Trauma - Femur/Tibia (Complete) Flashcards
Per the Lower Extremity Assessment Project (LEAP) study, what were theoutcomes of amputation vs limb salvage?
[JAAOS 2011;19(suppl 1):S20-S22]
No difference in outcomes with amputation versus limb salvage at 2- and 7-year followup
Per the LEAP study, what factors influenced outcomes of amputation/limb salvage?
[JAAOS 2011; 19(suppl 1): S20-S22]
Outcomes were influenced more by patient economic, social, and personal resources than by the initial treatment
- Patient characteristics and the patient’s environment are the factors that most affect outcomes
- Regardless of initial surgical treatment (eg, amputation, limb salvage), medical complications, or the extent of residual physical limitations
Per the LEAP study, what is the difference in cost for amputation vs limb salvage?
[JBJS 2010;92:2852-68]
The lifetime cost for the amputation group was estimated to be about three times higher secondary to prosthesis-related expenses
Per the LEAP study, what role should an insensate foot play in deciding between amputation vs limb salvage?
[JBJS 2010;92:2852-68]
An insensate foot on presentation should not be a critical indication for amputation, as there was a return of plantar sensation by two years in the majority of cases
What are the indications for lower extremity amputation following lower extremity trauma?
[JBJS 2010;92:2852-68]
Absolute
- Blunt or contaminated traumatic amputation
- Mangled extremity in critically injured patient in shock
- Crushed extremity with arterial injury and a warm ischemia time greater than 6 hours
Relative indications
- Severe bone or soft tissue loss
- Anatomic transection of the tibial nerve
- Open tibial fracture with serious associated polytrauma or a severe ipsilateral foot injury
- Prolonged predicted course to obtain soft tissue coverage and tibial reconstruction
What is the blood supply to the femoral head?
[JAAOS 2016;24:515-526]
Primary = medial femoral circumflex artery
- Femoral artery → profunda femoris artery → medial femoral circumflex artery → ascending branch → deep branch
What is the Garden Classification of femoral neck fractures based on AP?
Type I – incomplete, valgus impacted
Type II – complete, nondisplaced
Type III – complete, partial displacement
Type IV – complete, full displacement

What is the Simplified Garden Classification for femoral neck fractures?
- Nondisplaced = Garden I and II
- Displaced = Garden III and IV
What is Pauwel’s classification of femoral neck fractures?
Based on the obliquity of the fracture line with respect to the horizontal
- Type I - 0-30 degrees
- Type II - 30-50 degrees
- Type III - >50 degrees
- Most unstable
- Highest risk of nonunion and AVN

What are signs of adequate femoral neck reduction?
- Restoration of Shenton’s line
- Garden alignment index
- Angle of compression trabeculae to femoral shaft on AP should be 160 degrees
- Angle of compression trabeculae to femoral shaft on lateral should be 180 degrees
- Lowell’s alignment theory
* Head neck junction should make a smooth ‘S’/reverse ‘S’ on all views - Restoration of the neck shaft angle

What are the techniques for closed reduction of a femoral neck fracture to obtain anatomical alignment?
- Leadbetter [World J Orthop 2014 July 18; 5(3): 204-217]
- Hip flexion to 45
- Slight abduction
- Longitudinal traction
- Internal rotation
- Extension
- Flynn [Injury; 5: 309-217]
- Flexion of the hip with slight abduction
- Traction in line with the long axis of the femoral neck
- Extend and internally rotate the hip while traction is maintained
What residual deformity following femoral neck reduction is not acceptable?
[JOT 2015;29:121–129]
- Varus angulation
- Inferior offset
- Retroversion
***These 3 factors increase the risk of nonunion, loss of reduction and osteonecrosis
In the young patient, what means of anatomical reduction is preferred – open vs. closed?
[JOT 2015;29:121–129]
- Both are acceptable as long as anatomical reduction achieved
- If closed unsuccessful proceed to open reduction
What approaches are used for open reduction of a femoral neck fracture in the young adult and what are the advantages and disadvantages?
[JOT 2015;29:121–129]
- Anterior (Smith-Peterson)
- Advantage
- Excellent exposure of anterior femoral neck and subcapital region
- Disadvantage
- Second lateral incision needed for internal fixation
- Anterolateral (Watson-Jones)
- Second lateral incision needed for internal fixation
- Advantage
- Single incision
- Disadvantage
- Limited subcapital exposure
What are the indications for cannulated screws and SHS in femoral neck fractures?
[JOT 2015;29:121–129]
- Garden I and II
* Cannulated screws or SHS - Garden III and IV
- Closed reduction with anatomical alignment, assess Pauwels angle
- Pauwel’s type I and II = cannulated screws or SHS
- Pawuel’s type III = SHS
- Comminution and basicervical = SHS
Based on the FAITH trial which construct (cannulated screws vs DHS) results in less reoperation within the first 24 months?
Neither, equal reoperation between cannulated screws and SHS
Based on the FAITH trial which subgroups may benefit from SHS (vs cannulated screws)?
- Smokers
- Basicervical fractures
- Displaced fractures
What is one disadvantage of SHS shown in the FAITH trial compared to cannulated screws?
Higher risk of AVN (9% vs. 5%)
What are the technical points for the placement of cannulated screws for femoral neck fracture?
[JOT 2015;29:121–129]
- 3 cannulated screws (6.5, 7.0 or 7.3mm)
- Parallel inverted triangle configuration
- Inferior – along calcar, resists inferior displacement
- Posterosuperior – resists posterior displacement
- Anterosuperior
- Start point for the inferior screw should be at or above the LT
- Screw threads should be entirely within the head fragment and within 5mm of subchondral bone

What modifications can be made to the cannulated screw construct to enhance fixation (in femoral neck)?
[JOT 2015;29:121–129][Eur J Orthop Surg Traumatol (2016) 26:355–363]
- 4th screw along posterior cortex in setting of posterior comminution
- Add washers in osteoporotic bone to prevent penetration through lateral cortex and enhance lag effect
- Parallel or divergent screws (avoid convergent)
- Trochanteric lag screw in high risk patterns (high Pauwels angle)
- Inferomedial buttress plate
What are the advantages of a derotation screw when using a SHS?
[Eur J Orthop Surg Traumatol (2016) 26:355–363]
- Protect against rotation/displacement and risk of AVN
- Biomechanically stronger
What is the tip-apex distance and the calcar referenced tip-apex distance – what is the significance?
[J Orthop Surg Res. 2018; 13: 106]
- TAD = sum of the distances from the tip of the lag screw to the apex of the femoral head on AP and lateral radiographs
- CalTAD = sum of a TAD in the lateral view and the distance, in the AP view, between a line tangent to the medial cortex of the femoral neck and the tip of the lag screw
* TAD >25mm, CalTAD >25 and combined TAD and CalTAD >50mm increase the risk of lag screw mobilization and cutout

What is the management of femoral neck nonunion after ORIF?
[JOT 2006;20:485–491]
- Elderly patient
* Total hip arthroplasty or hemiarthroplasty - Young patient
- Valgus intertrochanteric osteotomy with blade plate (Pauwels)
- Converts shear forces into compressive forces
- Valgus intertrochanteric osteotomy with sliding hip screw (contemporary)
- Potential advantages
- Reaming creates local autograft
- Sliding screw maximizes compression
- Less technically demanding than blade plate
- Disadvantages
- Greater bone removal
- Less rotational control of the proximal segment
- Potential advantages
What are the steps in performing valgus intertrochanteric osteotomy for femoral neck nonunion?
[JOT 2006;20:485–491]
- Determine the osteotomy angle
- Goal = fracture plane less than 30°
- Osteotomy angle = current angle minus the goal angle
- Advance the guide pin into the femoral head
* Ream, tap and advance the lag screw - The superior limb of the closing wedge osteotomy starts just below the lag screw (perform first)
* Ends half way across the width of the femur as it intersects the inferior limb - The inferior limb of the closing wedge osteotomy passes just below the LT
* Do not complete medial aspect of osteotomy until the side plate is attached - Attach side plate to the lag screw
- Complete the inferior limb osteotomy medially and use the side plate to rotate the proximal femur fragment into valgus
- Use the compression screw of the SHS and fix the side plate with cortical screws

