Week 4- Bladder Obstruction Flashcards
(53 cards)
What is the innervation of the kidneys, ureters, bladder and urethra?
Kidney:
- T10-L1 (SNS)
- vagus (PNS)
- Only SNS feels pain?
Ureter
- T11-L2 (SNS)
- S2,3,4 (PNS)
- Both can feel pain
Bladder
- Same as ureter, BUT PNS has the pain fibers
Urethra
- L1,2 (SNS)
- S2,3,4 (PNS)
Trace the path of a sympathetic neuron going to the bladder. What does it innervate?
Pre-ganglionic neuron comes out of the spinal cord at T11-L2, goes through the white rami communicans an to a pre-aortic ganglion. Then intermesenteric plexus, then superrior hypogastric plexus, which bifurcates. And then goes to innervate the:
- detrusor (B-adrenergic= relax)
- internal sphincter (alpha-adrenergic= contract)
- seminal vesicles (ejaculate)
Trace the path of a parasympathetic neurons going to the bladder. What does it innervate?
Preganglionic comes out of S2,3,4, synapses in the hypogastric plexus. Innervates:
- detrusor (msucarinic ACh= contract)
- internal spincter (=relax)
- penis (erection)
Trace the path of a sympathetic nerve going to the kidney
The pre-ganglionic nerve comes out of T10-L1, goes through the white ramus communicans, then synapses in the renal ganglion and continues on to the kidney.
Trace the path of a parasympathetic nerve going to the kidney
The vagus nerve (cranial nerve X) goes there….
What is LUTS?
Lower Urinary Tract Symptoms. A constellation of symptoms from either obstructive or irritative voiding disturbances.
- Urinary frequency
- Nocturia
- Urgency, with or without incontinence
- Hesitancy in initiating the stream
- Weak stream
- Dysuria
- Sense of incomplete bladder emptying
- Post void or terminal dribbling
What the the differential for LUTS?
Huge!

What to ask your patient with LUTS?

What are irritative vs. obstructive voiding dysfunction symptoms?

Are dysuria, microhematuria and incontinence normally seen in BPH?
Not in uncomplicated cases
What is IPSS?
International prostate symptom score
What would you always do with a man with prostate enlargement? What would you sometimes do?
Always:
- IPSS
- Urinanalysis
Sometimes:
- PSA
- Serum creatinine (if suspected hydronephrosis)
- cytology (if predominantly irritative symptoms)
- urodynamic studies (e.g. post-void residual volume)
What are BOO, BPE and BPH?
BOO: bladder outlet obstruction (a clinical term)
BPE: benign prostate enlargement (a clinical term)
BPH: benign prostate hyperplasia (a histological diagnosis)
Does BPH progress? What are predictors of progression?
Yes- in some patients- the prostate continues to enlarge. Age, prostate volume and PSA levels are all negative. Symptoms can worsen, or acute urine retention
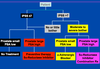
What is the treatment algorithm for BPH? (see other slides for the rationale of each treatment)
What are lifestyle measures for treating BPH?
“sleep apnea” means treating sleep apnea because it can cause nocturia.

Are the alpha-adrenergic blockers used for BPH selective or non-selective for urinary tissue? What are side-effects
They are selective. Older drugs were not selective.
Tamulosin (Flowmax) can produce retrograde ejaculation (not a problem except for fertility), but not erectile dysfunction
Is viagra (PDE5i’s) safe with non-selective alpha blockers? Selective alpha blockers?
Can result in hypotension with non-selective , but is safe with selective alpha blockers
How is cell growth promoted in the prostate? (e.g. what hormone, and how is this targeted)
Testosterone: converted to its more powerful self, DHT intracellularly by either Type 1 or Type 2 5-alpha-reductase. Type 2 is found only in the prostae, type 1 is found in the skin, liver, bladder.
Can block Type 2 (finasteride)
What are the important side effects of type 2 5-alpha reductase inhibitors?
What is the great thing about them?
Sexual side effects (ED….)
They reduce the risk of prostate cancer by 25%
How to treat: low IPSS, large prostate and PSA?
With a 5ARi alone. Don’t need in combination with an alpha-blocker because the alpha-blocker deals mostly with the symptoms
How to treat: low IPSS, small prostate and low PSA.
No treatment.
How to treat: high IPSS, bother, small prostate, low PSA
An alpha blocker to treat symptoms. They won’t benefit from shrinking the prostate
How to treat: high IPSS, bother, large prostate, high PSA level
WIth combination therapy. 5ARi shrinks the prostate, and the 5 alpha blocker helps with symptoms




