Metastasis Flashcards
(26 cards)
What is invasion?
What is metastasis?
Invasion and metastasis: characteristics of malignant tumors.(benign tumors don’t invade or metastasize)
–> Invasion - the infiltration of adjacent tissues
by malignant cells.
Metastasis - the transfer of malignant cells from
the primary site to a non-connected (secondary)
site. In other words, metastases are tumors discontinuous with the primary tumor.
What is “carcinoma in situ”?
In which tissues is it common?
Do in situ epithelial cancers display cytologic features of malignancy?
Do they eventualy penetrate the basement membrane?
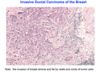
Pre-invasive stage referred to as “carcinoma in situ.”
Common in carcinomas of the skin, breast, and certain other sites.
In situ epithelial cancers display the cytologic features of malignancy without invasion of the basement membrane.
May be considered one step removed from invasive cancer, since, with time, many penetrate the basement membrane and invade into the stroma.

What is a characteristic of malignant tumors?
Malignant tumors are often poorly demarcated from the surrounding normal tissue.
-Tumor protruding into surrounding tissue in a crablike fashion – hence the name “cancer”

Dissemination of cancer may occur by what three ways?
Do malignant tumors recognize anatomic barriers?
Why is their surgical removal often very difficult?
Dissemination of cancers may occur through one of 3 pathways:
(1) direct seeding of body cavities or surfaces (ex: ovarian cancer: tumors come from fallopian tube into the ovary, and disseminate into the peritoneal cavity and into the organs, basically it means coming directly out of their origin into other areas.)
(2) lymphatic spread (spread through lymph nodes).
(3) hematogenous spread (through the blood).
Most malignant tumors are obviously invasive. Can penetrate the wall of organs such as the colon or uterus.
They recognize no normal anatomic boundaries!
Surgical resection often difficult or impossible: even if tumor appears well circumscribed, need to remove a large margin of normal tissue adjacent to the infiltrative neoplasm.
Why is it advantegeous for tumors to move beyond basement membrane?
What is necessary for tumors to get bigger than 1 mm?

In the primary tumor it becomes advantageous to move beyond basement membrane when conditions get crowded & harsh (hypoxia caused by limited blood supply, waste products and lack of nutrients).
Then there is selective pressure to “move out” or metastasize

What are some emerging hallmarks of tumors?
What can inflammation by innate immune cells can cause to cancer in some cases?
Emerging Hallmarks and Enabling Characteristics:
- Modify cellular metabolism to support neoplastic proliferation.
- Evade immunological destruction.
Because neither capability is yet generalized and fully validated, they are labeled as emerging hallmarks.
- Genomic instability genetic alterations that drive tumor progression.
- Inflammation by innate immune cells designed to fight infections & heal wounds, but can be tumor promoting.

The bigger the tumor the GREATER the chance that it will metastasize?