What are Kaufer’s five variables affecting the biomechanical strength of repair in intertrochanteric hip fractures?
- Surgeon-independent variables
- Bone quality
- Fracture pattern or fracture stability
- Surgeon-dependent variables
- Implant choice
- Quality of fracture reduction
- Positioning of the implant
What are the characteristics of stable intertrochanteric hip fractures?
[J Orthop Trauma 2015;29:S4–S9]
- Resist displacement after adequate reduction and fixation
- Includes:
* 2-part intertroch fractures with intact posteromedial buttress - Treated with either IM device or SHS
What are characteristics of unstable intertrochanteric hip fractures?
[J Orthop Trauma 2015;29:S4–S9]
- Tend to collapse after adequate reduction and internal fixation
- Includes:
- Posteromedial comminution
- Reverse obliquity
- Subtrochanteric extension
- Lateral wall comminution (reverse obliquity equivalent)
- Reverse oblique variant
- Fracture orientation when viewed on AP looks typical, however on the lateral the fracture extends from proximal-anterior to distal-posterior
- Treated with IM device (ie. Contraindications for SHS)
If a SHS is used and a lateral wall blowout is identified or caused iatrogenically, what are the surgical options?
[JAAOS 2016;24:e50-e58]
- SHS with the addition of a trochanteric stabilization plate
- Conversion to a cephalomedullary nail
What is an acceptable range of neck-shaft angle compared to the patient’s opposite side (in intertrochanteric hip fractures)?
[J Am Acad Orthop Surg 2004;12:179-190]
5o of Varus to 20o of Valgus
- valgus is more acceptable as it reduces the bending stress on the implant and may offset the shortening that occurs with fragment impaction
What is the optimal position of the lag screw for SHS?
- Center-center in the femoral neck
* Avoid anterior/superior placement and posterior/inferior placement - ‘Deep’ on AP and lateral
* IE. Tip-Apex distance <25mm

What are the advantages of an intramedullary sliding hip screw (i.e nail) vs. a standard SHS in intertrochanteric hip fractures?
[J Am Acad Orthop Surg 2004;12:179-190]
- Closed, percutaneous
- Minimizes fracture zone insult
- Reduces perioperative blood loss
- Decreased bending moment on the lag screw (shorter lever arm)
- Intramedullary buttress prevents femoral shaft medialization
How can anterior cortical abutment or perforation be avoided when using a long cephomedullary nail?
[JAAOS 2016;24:e50-e58]
- Anterior cortical perforation secondary to a nail-femoral bow mismatch is a complication unique to long nails
- Ways to prevent include:
- Avoid posterior GT entry point
- Accept only a central or slightly posterior position of the guidewire in the canal distally
- Use a shorter nail in an excessively bowed femur
- Avoid overreaming or eccentric reaming
- Leave the guidewire in place until the nail is fully seated
- Use a smaller diameter nail
What are the disadvantages of long nails versus short nails in the management of intertrochanteric fractures?
[JAAOS 2016;24:e50-e58]
- Longer surgical time
* Due to time for reaming and free hand distal locking screw - Increased blood loss and higher incidence of transfusions
- Higher cost
- Distal femur metaphyseal fracture
* Unique to long nails as stress riser is distal
What are the indications of a long nail over a short nail in intertrochanteric hip fractures?
[JAAOS 2016;24:e50-e58]
- Reverse obliquity fractures – AO/OTA 31-A3
- Subtrochanteric extension – AO/OTA 31-A2.3
* Extension >1cm below the LT - Capacious proximal canal
* Short nails will result in toggle and an overall varus alignment - Pathological fractures
What are the surgical options in the event of a diaphyseal femoral fracture with a short cephalomedullary nail in place?
[JAAOS 2016;24: e50-e58]
- Early – convert to long nail
- Late – plate osteosynthesis
What is the Z-effect and reverse Z-effect complication (in context of intertrochanteric hip fracture)?
[Patient Safety in Surgery 2011, 5:17]
- Unique complication when treating intertrochanteric fractures with IM nails and two proximal lag screws (eg. recon nail)
- Z-effect =
- Lateral migration of the inferior screw
- Varus collapse
- Perforation of the femoral head by the superior screw
- Reverse Z-effect =
- Lateral migration of the superior screw
- Medial migration of the inferior screw
What is the consequence of shaft medialization in fixation of interrtochanteric hip fractures?
- Decreases femoral offset
- Decreases abductor muscle efficiency
- Increases joint reactive forces
- Valgus knee alignment
What is the definition of the subtrochanteric region?
Area extending 5cm below the lesser trochanter
What are the deforming forces on the proximal fragment in a subtrochanteric femur fracture?
- Abduction – gluteus medius and minimus
- Flexion – iliopsoas
- External rotation – short external rotators

What are the deforming forces on the distal fragment in a subtrochanteric femur fracture?
Adduction and shortening – adductors

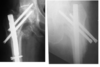
What is the Russel-Taylor classification for subtrochanteric fractures?
Type I – spare the piriformis fossa
Type II – involve the piriformis fossa
Subclassified as A or B
- Type A do not involve the lesser trochanter
- Type B do involve the lesser trochanter
*** Historically used to differentiate between fractures that would amenable to an IM nail (type I) and those that required some form of a lateral fixed angle device (type II)
- Current interlocking options with both trochanteric and piriformis entry nails allow for treatment of type II fractures with intramedullary implants

What is the most common malunion following fixation of subtrochanteric fractures?
Varus and flexion (procurvatum)
What are techniques to avoid varus malreduction when nailing a subtrochanteric fracture?
[JOT 2018;32:e151–e156)][JOT 2015;29:S28–S33]
- Slight medialization of start point with a trochanteric nail
* Also leads to less abductor damage - Joysticks
- Femoral distractor
- Finger reduction tool (spoon)
- Blocking screws
- Schanz pins
- Clamps
- Lateral decubitus position neutralizes deforming forces
- Unicortical plating
What is the blood supply to the femur?
[Rockwood and Green 8th ed. 2015]
- Medullary
* 1-2 nutrient vessels arising from the profunda femoral artery and entering the proximal ½ of the femur posteriorly at the linea aspera - Periosteal
What is the classification system for femoral shaft fractures?
[Rockwood and Green 8th ed. 2015]
- Winquist and Hansen system
- Based on the percentage of intact femoral shaft at the fracture site
- Grade 0
- No comminution
- Grade I
- ≥75% cortical contact
- Small butterfly fragment or minimal comminution <25%
- ≥75% cortical contact
- Grade II
- ≥50% cortical contact
- Butterfly fragment or comminution 25-50%
- ≥50% cortical contact
- Grade III
- Minimal cortical contact
- Butterfly fragment or comminution 50-75%
- Minimal cortical contact
- Grade IV
- No cortical contact
- Complete cortical comminution
- Segmentally comminuted
2. AO-OTA classification
- No cortical contact
- Type A – simple
- Type B – wedge
- Type C – complex

