Tumour Flashcards
Describe this XRay? 15yo boy with painful mass. Differential? Top Diagnosis? Prognosis and Prognostic factors?

EWING SARCOMA
-
Differential
- ewing
- osteosarcoma
- less likely
- leukemia
- rhabdomyosarcoma
- neuroblastoma (<5yo)
- Ewing Sarcoma
- 5-25 years of age
- second most common bone tumor in children
- ~50% are found in the diaphysis of long bones
-
t(11:22) translocation
- found in all cases
- leads to the formation of a fusion protein (EWS-FLI1)
- can be identified with PCR and useful to differentitate Ewing sarcoma from other round cell lesions
-
Prognosis
-
survival
- 60-70% long term survival with isolated extremity disease at presentation and appropriate treatment/tumor response to chemotherapy
- 40% long term survival with pelvis lesions
- 15% long term survival if patient presents with metastatic disease
-
poor prognostic factors
- spine and pelvic tumors
- tumors greater than 100cm3
- < 90% necrosis with chemotherapy
- elevated lactic dehydrogenase levels
- p53 mutation in addition to t(11:22) translocation
-
survival
16yo female with painful thigh. Top Diagnosis? How will she present to you? Radiographic findings typical of this?

Ewing Sarcoma
-
Presentation
- pain often accompanied by fever
- often mimics an infection
-
Physical exam
- swelling and local tenderness
-
Radiographs
- large destructive lesion in the diaphysis or metaphysis with a moth-eaten appearance
- Most common diaphyseal lesion
- Common in pelvis
- lesion may be purely lytic or have variable amounts of reactive new bone formation
- periosteal reaction may give “onion skin” or “sunburst” appearance
- Codman’s triangle
- associated soft tissue mass
-
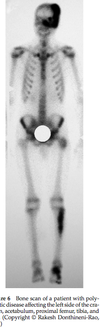
Bone scan
- required as part of staging workup - will show very “hot” lesion
-
MRI
- neccessary to identify soft-tissue extension and marrow involvement
- often shows a large soft tissue component
-
CT chest
- is required for appropriate staging to look for pulmonary metastasis
12 yo male comes in with fever, and painful left hip. Below is his XR. Diagnosis? Managment? Treatment?

Ewing Sarcoma
-
Differential
- infection
- leukemia
- osteosarcoma
- neuroblastoma (if young)
-
Radiology
- permative, moth eatten appearance
- diffuse, aggressive, lytic lesion with periosteal reaction
- may be evidence of onion skinning or sunburst
- ill defined margins, associated soft tissue mass
-
Further work-up
-
Labs - ESR, CRP, WBC, CBC and smear, LDH
- ESR is elevated
- WBC is elevated
- anemia is common
- lactic dehydrogenase (LDH)
-
Bone marrow biopsy
- required as part of workup for Ewing’s to rule out metastasis to the marrow
- also assesses for translocation; translocation in normal marrow has increased risk of relapse
-
Molecular Analysis
- CD99
- PCR can confirm - 11, 22 translocation
-
Bone scan - hot
- __assess mets
-
MRI - assess soft tissue mass
- __marrow involvement
-
CT chest - assess pulmonary mets
- __can help to plan radiation
-
Labs - ESR, CRP, WBC, CBC and smear, LDH
- Consult pediatric oncology and rad onc to discuss imaging
-
Treatment is multi-modal
- preoperative chemotherapy given for 8-12 weeks (3 drugs)
- doxyrubicin (cardiotoxicity)
- vincristine
- cyclophosphamide
- isophosphamide
- etoposide
- Restage with MRI to assess response
- >90% necrosis is good prognosis
- Wide surgical resection with limb salvage or amputation
- Positive margins - re-resection and consider radiation
- OR Radiation if difficult area, but this is falling out of favour due to long term complications
- nonresectable tumor
- wide metastatic disease
- maintenance chemotherapy for 6-12 months
- Monitor for recurrent disease every three months for 2 years, then reduce intervals
- preoperative chemotherapy given for 8-12 weeks (3 drugs)

