = 5-10%
70% dead within 1 year due to late presentation
What is chronic gastritis?
What are some signs/symptoms?
What is being indicated in the histopathology of gastritis below?

Chronic inflammation of gastric mucosa. Common. [Pic: crypt in stomach - black dots = H.pylori on surface]
Often asymptomatic, or epigastric pain related to hunger/specific foods/time of day +/- bloating, dyspepsia, tender epigastrium. _ALARM S_ymptoms = _a_naemia, _l_oss of weight, _a_norexia, _r_ecent onset/progressive symptoms, _m_elaena/haematemesis, _s_wallowing difficulty
Chronic inflammation - lymphocytes and plasma cells. Can see neutrophils in superficial epithelium above

What is the aetiology of chronic gastritis?
What is the arrow in the image indicating?
List the possible outcomes of H.pylori infection.
How is possible chronic gastritis due to H.pylori treated?
- Bacterial infection:** 85-90% (H.pylori*).
- *Chemical injury:** NSAIDs, bile reflux, alcohol(?); Autoimmune: anti-parietal cell antibodies
H. pylori - slightly curved spirochetes
Peptic ulceration (5-15%); gastric carcinoma (1-3%); primary gastric lymphoma (0.5%), asmyptomatic (>80%)
If ≤55yrs test for H.pylori; treat if +ve: first line triple therapy = PPI (omeprazole) and 2 antibiotics (clarithromycin and amoxicillin).
If ≥55 (and new dyspepsia not from NSAID use and persisting for >4-6wks) or ALARM Symptoms, refer for urgent endoscopy
What causes peptic ulcers? Where are the most common sites?
What is the epidemiology of peptic ulcers? (Lifetime risk of development, M:F, worldwide incidence)
What are some predisposing factors for peptic ulcers?
Action of ‘peptic’ juices on gastrointestinal mucosa. Can be chronic (pain at night, 1-3hrs after food, if untreated takes ~15yrs to kill) or acute (stress ulceration e.g. radiation, NSAIDs). Most common sites = oesophagus, stomach, duodenum, Meckel’s diverticulum (in small bowel, if it contains gastric mucosa)
Lifetime risk: 10% men, 4% women. M:F for duodenal U = 3:1; gastric U = 1.5-2:1.
DU decreasing worldwide (better dx/tx) but commoner than GU; GU static
H.pylori gastritis, Zollinger Ellison syndrome (gastrinoma, autoimmune, stomach produces too much acid), other (NSAIDs, heredity, blood group O, alcohol)
What is the pathogenesis of peptic ulcers?
Describe the macroscopic appearance of peptic ulcers.
What are some complications of peptic ulcers?
Imbalance between damaging forces (increased acid/pepsin, bile salts, H.pylori, impaired regulation of acid/pepsin secretion, NSAIDs, alcohol, tobacco) and mucosal protective mechanisms (mucin secretion, cellullar mucus, bicarb secretion, mucosal blood flow, cell turnover, prostaglandin synthesis, apical membrane transport)
80% single, 75% <3cm diameter, punched out edges, often deeply penetrating, fibrosis at base [Pics: top L = well defined deep peptic ulcer; top R = PU; bottom = cross section of PU, white vertical lines = stellate - scarring - fibrosis at base]
Haemorrhage. Obstruction (if pyloric or pre-pyloric) from oedema and scarring. Perforation -> peritonitis
What is the geographical distribution of gastric carcinoma like?
List some presenting features of gastric carcinoma [pic].
What are some predisposing factors for gastric carcinoma?

High (Japan, China, Portugal, Russia…) and low incidence areas
Dyspepsia, weight loss, anorexia, abdominal pain, vomiting, haemorrhage (if tumour errodes into BV), anaemia, metastatic disease. Signs suggesting incurable disease: jaundice, ascites, hepatomegaly, epigastric mass, large Virchow’s node, acanthosis. Tend to go to perigastric and coeliac LN, and first organ travelled to tends to be liver
H.pylori gastritis, genetic factors, environmental factors e.g. diet
Briefly describe the stages in development of gastric carcinoma.
What are the most common sites of gastric carcinoma?
Describe the macroscopic appearance of GC.
Describe what you see/the arrows in each of the images.

Normal gastric mucosa -> (H.pyori converts it to:) -> chronic gastritis -> intestinal metaplasia -> dysplasia -> carcinoma
Antrum 50%, Body 25%, GOJ 25% (but changing)
Polypoid fungating, polypoid with ulceration, ulcerating, diffuse infiltrating (linitis plastica) [Pic]
Top L: large polypoid mass. R: polypoid mass with ulceration. Bottom L: diffuse infiltrating tumour, effacing the submucosa

What are the 2 possible microscopic features of a gastric carcinoma?
What is an early gastric carcinoma?
What are the routes of spread for a gastric carcinoma?
What is the prognosis like for advanced/early GC?
- Adenocarcinoma (95%)** - divided into 2 main types: intestinal (from intestinal metaplasia), or diffuse (signet ring*)
- *Undifferentiated carcinoma (5%)**
Tumour confined to mucosa/submucosa. Frequency depends on efforts made to find it
Direct, lymphatic, haematogenous, transcoelomic (e.g. to ovaries - Krukenberg tumour)
Advanced: 5-15% 5 year survival. Early: >90% 5 year survival
What is shown in each of the histologies?

L: intestinal type adenocarcinoma. Some regular, some mishapen
R: diffuse adenocarcinoma. Signet rings, intra-cytoplasmic vacuoles contain mucin, push nuclei to side. Poor prognosis and present quite late
Compare intestinal-type adenocarcinoma and diffuse adenocarcinoma.
(% of gastric adenocarcinoma, origin, geographical distribution?, presentation)
Intestinal: 55% of gastric adenocarcinoma, originates from foci of intestinal metaplasia, incidence mirrors geographical distribution, presents as polypoid/ulcerating mass
Diffuse: 30% of gastric adenocarcinoma, originates from mucous neck cells in gastric pits, no significant geographical distribution, presents as linitis plastica, spreads widely through gastric wall with single cell infiltration