What are the indications for a retrograde nail in a femoral shaft fracture?
- Ipsilateral femoral neck fracture
- Ipsilateral acetabular fracture
- Distal femur fracture
- Bilateral femur fracture
- Multisystem trauma
- Floating knee
- Obesity/pregnancy
* Relative contraindication for antegrade nail
What are the IMN start points?
- Antegrade – depends on nail
* Both GT and piriformis fossa are acceptable - Retrograde
- Anatomically
- 1.2cm anterior to the femoral PCL insertion and centered in the intercondylar notch [JOT 2015]
- Radiographically
- Midline (or just medial) in intercondylar notch and just anterior to Blumensaats line
What are the advantages of reaming for femur IM nails?
- Allows for larger stiffer nail to be passed
- Increases the length of the isthmus
* Increasing bone-nail contact, thereby increasing stiffness - Autograft bone
What are the disadvantages of reaming for femur IM nails?
- It increases the length of the surgical procedure
- It may increase the chance of pulmonary fat emboli
- It can create heat necrosis
- It temporarily destroys part of the endosteal blood supply.
What are techniques to limit fat emboli syndrome/appropriate reaming technique/minimize intramedullary pressure (femoral shaft fracture)?
[J Orthop Trauma 2009;23:S12–S17]
- Sharp reamers
- Narrow reamer shaft
- Long lead head taper
- Enlarged cutting flutes
- Flexible shaft
- Slow driving speed
- High revolution
- Venting
- Reamer-irrigator-aspirator (RIA)
- Hollow reamers
- Over-ream compared to size of nail
What are the advantages and disadvantages of using a fracture table for nailing diaphyseal femur fractures?
[JAAOS 2017;25:e251-e260][JBJS 2002;84(9):1514-1521]
Advantages
- Fewer assistants
- Easier femoral head and neck imaging
- Better if thoracic trauma
Disadvantages
- Longer setup
- Nerve palsies
- Pudendal, femoral, sciatic
- Compartment syndrome in the contralateral leg
- Decreased access to other body parts
- Increased internal malrotation >10o
What are advantages and disadvantages of the lateral decubitus position (vs. supine) for nailing diaphyseal femur fractures?
[JAAOS 2017;25:e251-e260]
Advantages
- Easier access to proximal femur
- Easier start point access in larger patients
- Reduces sagittal plane deformity of the distal fragment in relation to the proximal fragment in a proximal diaphyseal shaft fracture
Disadvantages
- Unfamiliarity with positioning
- Pulmonary complications in patients with lung injuries
- Difficulty obtaining lateral images of the proximal femur
- Increased risk of angular or rotational malalignment
- Requires repositioning for bilateral femur nailing
What are methods for assessing restoration of length in diaphyseal femur fracture nailing?
[JAAOS 2017;25:e251-e260]
Measure contralateral femur length from starting point to distal physeal scar using a extra-medullary ruler or sterile IM nail
What are methods for assessing restoration of rotation in diaphyseal femur fracture nailing?
[JAAOS 2017;25:e251-e260]
- Assess the LT profile in comparison to the contralateral side
* Take a perfect lateral of the knee or an AP with patella centered over the distal femur then take an AP of the hip - Key in fracture fragments
- Cortical thickness
- Diameter difference between proximal and distal fragment
- Clinical comparison of contralateral leg rotation (hip IR and ER)
- Inherent anteversion built into the nail [J Orthop Trauma 2014;28:e34–e38)]
* By centering the proximal locking screws in the femoral head and aligning the distal locking screws with the femoral condylar axis, the proximal and distal fracture fragments are positioned in the same anteversion inherent to the nail construct - Fluoroscopic measurement of anteversion [JAAOS 2011;19:17-26]
- Assess uninjured side first
- True lateral view of the proximal femur followed by true lateral of ipsilateral knee
- The difference in angles of the fluoro between the two measurements determines the version
What are the deforming forces on the distal fragment in femur diaphyseal fractures?
[JAAOS 2017;25:e251-e260]
- Apex medial due to tension of IT band
- Apex posterior due to tension of gastrocnemius
What are reduction techniques for diaphyseal femur fracture nailing?
[JAAOS 2017;25:e251-e260]
- Traction
- Fracture table
- Skeletal traction (distal femur or proximal tibia)
- Manual traction
- Noninvasive reduction techniques
- Stack of towels in apex posterior deformity
- Radiolucent triangle in distal fractures to relax the gastrocs
- Pushing reduction force (eg. mallet)
- Pulling reduction force (eg. towel or laporotomy sponge)
- F-tool
- Medullary femoral reduction tool (ie. Reduction spoon)
- Percutaneous reduction techniques (stab incisions)
- Spiked-ball pusher
- Shoulder hook
- Fracture reduction clamps
- External fixation half pins
- Blocking screws
- Placed on concave side in the mobile segment
- Open reduction (direct lateral subvastus approach)
- Placed on concave side in the mobile segment
- Bone reduction forceps
- Plating with unicortical screws
What assessments should be made prior to completion of femur nailing?
[JAAOS 2017;25:e251-e260]
- Confirm acceptable length, alignment and rotation
- Femoral neck fracture ruled out by fluoro
- Knee ligament examination
- Assess compartments
What are the described traction table-related complications?
[JAAOS 2010;18:668-675]
- Malrotation and malalignment
- Increased incidence of femoral malrotation >10°
- Compared to manual traction
- Misjudging start point in obese patients results in varus/valgus malalignment
- Neurological injury
- Pudendal nerve injury due to perineal post
- Results in perineal dysesthesia and/or erectile dysfunction
- Sciatic nerve injury in the well leg
- Due to hemilithotomy position with hip flexed to 90° and knee flexed to <90°
- Common peroneal nerve injury in the well leg
- Due to hemilithotomy position compression against leg holder or compression due to straps/wraps
- Perineal soft tissue injury
- Due to hemilithotomy position compression against leg holder or compression due to straps/wraps
- Due to compression against the perineal post (can cause necrosis)
4. Compartment syndrome - Occurs in well leg due to the hemilithotomy position
- Direct calf compression and vascular hypoperfusion
What are ways to reduce the risk of traction table-related complications?
[JAAOS 2010;18:668-675]
- Use a flat top table and free extremity draping in the obese patient
- Perineal post should be placed between the genitalia and the contralateral leg
- Use a well padded, large diameter (>10cm) perineal post
- Avoid adduction of the leg across neutral
- Avoid well leg hemilithotomy position
- Limit traction time
* If traction time >2 hours release the traction
What imaging should be obtained and reviewed in the perioperative management of a femoral shaft fracture to reduce the chance of missed femoral neck fractures?
[Rockwood and Green 8th ed. 2015]
- Obtain preoperative hip xrays
- If CT obtained for abdominal/pelvic injuries review for hip fracture
- Obtain intraoperative fluoro images before nailing
- Obtain intraoperative fluoro images after nailing with the hip in 10-15 degrees of internal rotation
- Obtain postoperative hip radiographs prior to leaving the operating room
In what percentage of femoral shaft fractures does an ipsilateral femoral neck fracture occur?
[JAAOS 2018;26:e448-e454]
2-9%
In what percentage of ipsilateral femoral neck and shaft fractures is the femoral neck fracture missed?
[JAAOS 2018;26:e448-e454]
- Historically, up to 30%
- Recently, 6-22%
In ipsilateral femoral neck and shaft fractures – who is the typical patient and what is the typical femoral shaft and neck fracture?
[JAAOS 2018;26:e448-e454]
- Typical patient:
- Avg age is 35
- 75% are male
- Typical femur fracture
- Comminuted, middle 1/3
- Open in 15-33% of cases
- Typical femoral neck fracture
* Basicervical, vertically oriented and undisplaced in 60% of cases - Associated injuries
- 75-100% have multisystem injuries
- 20-40% have ipsilateral knee injuries
- Ligamentous injury
- Tibial plateau fracture
- Patella fracture
- Knee dislocation
What is the commonly described mechanism for ipsilateral femoral neck and shaft fractures?
[JAAOS 2018;26:e448-e454]
“Dashboard” Injury
- Axial force creates mid-shaft comminuted fracture
- If hip is abducted, femoral neck or acetabular fracture can occur
- Posterior hip dislocation if adducted
What is the Tornetta protocol (2007) for diagnosing ipsilateral femoral neck fractures in the context of a femoral shaft fracture?
[JAAOS 2018;26:e448-e454]
- AP internal rotation radiograph of the hip
- Fine-cut (2-mm) CT scan through the femoral neck