Poor prognostic factors associated with Ewings
-
The most important factor is clincially evident metastatic disease
- mets to lungs is better than distant boney mets
- skip lesions better than distant boney mets
-
Location
- spine and pelvic tumors (distal tumors have a better prognosis)
-
Size
- tumors greater than 100cm3
- or >8cm
- Age >14 yo
- Male
-
LDH >200IU
- CRP/WBC elevation may be associted with mets and higher tumor burden
- < 95% necrosis with chemotherapy
- p53 mutation in addition to t(11:22) translocation
- Relapse at < 2years
What is important for staging Ewings?
- All present as stage IIb or III
- plain radiographs and MRI of the primary site
- CT chest - pulmonary mets
- Bone Scan - skip lesions, boney mets
- Bone marrow biopsy
- ESR, CRP, LDH
Treatment of Ewings
- preoperative chemotherapy given for 8-12 weeks (3 drugs)
- doxyrubicin (cardiotoxicity)
- vincristine
- cyclophosphamide
- isophosphamide
- etoposide
- Restage with MRI to assess response
- Wide surgical resection with limb salvage or amputation
- Send to pathology to assess for margins and amount of necrosis
- >90% necrosis good prognosis
- positive margins = RT
- OR Radiation if difficult area, but this is falling out of favour due to long term complications
- nonresectable tumor
- wide metastatic disease - should irradiate lungs even when improves with chemo
- technique
- 2-3 cm margin
- 60 grey
- maintenance chemotherapy for 6-12 months
- Monitor for recurrent disease every three months for 2 years, then reduce intervals
- Relapse is common
- treatment associated AML (5 years)
- treatment associated myelosysplasia
- sarcoma 2nd to radiation (10 years); 20%
- carcinoma
Complications associated with radiotherapy in children
- limb length discrepany
- joint contracture
- muscle atrophy
- pathological fractures
- secondary malignancy
Two class of criteria you can use to decide wether to prophylactically fix this?

Harington Critera
- > 50% destruction of diaphyseal cortices
- > 50-75% destruction of metaphysis (> 2.5 cm)
- Permeative destruction of the subtrochanteric femoral region
- Persistent pain following irradiation
Mirel’s Criteria

What is the most common site of metastatic cancer?
thoracic spine
Always make sure to ask about neurological symptoms in any lesion that could be mets
A patient with metastatic disease present with confusion, lethary, polyuria, N/V and are severaly dehydrated. What is the diagnosis? What is the treatment?
Hypercalcemia
- Loop diuretics
- fluid resussitation
Principles of tumor biopsy
-
Prerequisites
- CBC, INR, PTT
- Imaging
- XR, CT
- MRI - to look at most appropriate site of lesion
-
Indications
- bone tumor
- Where multiple sites need biospy (because of tumor heterogeneity)
- Call your nearest tumor specialist to confirm you are dong appropriate biopsy, or ask if they would like referal
-
Incision
- Keep the incision as small as possible
- use longitudinal incision in the extremities
- allows for extension of the incision for definitive management
-
Approach
- do not expose neurovascular structures
- all tissue exposed during the biopsy is considered contaminated with tumor
- maintain meticulous hemostasis
- release tourniquet prior to wound closure
-
Biopsy
- perform thru the involved compartment of the tumor, if possible threw one muscle
- for bone lesions with a soft tissue mass, it is ok to perform the biopsy using the soft tissue mass
- Make a circular or longitudinal hole, <10% bone diameter
- Confirm with your pathologist that you have adequate specimen
-
Closure
- if using a drain, bring drain out of the skin in line with surgical incision
- layered tension-free closure

Prognosis and characteristics of common metastatic cancer?
Thyroid (lytic) - 48 months
Prostate (blastic) - 40
Breast (mixed) - 24
Kidney (lytic) - variable
Lung (lytic) - 6 months
myeloma (lytic) - 2-5 years
Work-up of this patient

