Thrombosis, Embolus, and Shock Flashcards
What is extravasation?
Into tissues?
Into body spaces?
Happens due to what?

Normally, hydrostatic and osmotic forces are nearly balanced.
Extravasation of fluid into tissues (edema) and spaces (effusion).
Due to:
1- Increases in capillary hydrostatic pressure and decreases in plasma oncotic pressure.
2- Increased vascular permeability
3- Exceeds capacity for lymphatic drainage

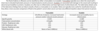
What is the difference between a transudate and an exudate?
What are some of the cuases for transudate? For exudate?

Fluid out of the vessels can be classified as:
Transudate
Happens due to Increased hydrostatic pressure
Reduced oncotic pressure
Exudate
Due to Increased vascular permeability
Inflammation –> Endothelial cell contraction creates small gaps
Direct damage to endothelial cells.
Increases blood volume
What is hyperemia? Color of tissue?
What is Congestion? Color of tissue?

Hyperemia
Physiologic: Active increase in blood inflow
-Arteriolar dilation
-Oxygenated blood: red (erythema)
Congestion
Pathologic: Passive
-**Impaired venous outflow
Deoxygenated blood: pale or red/blue
Hyperemia and congestion examples

Left heart congestions leads to what issues?
Right heart congestion affects what?
Left heart congestion first causes pulmonary edema and pleural effusion. Then, there is a decrease in renal blood-flow, which leads to H2O and Na+ accumulation that increases the blood volume. This increase in blood volume leads to peripheral tissue inflammation (edema).
Right heart congestion leads to liver congestions (since it is the place where blood comes from to the vena cava/right atrium), which leads to splenic congestion. Liver congestion also leads to GI tract varices and ascites (protein containing fluid in the abdomen).

What is hemorrhage?
What are some causes?
-Blood outside of the vasculature, due to vessel damage.
Causes:
-Impaired integrity of vessel walls
-Low level/function of platelets
-Low level/function of coagulation factors

How big are petechia?
How big is a purpura?
How big are ecchymoses?

What is thrombosis? What is it composed of?
What three factors from the Virchow triad promote thrombosis?
Where is it more common in the body?

Thrombosis is an intravascular mass attached to the vessel that is composed of varying proportions of coagulating factors, RBCs, and platelets.
Endothelial injury, hypercoagulability, and abnormal blood flow are the three factors in the Virchow triad.
It is more common in the venous system because of slower blood flow, with the veins in the lower extremeties as the most common site.

Thromboembolus (piece of thrombus)
What are some of the causes of deep vein thrombosis?
*Most common type of embolus
Deep Vein Thrombosis
Immobility, recent surgery
Estrogen
Pregnancy or post-partum
Previous or current cancer
Coagulation abnormalities
Limb trauma and/or orthopedic procedures
Obesity

Pulmonary Embolus
What is an embolus?

A free floating, intravascular mass of a solid, liquid or gas is an embolus.
- It can be carried by the blood from its site of origin to other areas of the body until it becomes lodged in a vessel too small to pass through.
- Most emboli are detached thrombi, or fragments of thrombi, called thromboemboli. Other types of emboli include fat, atherosclerotic debris, gas bubbles, bone marrow, tumor fragments, amniotic fluid or foreign material. The clinical consequence of vessel blockage depends on the size of the vessel, the organ/tissue involved, and whether complete or partial vessel occlusion occurs. Emboli in the venous/right sided system most commonly lodge in the lungs. Emboli in the arterial/left sided system can affect any organ, but most commonly travel to the legs or brain.