- Intraoperative fluoroscopic lateral view of the hip
- Postoperative AP and lateral radiographs of the hip in the operating room
* Outcomes:*
- Reduced rate of delay in diagnosis by 91%
- Cannada study (2009) - 2mm CT scan missed 18% of ipsilateral femoral neck fractures
What is the recommended management of a combined femoral shaft and hip fracture?
[Rockwood and Green 8th ed. 2015] [JAAOS 2018;26:e448-e454]
[Rockwood and Green 8th ed. 2015]
- 2 constructs
- Fix the hip fracture first
- Subcapital and transcervical with mutiple lag screws
- Cannulated screws
- Basicervical and intertrochanteric with sliding hip screw
- Fix the femoral shaft second
- Usually retrograde nail
- Lateral plating also acceptable
[JAAOS 2018;26:e448-e454]
- Once a femoral shaft fracture is diagnosed, get AP pelvis and AP/lateral hip XRs
- If a CT of the pelvis is ordered for other reasons, this is reviewed as a “free look” at the femoral neck
- Do not routinely order a CT solely to evaluate the femoral neck
- If displaced femoral neck fracture:
- ORIF of femoral neck with SHS or cannulated screws
- Open reduction through anterior approach
- Lateral appraoch for fixation
- Screws/fixation placed in the posterior
half of the shaft so retrograde nail can pass anterior to them
- Femoral shaft fracture is then reduced, and a retrograde femoral nail is placed with the tip of
the nail passing anterior to the screws of the proximal implant
3 Femoral shaft fracture without a femoral neck fracture diagnosed preoperatively:
- Intraop assessment of the femoral neck with fluoroscopy in OR, with beam angled 10o to visualize the neck in profile
- If a neck fracture is identified, use 2-implant fixation with closed reduction of neck
- If no neck fracture is identified, a CM nail with two proximal interlocking screws placed across the femoral neck is used
Notes:
- Most important factors related to femoral neck union is quality of reduction
- Treatment with an antegrade nail with cannulated screws adjacent to the nail is typically used only in patients with a neck fracture that is identified intraoperatively after nail insertion
- Neck screws are placed anterior to nail
- If anterior and posterior screws are attempted,
an iatrogenic subtrochateric fracture can occur
What are the complications associated with treatment of ipsilateral femoral neck and shaft fractures?
[JAAOS 2018;26:e448-e454]
- Femoral neck
- Nonunion 5%, Malunion 5%
- Both lower than those for isolated femoral neck fractures
- Risk factors for nonunion/AVN:
- Delay in the diagnosis of the femoral neck fracture
- Amount of initial displacement
- Malreduction at the time of fixation
- Femoral shaft
- Nonunion - up to 20%
- Higher than the rates reported for isolated femoral shaft fractures
- Due to higher energy injuries that have a higher proportion of open fractures compared with isolated femoral shaft fractures
- Open fracture is the greatest risk factor for nonunion of the femoral shaft component
What is the incidence of femoral malrotation following IMN?
[JAAOS 2011;19:17-26]
Up to 27.6% (range 2.3-27.6%)
Which malrotation is more poorly tolerated?
[JAAOS 2011;19:17-26]
External malrotation
What pattern of femoral shaft fracture has the highest risk of malrotation?
[JAAOS 2011;19:17-26]
- Transverse
- Segmental
- comminuted
- Bone loss
What type of malrotation is more common with proximal vs. distal femoral shaft fractures?
[JAAOS 2011;19:17-26]
- Proximal femur fractures = internal malrotation
- Distal femur fractures = external malrotation
What type of malrotation is associated with fracture table vs. supine/free-leg/lateral bump position?
[JAAOS 2011;19:17-26]
- Internal malrotation = fracture table
- External malrotation = supine/free-leg/lateral bump position
How is femoral version determined with CT?
[JAAOS 2011;19:17-26]
Angle between a line drawn through the center of the femoral neck and a tangent drawn across the posterior aspect of the distal femoral condyles
When should femoral malrotation be treated surgically?
[JAAOS 2011;19:17-26]
- No universally accepted guidelines exist for defining the degree at which malrotation becomes significant
- Intervene when patient determines malrotation to be functionally or cosmetically unacceptable
What investigations should be utilized to determine extent of femoral malrotation and plan correction (post IMN)?
[JAAOS 2011;19:17-26]
CT rotational profile
How is femoral malrotation addressed surgically?
[JAAOS 2011;19:17-26]
- Prior to union
- Remove distal locking screw and correct rotation
- If correction is <20° distal screw cutout is a concern, consider using alternate locking holes
- Following union
- Remove nail
- Perform transverse osteotomy
- Correct rotation and reinsert nail and locking screws
- Rotation correction
- Can be achieved by placing Steinmann pins in trochanteric region and distal femoral region prior to nail removal
- Angle of correction can be measured with goniometer relative to the pins
What is an atypical femur fracture?
[JAAOS 2015;23:550-557]
Diphosphonate-related fracture
What are the major and minor criteria of atypical femur fractures based on the 2013 American Society for Bone and Mineral Research Task Force Revised Case Definition?
[JAAOS 2015;23:550-557]
Major
- No or minimal trauma
- Fracture originates at the lateral cortex and is substantially transverse in orientation
- Complete fractures may be associated with a medial spike
- No or minimal comminution
- Thickening of the lateral cortex (beaking)
Minor
- Generalized increase in cortical thickness of the femoral diaphysis
- Unilateral or bilateral prodromal symptoms
- Bilateral incomplete or complete femoral diaphyseal fractures
- Delayed fracture healing
Generally, when is disphosphonate therapy started?
[JAAOS 2015;23:550-557]
When the T-score ≤-2.5 at the femoral neck or spine
What is the function of disphosphonates?
[JAAOS 2015;23:550-557]
Binds to hydroxyapatite crystals
- Results in:
- Decreased osteoclast function
- Induces osteoclast apoptosis
- Inhibit bone resorption
When is a drug holiday recommended from diphosphonates?
[JAAOS 2015;23:550-557]
- High risk patient
- Hip T score ≤ -2.5, previous fracture of the hip or spine or ongoing high dose steroid therapy
- Drug holiday not justified
- Moderate risk patient
- (Hip T score> -2.5 and no prior hip or spine fracture)
- Consider drug holiday after 3-5 years of alendronate, risedronate or zoledronic acid therapy
- Low risk patient
- (Did not meet criteria for treatment at time of treatment initiation)
- Discontinue therapy
What are the risks and adverse effects associated with bisphosphonate therapy?
[The American Journal of Medicine (2013)126:13-20]
- Osteonecrosis of the jaw
- Atypical femur fractures
- Atrial fibrillation
- GI intolerance
- Hypocalcemia
- Flu-like symptoms
* Acute phase reaction with monthly dosing - Inflammatory eye disorders
What is the management of an atypical femur fracture?
[JAAOS 2015;23:550-557]
- Discontinue diphosphonate therapy and consult endocrinology
- Assess Vitamin D and calcium intake and supplement as needed
- Evaluate the contralateral femur for atypical fractures
* Consider radiographs, MRI, CT, bone scan - Surgery for incomplete and complete atypical femur fractures
- Although nonsurgical can be attempted for incomplete fractures the outcomes are poor
- Intractable pain, complete fracture
- IM nailing preferred
- Bilateral atypical fractures
- Decision of single vs. staged fixation is patient dependent
What can be considered in the management of delayed or nonunion of an atypical femur fracture?
[Hip Pelvis. 2018 Dec; 30(4): 202–209]
Endocrinology referral for teriparatide
- Recombinant form of parathyroid hormone (PTH)
What are the deforming forces on the distal femur in a distal femur fracture?
[Rockwood and Green 8th ed. 2015]
- Gastrocnemius
* Cause extension of the distal fragment (apex posterior) - Hamstrings, quadriceps and adductors
* Cause shortening and varus
In open distal femur fractures where is the typical wound located?
[Rockwood and Green 8th ed. 2015]
Anterior proximal to patella with variable degree of quadriceps tendon injury
What is the most common ligament injury associated with distal femur fractures?
[Rockwood and Green 8th ed. 2015]
ACL
What classification system is used for distal femur fractures?
[Rockwood and Green 8th ed. 2015]
OTA
- A – extra-articular
- (1) simple
- (2) metaphyseal wedge
- (3) metaphyseal complex (comminuted)
- B – partial articular
- (1) lateral condyle sagittal
- (2) medial condyle sagittal
- (3) coronal (Hoffa)
- C – complete articular
- (1) articular and metaphyseal simple
- (2) articular simple/metaphyseal complex
- (3) articular complex