-
History
- Pain, qualify the pain, other sites of pain
- This is the most common presenting symptoms
- Constitutional symptoms or specific symptoms to any carcinoma
- Chest pain, abdominal bloating, intolerance to hot and cold
- Neurological symptoms
- Myelopathy, weankness, walking aids, bowel/bladder
- Risk factors - smoking, family history
- Last pap smear, mammogram, colonoscope
- Pain, qualify the pain, other sites of pain
-
Physical
- Look for evidence of primary
- Breast exam, thyroid mass, prostate (rectal)
- Costovertebral tenderness = renal call
- Look for evidence of mets
- Ascultate the lungs, palpate the abdomen
- Abdomenal exam
- Full neurological exam including gait, ASIA
- Look for evidence of primary
-
Workup for older patient with unknown primary
- Plain radiographs
- Full length films of lesion, chest
- CT chest/abdo/pelvis
- Can consider head
- Technetium bone scan - rule out other lesions
- Skeletal survery - Myeloma and thyroid cancer - cold bone scan
- Plain radiographs
-
Blood
- CBC and differential, ESR/CRP, INR, PTT
- LFT, Cr/Urea
- Ca, Phos, Alk Pho, LDH
- ***Hypercalcemia can be fatal to patient
- Helps to rule out metabolic bone disease (hyperparathyroid)
- Immunoelectrophoresis - SPEP, UPEP
- PSA, TSH
-
Imaging
- Radiographs - full length films of affected area
- Blastic - Prostate > breast > lung
- Lytic - renal, lung, thyroid, uterine, adrenal, melanoma, GI
- Not responsive to rads/chemo
- Usually need to treat operatively
- Elbow or knee = lung or renal
- Cortical = lung
-
Biopsy
-
Indications to rule out primary
- No history of cancer
- History of cancer with no evidence of mets
- When there is history of cancer and evidence of mets, ok to send reamings for path
- See the principles of biopsy section
- Use the easiest site to biopsy
- Can do a frozen section intra-op and if the pathologist confirms carcinoma you can proceed with fixation
-
Indications to rule out primary
-
Histology
- Mets - epithelial cells in clumps or glands in a fibrous stroma
- Immunohistochemical stains positive
- Keratin
- CK7 - breast, lung
- TTF1 - lung
-
Once you have the primary
- Med Onc - chemo
- Rad Onc - post-op radiation
- Radiology - if you want them to be embolized pre-op
Treatment prinicples of metastatic lesion
-
Non-op
- Indications
- Small lesions with little disability
- Upper extremity
- Sensitive tumors
- Blastic lesions
- Short expected survival or short condition
- Bisphosphanate - have been shown to decrease secondary skeletal events (SSE) - funded fr breast, myeloma and prostate
-
Radiation
- All require post-op unless death is imminent - otherwise you risk reoperation
- Begin radiation after surgery - 3 weeks
- Make sure you close your wounds well and can leave in the sutures
- Radiation needs to include the entire fixation device
-
Chemo
- Lymphoma/leukemia are very sensitive to rads/chemo so you usually don’t need to do sx
- Indications
-
Operative
- Get imaging of the full bone including joint above and below
- CT may be necessary
- Embolization - renal cell, thyroid
- Post-op RADS - helps to minimize recurrence and for pain control
-
Indications
- Femur fractures
- >2.5cm
- >50% cortical lesion
- Pain refractory to rads
- Mirel’s criteria
-
Hemiarthroplasy or tumor prosthesis
- Required when there in an intra-articular, uncontained lesion
- Can also be done for a proximal femoral neck fracture
- Cemented
- Considerations
- Soft tissue deficient and instability
- Adequate closure of capsule, abductors and ER’s
- High risk of infection
- Soft tissue deficient and instability
-
Prophylactic nailing
- Statically locked
- Recon nail has a higher failure rate for both intertroch and subtroch
- Can augment with PMMA
- Don’t forget to vent the femur if there is no fracture when reaming
- *Doing more than one intramedullary device for multiple lesions can put a lot of stress on the pulmonary system - might be better to stage multiple lesions and allow the patient to recover from each nail
-
ORIF with PMMA
- Indications
- Humerus diaphyseal or metaphyseal with uncontained defect
- Tibia - metaphyseal defect that is extra-articular
- Impending and complete fractures
- Curettage, cement, screw into cement
- Indications
- Get imaging of the full bone including joint above and below
- Spinal neurologic decompression, surgical stabilization, post-op radiation therapy
- Met lesions to spine with compression of neuro elements
Treatment of humeral lesions

