Week 3 - respiratory system Flashcards
(78 cards)
Anatomically, how is the respiratory system divided?
-
Upper respiratory tract, consisting of:
- Nostrils
- Nasal cavity
- Pharynx
- Epiglottis
- Larynx
-
Lower respiratory tract, consisting of:
- Trachea
- Bronchi
- Bronchioles
- Lungs

Where does air enter the respiratory system?
Outline the structure
- Air enters the respiratory system through the nostrils
- Nostrils are divided by the nasal septum cartilage

Describe the entrance of the nasal cavity
- The surface wall consists of:
- Stratified epithelial cells
- Sebaceous glands
- Nose hairs
- The above serve to filter out inhaled particles

Describe the nasal passage
- The walls of the nasal passage are lined with respiratory mucosa
- Respiratory mucosa is covered by pseudostratified ciliated columnar epithelium which is interspersed with goblet cells
- Cilia cover the surface of epithelial cells which have rythmic movement (mocucillary action)
- Goblet cells and mucosal glands are responsible for secreting mucous

What is the function of mucous in the respiratory system?
- Mucous traps inhaled particles and the mucocillary action moves the airborne contaminants towards the pharynx (throat)

How is the inahled air warmed by the nasal cavity?
- Inspired (inahaled) air is warmed and conditioned by a network of thin walled veins that are located under the nasal epithelium
- There are several blood vessels in this area which causes the transfer of heat to the colder inspired air
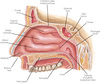
What are conchae?`
- Conchae, aka turbinate, are present in the nasal cavity
- Conchae are lined with mucosa which increases the surface area over which inspired air passes through in the nasal cavity
- The inspired air is warmed and humidified as it passes over the conchae

What else is present in the mucosa of the nasal cavity?
- Nerve endings are located in the nasal mucosa which detect smell (olfactory nerve), pressure, temperature and pain
What are paranasal sinuses?
- Paranasal sinuses are located close to the nose inside the frontal, maxillary, sphenoidal and ethmoid bones
- The paranasal sinuses are lined with a mucous membrane that drains into the nasal cavities which assist in the production of mucous from the respiratory tract
Besides the paranasal sinuses, what else drains into the respiratory tract?
- The lacramal sacs also drain into the nasal cavity
- They are responsible for collecting tears from each eyelid and drain them into the nasal cavity

What is sneezing?
- Sneezing generally occurs when an irritant passes through the nasal hairs to reach the nasal mucosa
- This triggers the release of a histamine which irritates the nerve cells in those
- This results in an electrical impulse being sent to the brain which initiates the sneeze reflex
- The brain also simulates the pharyngeal, tracheal and chest muscle to expel a large volume of air from the lungs through the nose and mouth
- Sneezing can also be triggered by allergies and sinus infection
Give some examples of sino-nasal pathologies
-
Turbinate / mucosa hypertrophy:
- terbinate hypertrophy (enlargement) may arise due to inflammation or abnormal developement which results in an increase in volume of the turbinate mucosa
-
Deviated septum:
- Occurs when the septum has drastically deviated from the midline between the nostrils
-
Nasal polyps:
- Abnormal nonconcerous growth of tissues projecting from the mucous membrane in the nasal sinus
What is the pharynx and what can it be divided into?
- The pharynx (throat) is a tube-like structure that connects the posterior oral and nasal cavities to the larynx and oesophagus
- Divided into three anatomical portions according to location:
- Nasopharynx: posterior to the nasal chambers and located between the internal nares and the soft plate
- Oropharynx: posterior to the mouth
- Laryngopharynx: posterior to the pharynx

Describe the nasopharynx
- At the walls of the nasopharynx are the left and the right Eustachian (auditory) tubes connected to the middle ear
- The lining of the Eustachian tubes is continuous with the lining of the nasopharynx
- The connection between the nasopharynx and the middle ear permits the equilisation of air pressure between the middle ear and the exterior ear
- Tonsils are located in the pharynx and pharygneal tonsils are situated in the nasopharynx

What is the purpose of the pharynx?
- Serves as a passageway for both the digestive system and the respiratory system because food and air travels through it
- Air enters the pharynx from the two nasal cavities and food enters from the mouth
How is food and air directed through the pharynx?
Describe this structure
- The epiglottis controls the direction of food from the pharynx down the oesophagus and the direction of air down the trachea
- The epiglottis is a flap of elastic cartilage that acts as a lid which covers the trachea when food is swallowed to prevent it from entering the larynx
- During swallowing breathing is momentarily stopped because the soft palate and its uvula point upwards so that neither food nor air can pass through it
What is the nasopharynx lined by?
- The surface of the nasopharynx is covered by pseudo-stratified columnar epithelium
- They also have a simular mechanism of mucous secretion from goblet cells in the epithelium to warm, humidify and filter the inahled air
What is the orthopharynx and the laryngopharynx lined with?
- The surface is lined with non-keratinising stratified squamous epithelium which is required as it is exposed to the passage of food unlike the nasopharynx
Describe some pathologies of the pharynx
- Pharyngeal cancer: can arises in the squamous epithelial cells of the pharynx which can restrict the airway and alter the natural flow of air in the pharynx
- Pharyngitis: the inflammation of the pharynx can be acute or chronic with different causes.
- Can cause swelling of the oropharynx and elnarged tonsils restricting the passageway for breathing and swallowing
- Tonsillitis: inflammation of the tonsils can be caused by bacteria or viral infection
- Tonsils become enlarged and this restricts the opening of the airways from the oral cavity to the oropharynx causing breathing and swallowing difficulties

Describe the larynx
- The larynx is commonly referred to as the voice box and is situated below the pharynx
- It is composed of several cartilages (thryoid, cricoid, epiglottis, arytenoid, corniculate and cuneiform) connected by ligaments and membranes
- The larynx houses the vocal folds that are responsible for phonation (sound production)
- The space between the vocal cords is the glottis

Besides phonation, what else is the larynx responsible for?
- The larynx serves as a sphincter in transmitting the inspired air from the oropharynx to the trachea (and also increating sound for speach)
How is the larynx responsible for phonation?
- The expired air released from the lungs passes through the glottis and the vocal cords induces phonation at the larynx
- Similar to guitar strings, vocal cords in the larynx produce a vibrating sound and the final sound depends on the pharynx, nose, mouth, tongue and lips
What is the larynx lined with?
- The larynx is lined with a ciliated mucous that further contributes to the removal of particulates and to warm and humidify the air
Describe the larynx during swallowing
- Food is prevented from entering the larynx during swallowing becuase the back of the tongue that is attached to the top of the larynx pushes upwards, forcing the epinglottis to cover the glottis
- If food items do enter the larynx and come into contact with the vocal cords, the larynx muscles become stimulated and induce a cough reflex in attempt to expel the items to prevent choking






