Which condyle is most likely to be involved in a Hoffa fracture?
[Bone Joint J 2013;95-B:1165–71]
Lateral condyle
What is the classification of Hoffa’s fractures?
[Bone Joint J2013;95-B:1165–71]
Letenneur classification
- 3 types based on distance from the posterior cortex of the femur shaft
- Type 1 – fracture parallel to the posterior cortex
- Type 2 – fracture posterior to the posterior cortex of variable size
- Type 3 – oblique fracture

What are important anatomical features of the distal femur to be mindful of during surgery?
[Rockwood and Green 8th ed. 2015]
Trapezoidal-shape viewed end on
- Posterior wider than anterior
- 25° inclination on medial surface
- 15° inclination on lateral surface

What are the goals of operative treatment of distal femur fractures?
[Rockwood and Green 8th ed. 2015]
- Anatomic reduction of articular surface
- Restore length, alignment and rotation
- Stable internal fixation
- Early ROM
- Delayed protected WB
What surgical approaches can be considered for distal femur fractures?
[Rockwood and Green 8th ed. 2015]
- Lateral approach (most common)
- Lateral incision centred distally over the lateral epicondyle
- Incise fascia lata
- Sub-vastus lateralis
- Limited visualization of the intercondylar notch and medial condyle
- Anterolateral approach (“Swashbuckler”) [JOT 1999; 13(2): 138-140]
* Midline incision curved slightly laterally proximally- Fascia is split inline with incision and elevated off underlying vastus lateralis
- IT band is retracted laterally
- Lateral parapatellar arthrotomy is made
- Vastus lateralis is separated from the intermuscular septum and IT band
- Retractor is placed under the quadriceps muscle elevating them off the femur medially and everting the patella medially
* Provides excellent articular exposure - Exposes distal femur
- Minimal quads disruption
- Incision can be used in future TKA
- Lateral mini-invasive
- MIPO/LISS systems
- Fixation of condyle through incision
- Plate passed proximally with screws through stab incisions
- Medial approach

What are the construct options for distal femur fracture fixation based on fracture pattern in general (based on OTA classification)?
[Rockwood and Green 8th ed. 2015]
- OTA A
- Lateral periarticular locking plate (lateral approach)
- Minimally invasive locked plate
- Retrograde nail (locked)
- OTA B
- Lateral or medial condyle sagittal fracture
- Buttress plating
- Coronal fracture (Hoffa)
- A-P countersunk screws
- Small or mini-frag buttress plate
- If nonarticular apex present
3. OTA C
- If nonarticular apex present
- Anterolateral approach for anatomic reduction and fixation of articular surface followed by lateral locking plate
- Minimally invasive locking plate or retrograde nail can also be used

What is the blood supply to the tibia?
[Rockwood and Green 8th ed. 2015]
- Medullary (inner 70-75%)
- Derived from the main nutrient artery
- Branch of posterior tibial artery
- Enters tibia in proximal 1/3
- Branch of posterior tibial artery
- Periosteal (outer 25-30%)
What is the Classification of tibia shaft fractures?
AO/OTA classification
- A - simple fractures
- B - wedge fractures
- C - complex fractures

What are the associated injuries with a tibial shaft fracture?
[Rockwood and Green 8th ed. 2015]
- Compartment syndrome
- Ankle injuries
- Lateral ligament injuries
- Fractures of the posterior, medial and lateral malleoli
- Posterior malleolar fractures occur in:
- 8-9% of tibial shaft fractures
- 25-39% of distal 1/3 spiral fractures
3. Floating knee
4. Fracture extension into tibial plateau
- Posterior malleolar fractures occur in:
- Rare, but can be displaced during IM nailing
5. Knee ligamentous injury
6. Proximal tibiofibular joint dislocation
What radiographs are indicated in a tibial shaft fracture?
[Rockwood and Green 8th ed. 2015]
- Tibia/fibula AP+lateral
- Knee AP+lateral
- Ankle AP, mortise+lateral
What are acceptable alignment parameters for tibia fractures (amenable to conservative care)?
<5 degrees of varus/valgus angulation
<10 degrees of AP angulation
<10 degrees of rotation
<1cm of shortening
>50% of cortical apposition
What are indications for surgery in tibial shaft fractures?
[Miller’s, 6th ed.] [Rockwood and Green 8th ed. 2015]
- Unacceptable alignment
- Soft tissue injury not amenable to cast
- Floating knee (ipsilateral femoral fracture)
- Polytrauma
- Morbid obesity
- Unreliable patient
- Vascular injury
- Patient preference (favour early WB and joint ROM)
What is the Tscherne classification for closed tibial shaft fractures?
[CORR 2017 Feb;475(2): 560–564][AOfoundation]
Grade I
- Soft tissue injury – none or minimal
- Energy – low
- Typical fracture – spiral
Grade II
- Soft tissue injury – superficial abrasion or contusion from fragment pressure within
- Energy – mild to moderate
- Typical fracture – rotational ankle fracture-dislocation
- Pressure from unreduced medial malleolus fracture
Grade III
- Soft tissue injury – deep abrasion and local skin and muscle contusion from direct injury
- Also imminent compartment syndrome
- Energy – high
- Typical fracture – segmental tibia fracture from direct blow
Grade IV
- Soft tissue injury – extensive skin contusion
- Myonecrosis
- Degloving
- Vascular injury
- Compartment syndrome
- Energy – high
- Typical fracture – comminution, severe

In displaced tibia shaft fractures with an intact fibula, what malaligment is the tibia prone to?
[Rockwood and Green 8th ed. 2015]
Varus
- Therefore, it is a relative indication for surgery)
- Also, risk for nonunion
What are the approaches for intramedullary nailing of tibial shaft fractures?
[Rockwood and Green 8th ed. 2015]
- Medial parapatellar (most common)
- Lateral parapatellar
- Patellar tendon split
- Suprapatellar
What is appropriate patient positioning for an IM nail?
Supine on a radiolucent table
- Bump under ipsilateral hip
- Radiolucent triangle
What is the IM nail start point for standard tibia shaft fracture?
- AP view
* Just medial to the lateral tibia spine - Lateral view
* Just anterior to the articular surface
How is a true AP view of the knee obtained and what is the importance when selecting the start point for tibial IMN?
[Rockwood and Green 8th ed. 2015]
True AP = lateral aspect of the lateral tibial condyle bisects the head of the fibula
- Rotated AP view can change the appearance of the start point by as much as 15mm
What is the appropriate placement of the starting guidewire prior to opening reamer when doing a tibial IMN?
[Rockwood and Green 8th ed. 2015]
- AP view
* In line with the longitudinal axis - Lateral view
* Parallel to the anterior cortex
Where should the guidewire be positioned in the distal segment prior to reaming when doing a tibial IMN?
[Rockwood and Green 8th ed. 2015]
Level of physeal scar, centre-centre on AP and lateral views
In length stable tibial shaft fracture patterns, how can distraction at the fracture site be corrected when doing an IMN?
[Rockwood and Green 8th ed. 2015]
- Lock nail distally then ‘back slap’ the nail to achieve compression
- Compression screw used at proximal nail in most nailing systems
Summarize the steps of tibial IM nailing?
[Rockwood and Green 8th ed. 2015]
- Preoperative check
- Ensure adequate knee ROM
- Ensure canal is clear
- Ensure positioning devices available
- Ensure nail of appropriate size available
- Length and diameter
- Ensure reduction aids available
- Large bone clamps
- Femoral distractor
- Schanz pins
- Patient positioning
- Supine
- Radiolucent table
- Bump under ipsilateral hip
- Radiolucent triangle
- Fluoro from opposite side
- Approach
* Medial parapatellar - Identify start point with wire
- Advance wire into diaphysis
- Opening reamer advanced over wire
- Reduce fracture and advance ball tip guidewire across fracture into distal fragment
- Measure nail length
* Select nail shorter than measurement - Ream to 1.5mm larger than nail
- Lock proximally through outrigger and distally with perfect circle
- Confirm locking screws are through nail, fracture is reduced
- Irrigate and close wounds
- Full length radiographs postop to confirm alignment
What is the incidence of anterior knee pain following tibia IM nail?
[JBJS [Br]2006;88-B:576-80]
- 47.4% (range 10-86%) at a mean followup of 24 months
- Anterior knee pain is more frequently related to tibial nailing and in particular to a transtendinous approach, protrusion of the nail or a painful point of entry
What are the proposed etiologies of anterior knee pain following tibia IM nail?
[JAAOS 2018;26:e381-e387]
- Damage to intra-articular structures
* Eg. meniscus, ACL, cartilage, etc - Implant prominence
- Patellar tendon and fat pad
- Infrapatellar branch of the saphenous nerve
- Altered biomechanics and fracture motion
- Muscle deconditioning
What recommendations should be followed to avoid anterior knee pain following tibial IMN?
[JBJS [Br]2006;88-B:576-80]
- Skin incision away from area involved in kneeling
- Avoid infrapatellar branch of saphenous
* Limited incisions or horizontal incisions - Avoid protrusion of the nail (ensure countersunk)
- Locking screws should be appropriate length to avoid soft tissue irritation
- Avoid injury to the patellar tendon, fat pad and gliding tissues (use soft tissue protectors)
- Flexion of the knee to an angle greater than 100° should give minimum contact between the introducer and the patella, making the pressure changes at the patellofemoral joint less likely
When is plating of a tibial diaphyseal fracture indicated over IM nailing?
[Rockwood and Green 8th ed. 2015]
- Periprosthetic fracture (TKA)
- Tibia is too small for a nail
- Tibia canal is not patent or deformed from prior fracture
- Ipsilateral tibial plateau fracture
What percentage of tibia fractures are open?
[JAAOS 2010;18:108-117]
24%
What is the emergency department management of open tibial shaft fractures?
- ATLS and resuscitation
- Tetanus status
- Early antibiotics
- Neurovascular, compartment, soft tissue examination
- Debridement
- Irrigation
- Remove gross debris
- Cover with sterile permeable dressing
- Fracture reduction and splinting
What is the management of tetanus status in open fractures? [Orthobullets]
Dictated by immunization history and contamination of wound
- Doses
- Tetanus toxoid-containing vaccine dose is 0.5 mL intramuscular
- Tetanus immune globulin dose is 250 units intramuscular