Treatment of tibial lesions

Tumors that require chemo
-
Indications
- osteosarcoma (intramedullary and periosteal)
- Ewing’s sarcoma/primative neuroectodermal tumor
- malignant fibrous histiocytoma
- mesenchymal chondrosarcoma
- Rhabdomyosarcoma
- Synovical cell
-
Timing
- pre-op 8-12 weeks
- post-op 6-12 months
-
Common Drug
-
Doxorubicin
- anthracycline antibiotic
- functions as a cytostatic agent
- side effects
- cardiac toxicity
-
Doxorubicin
Describe the lesion. Differential? Diagnosis? Associated conditions?

Non-ossifying fibroma
-
Differential for larger NOF
- ABC
- Chondromyxoid fibroma
- Fibrous dysplasia
- Desmoplastic fibroma
-
Associated conditions
-
Jaffe-Campanacci syndrome
- congenital syndrome of multiple non-ossifying fibromas and
- cafe au lait pigmentation
- mental retardation
- heart, eyes, gonads involved
- neurofibromatosis
- familial multifocal NOF
- ABC
-
Jaffe-Campanacci syndrome
Describe this XR. Differential? Diagnosis?

Differential for metaphyseal fibrous defect
Osteoid osteoma
Intracortical abcess
Stress fracture
Intracortical osteosarcoma
Describe this XR? Differential? Diagnosis? Treatment?

Non-ossifying Fibroma
-
Radiographs
- diagnostic
- metaphyseal, eccentric, “bubbly” lytic lesion surrounded by sclerotic rim
- cortex expansion and thinning
- as bone grows
- migrates to diaphysis
- lesions enlarge (1-7cm)
- lesions become sclerotic as patient approaches skeletal maturity
- avulsion of adductor magnus insertion in the posteromedial aspect of the distal femur may produce a similar looking lesion.
-
CT
- quantitative CT shown to be useful in predicting fracture risk
-
observation
- first line of treatment
- most lesions resolve spontaneously and observation alone is the treatment for most cases
-
casting
- pathologic fracture
- can be treated as per the fracture alone (long leg casting for distal femur pathologic fx)
- Once fracture heals treat with curettage and bone grafting
-
intralesional curettage and bone grafting
- symptomatic and large lesion
- increased risk of fracture shown on quantitative CT
Describe the XR. Differential? Managment?

Malignant Fibrous Histiocytoma
- 20-30% arise from infection or implant
- usually >50yo
-
Presentation
- pain, swelling, pathological fracture
-
Imaging
-
lytic
- no evidence of cortical reaction; too fast for bone to respond
- destructive
- metaphyseal
-
lytic
-
Mangement
- requires a complete WU of solitary bone lesion
- ensure no hypercalcemia
- MRI to look at soft tissue invovlement
- biopsy to confirm
-
Treatment
-
multi-agent chemotherapy and limb salvage resection
-
chemotherapy
- preoperative 8-12 weeks
- maintenance 6-12 months
-
surgical resection
- trend towards limb salvage whenever possible
-
chemotherapy
-
multi-agent chemotherapy and limb salvage resection
Differential for multiple lesions in a young adult
EG
Fibrous dysplasia
Leukemia
Lymphoma
Hemangioendothelioma
Enchondroma / Olliers / Marfucci’s
Osteochondroma / MHE
NOF / Jaffe-Campanacci syndrome
Differential for multiple lesions in an older adult
Paget’s
Metastatic bone disease
Multiple myeloma
Lymphoma
Hyperparathyroidism
Bone infarcts
Lesions that have a cold bone scan
multiple myeloma
melanoma