What are the steps for a carcinoma metastasize?
How does the carcinoma invades the Extracellular matrix (ECM)?
What E-Cadherin is lost?
How is it in the extravasation process?
Tumor cells interact with extracellular matrix (ECM) at several stages during invasion.
Carcinoma cells must
1) breach the underlying basement membrane
2) traverse the interstitial connective tissue,
3) gain access to the circulation by penetrating the vascular basement membrane (intravasation).
Invasion of the ECM is an active process that can be resolved into several steps:
–>Changes “loosening up” of tumor cell-cell interactions:
loss of E-cadherin, for example
–> Degradation of ECM
–> Attachment to ECM components
–>Migration of tumor cells
Process is repeated in reverse when tumor cells extravasate at a distant site.
Step 1 of invasion: Dissociation of cells from one another - alterations in adhesion molecules.
Are normal epitheliam cells usually attach to each other?
What holds epithelial cells together? What are E-cadherins connected to in the intracellular side?
Normal epithelial cells _attached to each othe_r and surroundings via adhesion molecules.
Cell-cell interactions mediated by cadherin family of transmembrane glycoproteins.
Epithelial cells are held together by E-cadherin. On the intracellular side E-cadherins are connected to β-catenin and the actin cytoskeleton.
In epithelial tumors, such as colon and breast carcinomas, E-cadherin is often down-regulated, reducing the ability of cells to adhere to each other and facilitating detachment from the primary tumor and invasion into the surrounding tissues.
2nd step of invasion: local degradation of the basement membrane and interstitial connective tissue.
Tumors secrete what to degrade the basement membrane?
What enzymes regulate tumor invasion? How?
Cleavage products of what have chemotactic, angiogenic, and growth-promoting factors?
What does MMP9 does?
What is amoieboid migration?
Tumor cells secrete proteolytic enzymes or induce stromal cells to make them.
Matrix Metallo-Proteases (MMPs) regulate tumor invasion by:
1) remodeling insoluble components of the basement membrane
2) releasing ECM-sequestered growth factors. Cleavage products of collagen and proteoglycans have chemotactic, angiogenic, and growth-promoting effects.
Example: MMP9 is a gelatinase that cleaves type IV collagen of epithelial and vascular basement membrane & stimulates release of VEGF from ECM-sequestered pools.
Different type of movement:
In vivo imaging shows that tumor cells can adopt a 2nd mode of invasion, termed ameboid migration in which cell squeeze through spaces in the matrix instead of using proteases. Ameboid migration is quicker, and tumor cells use collagen fibers as “highways.”
Tumor cells, can switch between the two forms of migration, perhaps explaining the disappointing performance of MMP inhibitors in clinical trials.
3rd step in invasion: involves changes in attachment of tumor cells to ECM proteins.
Epithelial cells have recepts on their basal surface such as:____
in their basement membrane such as:_______
What is anoikis? What causes it?
Normal epithelial cells have receptors, such as integrins at their basal surface, for basement membrane laminin and collagens.
-These receptors help to maintain the cells in a resting, differentiated state.
–>Loss of adhesion to the basement membrane in normal epithelial cells leads to induction of apoptosis (anoikis, or death by detachment).
Metastatic tumor cells are resistant to this form of cell death.
Additionally - matrix itself is modified in ways that promote invasion and metastasis.
For example, cleavage of collagen IV and laminin in basement membrane by matrix metalloproteases, MMP2 or MMP9 (secreted by tumor cells) generates novel sites that bind to receptors on tumor cells and stimulate migration.

What is the 4th step of invasion?
What are the steps involved?
Locomotion is the 4th and final step of invasion, propelling tumor cells through the degraded basement membranes and zones of matrix proteolysis in ECM.
Cells must attach to the matrix at the leading edge, detach from the matrix at the trailing edge, and contract the actin cytoskeleton
to ratchet forward.

Motility
What is a paracrine effector of cell motility produced by stromal cells?
What is collective motility?
Cleavage products of matrix components (e.g., collagen, laminin) and some growth factors (e.g., IGFs I and II) have chemotactic activity for tumor cells.
Proteolytic cleavage can liberate growth factors bound to matrix molecules.
Stromal cells produce paracrine effectors of cell motility, such as hepatocyte growth factor (HGF) or scatter factor, which bind to receptors on tumor cells.
Collective motility refers to cancer cells traveling together without loosing their adhesions.
Loss of E-cadherin is often associated with the invasive phenotype:
What are some ways to loose E-cadherin?
Some of the ways that E-cadherin expression is lost include:
- Loss of heterozygosity
- Inactivating mutation (rare)
- Silencing of gene expression via hypermethylation of promoter
- Transcriptional repressors (Snail, Slug, Twist, ZEB1/2)
What transcription factors promote Epithelial-to-Mesenchymal transition?
What do they repress?

Transcription factors SNAIL,TWIST, and ZEB1/2 promote epithelial-to mesenchymal transition (EMT) by repressing E-cadherin.