What is the Gustillo classification of open fractures?
[JAAOS 2010;18:108-117]
Type I
- Clean wound <1cm in length
Type II
- Clean wound >1cm in length without extensive soft tissue damage, flaps or avulsions
Type IIIA
- Adequate soft tissue coverage despite extensive soft tissue damage, flaps or high energy trauma irrespective of wound size
Type IIIB
- Inadequate soft tissue coverage with periosteal stripping
- Often associated with massive contamination
Type IIIC
- Arterial injury requiring repair
*** For prognostic reasons, severely comminuted, contaminated barnyard injuries, close range shotgun/high velocity gunshot injuries, and open fractures presenting over 24 hours from injury have all been later included in the grade III group
What is the infection rate based on the Gustillo classification of open fractures?
[JAAOS 2010;18:108-117]
Type I - 0-2%
Type II - 2-10%
Type III - 10-50%
What is the recommended prophylactic antibiotic course following open tibial shaft fractures?
[JAAOS 2010;18:108-117]
- Initiate as soon as possible after injury
* Increased rate of infection in fractures managed with antibiotic prophylaxis >3 hours after injury compared with <3 hours after injury- 7.4% versus 4.7%, respectively
- Recommended 24-72 hours of antibiotic prophylaxis after initial surgical procedure
What is the recommended antibiotic depending on Gustillo type and contamination?
[Orthobullets]
Gustilo Type I and II
- 1st generation cephalosporin (Cefazolin)
- clindamycin or vancomycin can also be used if allergies exist
Gustilo Type III
- 1st generation cephalosporin (Cefazolin) + aminoglycoside (tobramycin, gentamycin)
Farm injuries, heavy contamination, or possible bowel contamination
- Add high dose penicillin for anaerobic coverage (clostridium)
Special considerations [JAAOS 2005;13:243-253]
- Fresh water wounds (Aeromonas hydraphila)
- Fluoroquinolones (Levofloxacin) or 3rd or 4th generation cephalosporin (eg. ceftazidime)
- Saltwater wounds (Vibrio species)
- Ancef/Ceftazidime + doxycycline

