Week 2 - The cardiovascular system Flashcards
(62 cards)
What is the cardiovascular system commonly referred to as and what does it do?
- Commonly referred to as the fluid transport system
- Delivers substances to the tissues of the body while removing waste products of metabolism
- Ensures that each cell is replenished with nutrients, water and oxygen
- Transports substances, such as hormones, from their site of production to their target organs
Where is the heart positioned in the body?
How many chambers does the heart have?
- To the left of the thoracic cavity between the lungs
- The heart has four chambers
What are the similarities and differences between cardiac muscle and skeletal muscle?
- The heart has it’s own conduction system in contrast to skeletal muscle which needs nervous stimuli
- Composed of specialised cardiac muscle cells which have their own electrical conductance abilities similar to nerves
What are the different layers of the heart?
- Outer pericardium - thick membrane sack that surrounds the heart and protects and lubricates the heart by reducing friction
- Visceral pericardium / epicardium - the inner layer of pericardium, consists of connective tissue
- Myocardium - thick and composed of specialsed cardiac muscle cells that have electrical conductance abilitities
- Coronary arteries supply the myocardium
- Endocardium - thin layer of smooth muscle consisting of epithelium and connective tissue + elastic & collagenous fibres
- Inner layer of the heart wall
- Purkinje fibres are specialised cardiac muscle fibres foudn here

Describe the chambers of the heart and what they are divided by
- Four chambers in the heart (2 left & 2 right)
- Upper chambers are the atria divided by interatrial septum (a wall-like structure)
- Lower chambers are the ventricles divided by interventricular septum

How is the heart able to act like a pump?
- Two sides of the heart function as two seperate pumps & pump blood through seperate circulations
- Right side pumps deoxygenated blood in the pulmonary system
- Left side pumps oxygenated blood in the systemic circulation
- Since the right and left ventricle & atrium is seperated from the right, oxygenated and deoxygenated blood doesn’t mix

What are the atria referred to as?
Where do they recieve blood from?
- Referred to as receiving chambers because the recieve blood returning to the heart (have smaller and thinner walls than ventricles)
- Right atrium receives deoxygenated blood from the superious vena cava and the inferior vena cava
- Superiour vena cava carries blood from head, neck, chest & arms
- Inferior vena cava carries blood from trunk & legs
- Left atrium receives oxygenated blood from the left &right pulmonary veins
What are the ventricles referred to as and where to the pump blood to?
- Referred to as discharding chambers as they receive blood from the atria and pump out into the pulmonary artery and aorta

Describe the flow of blood through the heart
- Blood from the superious / inferior vena cava enter the right atrium
- Right atria contracts and and blood flows across the tricuspid valve into the right ventricle
- Right ventricle contacts, tricuspid valve closes and blood flows across the semilunar valve into the pulmonary artery
- Pulmonary artery splits into two vessles & enters the capillaries of the alveoli in the lungs
- Blood returns to left atrium through the 4 pulmonary veins
- Left atrium contracts and blood goes across the bicuspid (mitral) valves into the left ventricle
- Left ventricle contracts, mitral valve closes forcing blood into the aorta across the semilunar valve
How many atrioventricular valves are there?
What is the function of the atrioventricular valves?
- There are two atrioventricular valves (AV) seperating the atria from the ventricles
- They are one way valves to ensure that blood only flows in one direction from the atria to the ventricles

What are the left / right AV valves known as and what is their structure?
- Right AV valve is known as the tricuspid valve because it has three flaps and is located between the right atrium and the right ventricle
- Left AV valve is called the bicuspid (mitral) valve as it has two flaps and separates the left atrium from the left ventricle

How & where are the AV valves attached?
- The AV valves are attached to the walls of the ventricles by string-like structures known as chordae tendinae
What are the valves positioned between the ventricles and the arteries known as?
- The semilunar valves are positioned between the centricels and large arteries (pulmonary atery and aorta) that carry blood away from the heart

What happens to the deoxygenated blood pumped from the heart?
- Blood leaves the right side of the heart and enters the pulmonary trunk
- From the pulmonary trunk to the pulmonary artery
- Enters the capillaries of the alveoli of the lungs where gas exchange occurs
What happens to blood from the left side of the heart?
- Blood is pumped across the aortic semilunar valve into the ascending aorta
- Aorta branches into ateries carrying oxygenated blood to all parts of the body
- First 2 aortic branches are the coronary arteries (supply oxygen. blood to the capillaries of the myocardium)
Structurally, what is the difference between the left and right side of the heart?
- Left ventricular musclar wall is very thick since it needs to force blood to all body parts meaning a high resistance to blood flow
- Right ventricular muscular wall is thinner as it only pumps blood to the lungs with a lower resistance to blood flow
How are the four chambers of the heart coordinated?
- Atria contract first (atrial systole) whilst the ventricles contract (ventricular diastole)
- Once ventricles are filled with blood the ventricles contract (ventricular systole) and the atria relax (atrial diastole)
- A brief period of relaxation for both the atria and the ventricles occurs
- The above series of events make up the cardiac cycle
What is the distinctive sound of the cardiac cycle called and why does the sound arise?
- Distinctive double thumping sound (lub dup) when heard through a stethoscope
- Lub is caused by the vibration and sudden closure of the AV valves during ventricular systole
- Dup is caused by the closure of the SL valves during ventricular diastole
What are the two pacemakers of the heart?
How are they regulated?
- The sinoatrial node and the atrioventricalar node are the two cardiac pacemakers causing the heart to beat
- They can be regulated by the automonic nervous system and circulating adrenalin

Describe the structure and function of the SA node
- SA node is a small mass of specialised cells located beneath the epicardium of the right atrium
- SA node is impulse generating tissue which initiates impulses throughout the myocardium, stimulating the contraction of cardiac muscle fibres
- Referred to as the pacemaker as it generates the hearts rhythmic contractions

Describe the path of the cardiac impulse
- Cardiac impulse starts as the SA node
- Travels into the atrial syncytium which causes the atria to contract
- Impulse travels along junctional fibres to the AV node
- Due to the smaller diamter of the junctional fibres, the impulses are slightly delayed
- Once impulse reaches AV node it passes into the bundle of His and Purkinje fibres to the ventricles causing them to contract

What is the significance of the smaller diameter of the junction fibres before the AV node?
- The impulses are slightly delayed
- Allows the atria more time to contract and pass their blood to the ventricles before ventricular contraction occurs
- Under normal circumstances ventricular beat follows each atrial beat

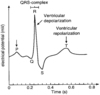
What is and electrocardiogram and what does it represent?
- An electrocardiogram (E. C. G.) is the graphic record that represents the electrophysiology of the heart
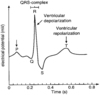
What can an E. C. G. show?
- ECG can show the heart’s rate and rhythm and it can also detect abnormalities such as enlargement of the heart