Embolus
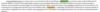
Thromboemboli-venous comes from the ____1________, organ affected is the ____2_____, and clinical outcome is ____3______.
Fat-bone marrow emboluscomes from the ____1________, organ affected is the ____2_____, and clinical outcome is ____3______.
Thromboemboli-veins
1- Deep leg veins, arms veins
2- lungs
3- Respiratory insufficiency and chest pain.
Fat-bone marrow
1- Long-bone fractures-vein damage
2- lungs
3- respiratory insufficiency 1-3 days post trauma, mental status changes

What is disseminated intravascular coagulation (DIC)?
Disseminated intravascular coagulation (DIC) is a unique condition where thrombosis and hemorrhage can occur simultaneously.
- Generalized activation of clotting leads to widespread thrombosis with subsequent consumption of platelets and clotting factors. This creates a deficiency of platelets and clotting factors that then results in bleeding.
-This systemic activation of thrombin can be caused by any underlying condition that results in release of procoagulants, such as tissue factor, into the circulation or by widespread endothelial cell injury.
DIC often presents clinically with anemia, respiratory insufficiency, convulsions, acute renal failure and shock. Bleeding typically dominates in acute onset of DIC, and thrombosis typically dominates with chronic DIC.

Disseminated Intravascular Coagulation:
What are some of the symptoms?
Symptoms from multiple organ systems:
- Respiratory insufficiency
- MSC, Convulsions
-Acute renal failure
-Petechiae/Purpura
-GI, oral hemorrhage
–>Shock
Hemolytic anemia, thrombocytopenia, low fibrinogen, elevated D-dimer and other fibrin degradation products
What is infarction?
What causes it?
Typically what kind of necrosis seens?
Where do liquefactive necrosis happens?
Tissue death (necrosis) caused by vessel occlusion
Typically coagulative necrosis (preservations of the structural outline of the dead cells)
Liquefactive necrosis (necrotic degradation of tissue that softens and becomes liquified) in the brain

What is the difference between red and white infarction?
In which organs do red and white infarts occur?
What shape are infarcts?
Thrombosis and emboli commonly lead to severe tissue ischemia and infarction.
Infarcts are areas of tissue death (necrosis) caused by ischemia.
The loss of adequate blood flow can be due to obstruction of arterial blood supply or venous drainage.
Infarcts can be classified as red (hemorrhagic) or white (anemic).
White:
Features associated with white infarcts are an arterial blockage, a single blood supply, and a dense tissue that limits accumulation of blood in necrotic areas.
Where does it occur? Heart, kidney, and spleen.
Red:
Features favoring formation of a red infarct include venous occlusion, a dual blood supply and loose tissue that permits movement of blood from adjacent areas into the necrotic area. A red infarct can form after an arterial occlusion if blood flow is subsequently reestablished and damaged vessels allow movement of blood into the necrotic area.
Where does it occur? Lungs, liver, intestine
Most infarcts are roughly wedge‐shaped due to arborization of blood vessels from the arterial supply.

What is shock?
What is cardiogenic shock? What are some of its causes?
What is myocardial shock? What are some of its causes?
Shock occurs when the circulating blood volume or blood pressure is not adequate to perfuse body tissues –> multiorgan dysfunction/damage
Cardiogenic Shock: failure of the heart to pump an adequate amount of blood and/or generate arterial blood pressure to perfusse distal tissues. Myocardial pump failure.
Caused by? Myocardial damage, extrinsic compression, outflow obstruction
Hypovolemic Shock: occurs when there is not enough blood volume to widely perfuse all tissues, and the cardiac output decreases because there is low blood return to the heart. –>Low blood volume.
Causes? Severe dehydration (vomiting, diarrhea), hemorrhage, burns
Both

Shock
Septic shock
What is it?
What systemic effects does it have?
How does it present by patient?
Is it responsive to IV fluids?
Septic shock is a subtype of shock due to systemic inflammation (SIRS).
It occurs when microbial infections cause high levels of inflammatory mediators in the blood leading to:
-widespread arterial vasodilation
- vascular leakage and venous blood pooling.
This in turn results in hypotension and decreased tissue perfusion.
–>Septic shock typically initially presents with warm, flushed skin and fever.
-Usually not responsive to IV fluids.

What is anaphylactic shock?
Neurogenic shock is characterized by?
Anaphylactic shock: caused by an allergic reaction
-Arterial vasodilation
-Vascular leakage
Neurogenic Shock: Loss of vascular tone, caused by:
-Anesthesia
-Spinal cord injury