What is the recommended timing of the initial operative irrigation and debridement in an open fracture?
[JAAOS 2010;18:108-117]
- Most guidelines recommend within 6 hours of injury
- Gustillo type I can be delayed until the following morning
- Gustillo type III, highly contaminated should be done on an urgent basis
What are the principles of irrigation and debridement of open fractures?
[JAAOS 2010;18:108-117]
- Systematic debridement
* Start with removal of gross contamination, then layer by layer debridement - Excise all necrotic tissue
- Muscle viability assessed with ‘the 4 Cs’
- Color
- Contractility
- Capacity to bleed
- Consistency
- Irrigate with saline at low pressure
- 3 litres for Gustillo type I
- 6 litres for Gustillo type II and III
- Limit tourniquet use
- Can add ischemic insult to already compromised tissue
- Limits ability to determine tissue viability
- Repeat serial debridement in 48-72 hours in high energy injuries
- Wound closure
- Gustillo type I, II, IIIA = primary closure
- Recommend use of Donati-Allgöwer sutures to minimize the amount of cutaneous vascular compromise
- Gustillo type IIIB = alternate coverage
- Consider:
- NPWT
- Antibiotic bead pouch in bone defect covered by semi-permeable sterile dressing
- Masquelet technique with PMMA spacer for bone defects
- Consider:
What do the results of the FLOW trial tell us about irrigation solution and pressure?
[N Engl J Med 2015;373:2629-41]
- Rates of reoperation were similar regardless of irrigation pressure (high, low, very low)
* Indicates that very low pressure is an acceptable, low-cost alternative for the irrigation of open fractures - The reoperation rate was higher in the soap group than in the saline group
Note: Primary end point = reoperation
- Defined as surgery that occurred within 12 months after the initial procedure to treat an infection at the operative site or contiguous to it, manage a wound-healing problem, or promote bone healing
What are the recommended construct options at the time of initial operative management for an open tibial fracture?
[JAAOS 2010;18:108-117]
- IM nail
- Preferred over external fixation
- Better maintenance of length, alignment and rotation
- Less reoperation
- Better tolerated by patient and nursing
- External fixation
* Used for temporary stabilization in cases of massive soft-tissue damage or as part of a damage-control protocol
If external fixation is used for an open tibial fracture when should it be converted to an IM nail?
[JAAOS 2010;18:108-117]
- As soon as patient condition allows and soft tissue coverage has been attained
* Conversion to IM should occur within 28 days - Safety interval of <10 days should be used in the management of pin-tract infections, with débridement, irrigation, and antibiotics, to allow for pin-tract granulation before IM nailing
* “Safety interval” = period of casting or bracing between removal of the external fixator and IM nailing to allow granulation of pin sites
What 3 options can be considered for wound coverage with exposed bone at the time of initial surgical fixation?
[Petrisor]
“Vac, pack or Abx beads”
What has the use of BMP-2 in open tibia fracture management shown?
[JAAOS 2010;18:108-117]
- Less reoperation
- Accelerated fracture healing
- Less infections in Gustillo IIIA and IIIB
What flaps can be used for soft tissue coverage of a tibia fracture?
[JAAOS 2010;18:108-117]
- Proximal 1/3
* Gastrocnemius rotational flap - Middle 1/3
* Soleus rotational flap - Distal 1/3
- Free flap
- Free muscle flap
- Gracilis, rectus femoris, latissimus (small, medium, large)
- Free muscle flaps are covered by split thickness skin grafts
- Free fasciocutaneous flap
- Eg. Anterolateral thigh free flap
- ***NOTE – equal outcomes with free muscle and fasciocutaneous flaps
- Free muscle flap
When should soft tissue coverage be performed following an open tibial shaft fracture?
- “Early flap coverage of open fractures yields the best results in terms of bony union, complication, and infection rates when compared with intermediate or late closure, as defined by our review” [J Trauma Acute Care Surg. 2012 Apr;72(4):1078-85]
- Early = <72h
- Intermediate = 72h-7d
- Late = >7d
2. 7-10 days after injury [JAAOS 2010;18:108]
What distal tibia fractures have an association with posterior malleolar fractures?
[JOT 2016;30:S12–S16]
Spiral oblique pattern
What are the most common deformities of distal tibia fractures found during nailing?
[JAAOS 2018;26:629-639]
Valgus deformity (most common)
- Followed by recurvatum and varus
What technique can help to avoid the valgus deformity when nailing a distal tibia fracture?
[JAAOS 2018;26:629-639]
An anterior to posterior directed blocking screw in the medial one third of the distal tibia prevents medial nail positioning and subsequent valgus deformity
What are the advantages and disadvantages of IM nailing vs. plating vs. minimally invasive plating of a distal tibia extra-articular fracture?
[JAAOS 2012;20:675-683]
- IM nail
* Advantages- Minimal disruption of soft tissue envelope
- Protects extra-osseous blood supply
- Better in older patients with thin skin, diabetic patients, compromised soft tissue
- Biomechanically superior in axial loading stress
- Compared to medial plate
- Disadvantages
- Compared to medial plate
- Knee pain
- Less stable
- Increased malaligment, malunion, and nonunion
- Plate
- Advantages
- Direct reduction
- Improved biomechanics (twice as stiff)
- High rates of union
- Low incidence of infection, nonunion and malalignment
- Disadvantages
- High risk of soft tissue complications
- Avoid in diabetes, open fractures, hemorrhagic fracture blisters over desired incision
- High risk of soft tissue complications
- Minimially invasive plating
- Advantages
- Biologically friendly
- Better in more distal fractures and fracture patterns prone to malalignment
- Disadvantages
- Limits direct reduction
- Increased hardware prominence and irritation
What is the role of fibular plating in management of distal tibia fractures?
[JAAOS 2012;20:675-683]
- Absolute indication = syndesmosis disruption
- Relative indication = medial plating of the tibia to resist valgus deformation
- Advantages
- Improve construct stiffness
- Reduce late malalignment
- Disadvantages
- May increase nonunion
- Decreased strain across tibia fracture
What techniques can be used to obtain reduction of distal tibia fractures?
[J Orthop Trauma 2016;30:S7–S11]
- Universal distractor
- Schanz pins in proximal and distal tibial physeal scar
- Parallel to joint on AP
- Posterior to allow for nail passage
- Bent guide wire tip
- Percutaneous pointed reduction forcep
- Unicortical plate
- Rigid plate (3.5mm compression plate)
- Leave in place until locked proximally and distally
- Blocking screws or wires
- Large fragment screws
- Interlocking screws from nail set (off label)
- Steinmann pin or K-wire (2mm or greater)
- Consider ‘cascading wires’ to direct path of wire and nail
- Consider fixing the fibula
What are ways to increase stability of IM nail fixation for distal tibia fractures?
[JAAOS 2012;20:675-683] [JOT 2016;30:S7–S11]
- Add blocking screws, angle stable locking screws, more distal locking screws in multiple planes
- Similar to ex-fix principles
- Larger screws
- More screws
- Out of plane screws
- Screw spread proximal distal
In cases of distal tibia fractures with simple articular involvement, what is the sequence of fixation?
[JOT 2016;30:S12–S16]
- Anatomic reduction and stable fixation of articular surface
* Prevents nail from displacing articular surface - Then, reduction of extra-articular tibial fracture
- Then, insertion of IM nail
What is the recommended management of posterior malleolar fractures during IMN of distal tibia fractures?
[JAAOS 2018;26:629-639]
- Displaced posterior malleolar fractures can be reduced, followed by stabilization with an independent small-fragment screw(s), or an A-to-P interlocking screw through the nail
- There is no evidence to support routine fixation of small, nondisplaced posterior malleolar fragments
What is the postoperative management of distal tibia fractures?
[JAAOS 2006;14:406-414]
Usually nonWB 6-8 weeks but with early ROM
- WB started when evidence of callus formation is present
What is the deformity in proximal 1/3 tibial shaft fractures?
Valgus and procurvatum (apex anterior)
What are the deforming forces in proximal 1/3 tibia fractures?
[Orthobullets]
- Patellar tendon
- Pes anserine
- Gastrocnemius
- Anterior leg compartment
What surgical techniques can prevent the valgus (coronal plane) deformity?
[OITE review]
- More lateral start point
- Blocking screw lateral to midline in proximal segment
- Unicortical plating
- Universal distractor (Schanz pins medial tibia)
What surgical techniques can prevent procurvatum (sagittal plane) deformity?
[OITE review]
- Suprapatellar start point
- Semi-extended position
* Neutralizes extensor mechanism force - Start point more proximal
- Blocking screw posterior in proximal segment
- More proximal Herzog bend
* Stays within proximal fragment
What are some described reduction techniques for IM nailing a proximal tibia fracture?
[J Am Acad Orthop Surg 2014;22:665-673]
- Open reduction with unicortical plating
- Percutaneous reduction forceps
- Blocking screws
- Percutaneous Schanz pins as joysticks
- Femoral distractor applied medially with posterior positioning of the Schanz pins
- More proximal and lateral start point
- Suprapatellar nailing in semiextended position
What are theoretical disadvantages to suprapatellar nailing of proximal 1/3 tibia fractures?
[J Am Acad Orthop Surg 2014;22:665-673]
- Injury to patellar and femoral trochlear cartilage
- Iatrogenic injury to other intra-articular structures
- Joint sepsis
- Intra-articular retained reaming debris
- Challenge of nail removal
- Possible limited nail diameter due to the size of the cannula
- Need for technique-specific instrumentation
What are anatomical features of the tibial plateau?
- The medial tibial plateau has a concave shape and the lateral tibial plateau has a convex shape
* Helps to differentiate medial/lateral plateau on a lateral radiograph of the proximal tibia - The medial tibial plateau is larger in both length and width than the lateral tibial plateau
- The lateral tibial plateau lies proximal to the medial plateau
What imaging should be ordered for a tibial plateau fracture?
[Orthop Clin N Am 46 (2015) 363–375]
- Radiographs
- AP, lateral, obliques
- Tibial plateau view
- 10° caudad to parallel the tibial slope
- Generally not needed with use of CT
- Useful intraoperative view to assess reduction
- CT with 3D reconstruction
* Perform post ex-fix if significant comminution present
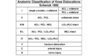
What is the classification system for tibial plateau fractures?
Schatzker
- Best interobserver agreement
- Agreement improves to excellent with addition of 3D reconstructions
- Schatzker I – split
- Schatzker II – split depressed (most common)
- Schatzker III – depressed
- Schatzker IV – medial condyle
- Schatzker V – bicondylar
- Schatzker VI – metaphyseal-diaphyseal dissociation

What are operative indications for tibial plateau fracture?
- Articular step-off >3mm
- Condylar widening >5mm
- Varus/valgus instability
- Medial condyle fractures
* Inherently unstable – Schatzker IV - Bicondylar fractures
* Schatzker V + VI - >5° of coronal alignment disruption [JAAOS 2018;26:386-395]
What are the goals of ORIF in tibial plateau fracture?
- Restoration of mechanical axis alignment
* ***Most important aspect - Restoration of condylar width
- Articular reduction
- Restoration of knee stability
What is the most common soft tissue injury associated with a tibial plateau fracture?
Lateral meniscus injury
- Usually peripheral tears
What injuries are commonly associated with a Schatzker IV (medial condyle fracture)?
- Knee dislocation
* Femur displaces with the medial fragment - Neurovascular injury (requires ABI)
- Compartment syndrome
What factor most significantly increases risk of developing post-traumatic arthritis following ORIF of tibial plateau fracture?
Failure to restore mechanical axis of limb
What substance has been shown to have the least articular surface subsidence when used to fill the bony void?
[Orthop Clin N Am 46 (2015) 363–375]
Calcium phosphate cement
- Can be injected after fixation
What Schatzker type is most commonly associated with nonunion?
[JAAOS 2018;26:386-395]
Schatzker VI injuries
- Usually the result of:
- Severe comminution
- Unstable fixation
- Failure to bone graft
- Mechanical failure of the implant
- Infection
- Or a combination of these factors.
What is the anterolateral approach for tibia plateau ORIF?
- Inverted L incision (hockey stick) ~1cm below joint line and 1cm lateral to the anterior tibial crest with the curve over Gerdy’s tubercle
* Alternative is a lazy S extending proximally - Expose the joint capsule and the fascia overlying the tibialis anterior
- Incise the fascia over the tibialis anterior and elevate the tibialis anterior off the tibial periosteum
- Incise the capsule transversely then incise the coronary ligament to create a submeniscal arthrotomy
What is the posteromedial approach for tibia plateau ORIF?
- Longitudinal incision is made along the posteromedial tibial border on the medial side of the medial head of gastroc
- Incise the fascia along the posterior border of pes anserinus
- Place a retractor along bone of posterior tibia to retract the medial head of gastroc
* Subperiosteal elevation of popliteus may be required
What are treatment options for Schatzker I (simple split) fractures?
[Orthop Clin N Am 46 (2015) 363–375]
Indirect reduction and percutaneous fixation
- Technique:
- Leg placed on a radiolucent triangle
- Perform a tibial plateau view
- Confirm reduction with a large pointed reduction clamp
- Hold provisionally with K-wire
- Place partially threaded cannulated screws with washers
- Minimum 2 proximal and 1 distal
- Sequentially tighten each screw

