Valvular Heart Disease & Tumors Flashcards
What valve is shown in the provided image?
What are important characteristic of this valve?

- Aortic Valve (Pulmonic looks exactly the same)
- 3 cup-shaped cusps
- thin, delicate, pliable
- plop open & are flexible
- no nodularity
- When they close, they are very tightly opposed, so there is no leakage around them
What is the the valve shown in the provided image?
What are its important characteristics?

- 2 Leaflets (not cusps)
- thin, delicate, pliable
- attached by chordae tendinae to the papillary muscles
- When leaflets close, they prevent back leakage (regurgitation) from ventricle to atrium
- Tricuspid is the same, but with 3 leaflets
What is Rheumatic Fever and how do you get it?
What should you be looking for in the history?
-
Immune-mediate inflammatory disease that occur few weeks after group A beta streprococcal pharyngitis (ie. strep pyogenes)
- Streprococcal M proteins that cross react with self-antigens in the heart, causing damage to the endocardium, myocardium, & pericardium
- Sterile condition, there are no organisms left (cultures will be negative, but can draw blood for antibodies)
- Episode Rheumatic Fever will predispose that person to recurrent Rheumatic Fever is they are infected again
- May not be aware they had strep throat, but maybe had just been tired, may not have had a serious sore throat, in other cases they will feel really terrible (headache, very sore throat, etc.)
- Major problem before widespread antibiotic therapy
What are the components of the Jones Criteria?
What are the major criteria for diagnosing Rheumatic Fever?
Minor criteria?
** will not be tested
- Jones Criteria: Evidence of a preceding group A streptococcal infection (culture, immunoassay, or positive serologic tests) and two major criteria or one major and two minor criteria
-
Major Criteria
- Carditis
- Polyarthritis (reactive arthritis)
- Chorea (rapid, jerky movements of the body)
- Erthema marginatum (upper arms, legs, & trunk)
- subcutaneous nodules (uncommonly seen)
-
Minor Criteria
- Fever
- arthralgia
- Previous ARF/RHD
- Increased acute-phase reactants
- Prolonged PR interval
What pathology is shown in the provided image?

Acute Rheumatic Fever: “Bread and Butter” Pericarditis
Gross: If you spread a lot of butter on a couple slices of bread & then stick them together and pull them apart, you get this kind of shaggy appearance & yellow color
Microscopic: lower left is myocardium, the middle where its a little lighter in color is the pericardium. May have a few scattered inflammatory cells (typically no neutrophils - nonsupperative). On the pericardium, you see what cause the shaggy, butter appearance, extensive fibrin deposition
What pathology is shown in the provided image?
Acute Rheumatic Fever: Inflammatory Mitral Valvulitis
Sterile condition, do not have organisms in them
- Little vegetations- verugae (different from infectious endocarditis) due to inflammation of the endocardium.
- Fibrinoid necrosis of the leaflets & subsequent scaring along the lines of closure, where they attach to the chordae tendinae.
- Mitral Valve most commonly involved
What pathology is shown in the provided image

- Rhematic Heart Disease
-
Aschoff body: small, subtle areas of necrosis- we can see the inflammatory cells responding to & causing the necrosis
- lymphocytes, plama cells, macrophages (Anitschkow cells
- Elongated cell on bottom photo are Anitschkow cells, which are specially activated, specialized macrophages (caterpillar cells)
- in cross section, look like Owl Eyes or Target
- Definitively diagnostic for Rheumatic Fever
What patology is shown in the provided image?
When does it typically present?

Mitral Valve Stenosis of Rheumatic Heart disease
Chronic Rheumatic Heart Disease, typically presents years or decades after the initial episode of Rhematic Fever
Mitral Valve is most commonly affected
Fish mouth stenosis: chronically scarred, very hard due to calcifications & fibrotic in other areas. Will not open or close properly – usually get stenosis & regurgitation. Surgical correction may be currative

What pathology is shown in the provided image?

Rheumatic Aortic Stenosis
Valve has a “dipped in candle wax” appearance
Commisures are completely fused & thickened (white solid arrows). No opening or closing, so will have stenosis & regurgitation
When do valvular heart disease become clinically apparent?
The severity of the disease depent on what criteria?
May be clinically silent when mild
- Become clinically apparent when one develops either or both:
- Stenosis
- Insufficiency (regurgitation)
- Depends on
- Valve involved
- Severity
- Speed of development
- Compensatory mechanisms
What is the most common cause of the following
Aortic Stenosis
Aortic Insufficiency
Mitral stenosis
Mitral insufficiency
- Aortic Stenosis: wear and tear, bicuspid AV, RHD
- Aortic Insufficiency: dilation of the ascending aorta, usually due to hypertension and aging; RHD
- Mitral stenosis: post-inflammatory scarring of RHD
- Mitral insufficiency: myxomatous degeneration (mitral valve prolapse); RHD
RHD = rheumatic heart disease
What pathology is shown in the provided image?
How common is it?
When is it most often diagnosed?

Congenital Bicuspid Aortic Valve
1.4% of live births
asymptomatic early
early calcific stenosis (b/c bloodflow will be more turbulant across the valve)
often diagnosed in young adulthood
larger cusp often has a midline raphe (yellow arrow)
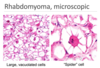
What pathology is shown in the provided images?
What is the major difference between the two images?

Calcific Aortic Stenosis
Congenital bicuspid valve– will develope decades earlier (young adults)
Normal 3 cusps (60-70s)

What pathology is shown in the provided image?

- Gross: calcifications start at the base and eventually extend to the edge of thos cusps & commisures
- Microscopic: nodule that is markedly calcified in teh center (decalcified section, so you aren’t seeing that typical blue)

What are the clinical manifestations of aortic stenosis?
- Clinical Manifestations
- angina
- syncope (fainting)
- congestive heart failure
- murmur
- palpitations
- sudden cardiac death