Epithelial to Mesenchymal Transition is a Normal Process During Development that gets used Inappropriately by Cancer Cells.
Why is it abnormal?
It should not be happening in adult cells, they should not be moving pass the embryonic stage.
Epithelial to Mesenchymal Transition - where in the
Metastatic Cascade is it thought to be Necessary?
What are some changes Associated with EMT?
What are mesenchymal proteins that are upregulated?
Is process reversible?
It is used in intravasation (epithelial to mesenchymal) and extravation (mesenchymal to epithelial) of metastatic cancer

Downregulation (decrease in) epithelial proteins;
–E-cadherin
–Cytokeratins
•Upregulation (increased) mesenchymal proteins:
–Vimentin
–Fibronectin
–N-cadherin
–Motility and invasiveness
–Increased protease secretion
–Fibroblast-like morphology
•Important to note that not all these changes always occur and the process is reversible
What are characteristics of tumor microenvironment?
What cells exhibit altered expression of ECM molecules, proteases, protease inhibitors, and various growth factors?
1) Mesoderm derived Cells
fibroblasts
adipocytes
immune cells
endothelial cells
2) Extracellular matrix
(ECM) i.e. collagen, etc
3) Soluble & matrix-associated growth factors, cytokines, proteases
Tumor cells live in a complex, ever-changing milieu composed of ECM, growth factors, fibroblasts, and immune cells, with significant cross-talk among all the components.
ECM not merely a static barrier for tumor cells to traverse but instead represent an environment in which reciprocal signaling can affect tumor suppression or progression.
Tumor-associated fibroblasts exhibit altered expression of ECM molecules, proteases, protease inhibitors, and various growth factors.
Vascular Dissemination and Homing of Tumor Cells
What are tumor cells vulnerable to once in circulation?
What might increase tumor survial once they are in the circulation? To which cells do they agreggate with?
Once in the circulation, tumor cells vulnerable to destruction by:
- mechanical shear stress
- apoptosis stimulated by loss of adhesion (anoikis)
- immune defenses.
In the circulation, tumor cells can aggregate in clumps. Adhesions between tumor cells and blood cells, particularly platelets, may enhance tumor cell survival and implantability. Tumor cells can bind and activate coagulation factors, resulting in the formation of emboli.
Arrest and extravasation of tumor emboli at distant sites involves adhesion to the endothelium, followed by egress through the basement membrane. Involves adhesion molecules (integrins, laminin receptors & proteolytic enzymes).
Extravasation:
Where do the tumor cells get out of blood or lymph vessels?
Organ tropism
Where do prostatic carcinoma prefers to spread?
Where do bronchogenic carcinomas tend to migrate?
What about neuroblastomas?
Extravasation: Site at which circulating tumor cells leave the capillaries can be due to the anatomic location of the primary tumor (1st capillary bed available to the tumor). However, the natural pathways of drainage do not fully explain the distribution of metastases.
Examples:
- prostatic carcinoma preferentially spreads to bone
- bronchogenic carcinomas tend to involve the adrenals and the brain
- neuroblastomas to liver & bones
What two theories attempted to explain cancer tropism?
Which one is better?
Two main theories proposed to explain organ tropism of cancer metastasis include:
“seed and soil” theory by Stephen Paget in 1889 - proposed that organ-specific patterns were explained by the needs of the cancer cell (the seed) for a specific environment (the soil) to initiate and maintain growth.
Ewing’s mechanical arrest theory - proposed thirty years later, postulated that cells mechanically arrest in the first capillary bed encountered.
Two theories are not mutually exclusive, but rather work in concert to produce successful metastases: cells arrest due to mechanical obstruction and chemical signals and then require suitable microenvironment for maintenance of secondary tumor growth (colonization).
What are the steps of extravasation?
To which theory do they most likely correlate to?
Do some tissues resist metastasis? Which are some examples?
1) First step in extravasation is adhesion to the endothelium: tumor cells express adhesion molecules and the endothelial cells of the target organ express ligands for the adhesion molecules. Endothelial cells of vascular beds of various tissues differ.
2) Chemokines: Breast cancer cells express chemokine receptors and the tissues that the cancer cells commonly metastasize to express the chemokine. Some target organs may liberate chemoattractants that recruit tumor cells to the site such as IGF1 and
3) Some tissues are nonpermissive environment—”unfavorable soil” for the growth of tumor seedlings.
Example- though well vascularized, skeletal muscle is rarely the site of metastases.
As an example of where some cancer cells like to metastasite, what chemokine receptors are expressed in breast cancer that hace chemokines produced by the tissues they usually metastasize to?
Breast cancer cells express chemokine receptors such as CXCR4. Chemokines that bind to these receptors (CXCL12 /SDF-1) are highly expressed by tissues that breast cancers commonly metastasize to (lungs, liver, bone).