What are treatment options for Schatzker II (split-depression) fractures?
[Orthop Clin N Am 46 (2015) 363–375]
Buttress plating
- Anterolateral approach
- Lazy-S, hockey stick or lateral incision centred over Gerdy’s
- Submeniscal arthrotomy
- Working through the fracture
- Book open with laminar spreader
- Elevate the depressed joint surface
- Provisional fixation with K-wire
- After reduction is confirmed (visualization and fluoro), apply a 3.5mm precontoured periarticular locking plate
- Nonlocking screws distally and locking screws proximally under articular surface
- Rafting screws
- Nonlocking screws distally and locking screws proximally under articular surface
- Fill bone void
- Repair the meniscus

What are the treatment options for complex, high energy tibial plateau fractures?
[Orthop Clin N Am 46 (2015) 363–375]
Delayed fixation
- Apply spanning ex-fix with pins outside the zone of injury and zone of future plate placement
- Obtain CT after application of ex-fix
- Definitive fixation when soft tissues allow
- Skin wrinkling, minimal blisters
- May require multiple surgical approaches
- Consider staging operations
- Medial then lateral or vice versa
What is the rate of popliteal artery injury with knee dislocation?
[J Am Acad Orthop Surg 2015;23:761-768]
Average = 16% (range 1.6-40%)
What nerve is at greatest risk in a knee dislocation?
[J Am Acad Orthop Surg 2015;23:761-768] [Orthop Clin N Am 46 (2015) 479–493]
Common peroneal nerve
- Usually a traction palsy
- Rarely transected unless open
- Peroneal palsy occurs in 25% of dislocations with 50% recovery of function
- Higher incidence (44%) in ultra-low energy mechanisms
- Typically obese patients
What are the ways in which knee dislocations can be classified?
[J Am Acad Orthop Surg 2015;23:761-768]
- Based on the direction of the tibia displacement relative to femur (Kennedy classification)
- Anterior
- Most common direction
- Caused be hyperextension mechanism
- Sequential failure of posterior capsule, PCL and sometimes ACL
- Popliteal artery injury usually an intimal tear due to traction
- Posterior
- Second most common
- Caused by posteriorly directed force to proximal tibia
- Popliteal artery injury usually a transection
- Medial
- Lateral
- Rotatory
- PCL remains intact as tibia rotates about the femur
- Schenk classification
- PCL remains intact as tibia rotates about the femur
- Based on severity/pattern of ligamentous damage
- KD I (1 crucuate)
- ACL or PCL injured
- +/- collaterals
- KD II (2 ligs)
- ACL and PCL injured
- KD III (3 ligs)
- ACL, PCL
- Medial OR lateral collateral
- KD IV (4 ligs)
- ACL, PCL, MCL, LCL
- KD V
- Fracture dislocation
NOTE: For KD III injury, the injury is written as KD IIIM or KD IIIL, depending on whether the medial or lateral collateral ligament is damaged.
- The subdesignations C and N indicate the presence of vascular and neural injury, respectively
What imaging is recommended in a knee dislocation?
[J Am Acad Orthop Surg 2015;23:761-768]
- Prereduction AP and lateral knee xray
- Postreduction AP and lateral knee xray
- CT scan if periarticular or intraarticular fracture identified on xray
- MRI obtained after successful reduction
What is the recommended reduction technique for a knee dislocation?
[J Am Acad Orthop Surg 2015;23:761-768]
- Conscious sedation
- Reverse the deformity
- Once reduced splint the knee in 20° flexion,
* Plaster splint preferred - Postreduction xray to confirm reduction
What is the dimple sign in context of a knee dislocation?
[Orthop Clin N Am 46 (2015) 479–493]
Occurs when the medial femoral condyle buttonholes through the medial capsule and entraps the MCL drawing it into the joint
- Often represents an irreducible dislocation
What is the algorithmic approach to assessing for vascular injury in the dislocated knee?
[J Am Acad Orthop Surg 2015;23:761-768]
- Pre- and post reduction assess for ‘hard signs’ of vascular injury and palpate pulses (DP and PT)
- Hard signs:
- Cold
- Pale
- Delayed capillary refill
- Pulsatile hematoma
- Absent pulse
- If pulses are absent or hard signs present, vascular surgery consult (no ABI) for emergent vascular exploration
- If pulse is present assess symmetry of pulse and ABI
- If asymmetrical pulse or ABI <0.9 = CT angiogram (CTA)
- If pulses symmetric and ABI >0.9 = admit for 24h observation with serial examination and ABIs
What are indications for a preoperative joint-spanning external fixator in a knee dislocation?
[J Am Acad Orthop Surg 2009;17:197-206]
- Open dislocation
- vascular repair
- Reduction not maintained in splint
Is open or arthroscopic ligament reconstruction preferred post knee dislocation?
[J Am Acad Orthop Surg 2009;17:197-206]
The preferred treatment of knee dislocations under ideal circumstances consists of:
- Arthroscopic ACL and PCL reconstruction
- Open LCL/PLC and/or MCL/PMC reconstruction
What is the recommended order of ligament repair/reconstruction post knee dislocation?
[J Am Acad Orthop Surg 2009;17:197-206]
PCL → ACL → PLC → PMC
- PCL is reconstructed first to restore native anatomic tibiofemoral relationship and to prevent posterior displacement of the tibia with ACL tensioning
Should the ligaments be repaired or reconstructed post knee dislocation?
[J Am Acad Orthop Surg 2009;17:197-206]
- Reconstruct ACL, PCL, and PLC
- Repair or reconstruct PMC
What are the preferred graft choices for ligament reconstruction?
[J Am Acad Orthop Surg 2009;17:197-206][J Knee Surg 2012;25:287–294]
- PCL
- Achilles tendon allograft for single bundle
- Achilles tendon allograft (anterolateral) and tibialis anterior allograft (posteromedial) for double bundle
- ACL
* Achilles tendon or other allograft - PLC
* Achilles allograft - PMC
* Allograft - two semitendinosis grafts or one anterior tibialis graft
What is the recommended timing for fixation of multiligamentous knee injuries?
[J Am Acad Orthop Surg 2009;17:197-206]
- In general for ACL/PCL + PLC or PMC injuries:
* If capsule is disrupted precluding arthroscopy first repair/reconstruct the PLC or PMC in the first week then do arthroscopic reconstruction of the ACL/PCL at 3-6 weeks - For ACL, PCL and PLC injuries timing is dependent on:
- Fanelli and Feldmann classification:
- Type A = increase in external rotation only
- Injury to the popliteofibular ligament and popliteus tendon
- Type B = increase in external rotation and increased varus laxity of approximately 5 mm at 30° of flexion
- Injury to the popliteofibular ligament, popliteus tendon, and LCL
- Type C = increase in external rotation and gross varus laxity of approximately 10 mm at 30° of flexion
- Injury to the popliteofibular ligament, popliteus tendon, LCL, and lateral capsule
- Type A = increase in external rotation only
- Type A and B
- Single stage arthroscopic ACL/PCL recon with open lateral side recon in first 2-3 weeks
- Type C
- Staged open lateral side recon in first week with arthroscopic ACL/PCL recon at 3-6 weeks
- For ACL, PCL and PMC injuries timing is dependent on:
- Fanelli and Harris classification
- Type A = axial rotation instability (either anteromedial or posteromedial) with no valgus instability
- Type B = axial rotation instability and valgus laxity at 30° of flexion with a firm end point
- Type C = axial rotation instability and valgus laxity at 30° of flexion with no end point
- Type A and B
- Single stage arthroscopic ACL/PCL recon with open medial side repair/recon in first 2-3 weeks
- Type C
- Staged open medial side repair/recon in first week with arthroscopic ACL/PCL recon at 3-6 weeks


