Inflammation Flashcards
What are the cardinal signs of inflammation?
Is inflammation the same as disease?
What are the vascular components of inflammation?
What is the cellular component?
Inflammation is simplistically defined by redness, heat, pain, swelling….and because of all these things, there may be a decrease in the normal function of the tissues affected by the inflammatory reaction.
Many folks often hear the term inflammation and equate to a disease state. However, this is not entirely true; inflammation is not a disease but rather a normal response to bodily invaders.
We now know that the purpose of inflammation is to bring phagocytic cells to the injured area to engulf/destroy the offending agent.
*Vascular component: increased vascular permeability, vasodilation, endothelial injury
Cellular component: Neutrophils extravasate from circulation to injured tissue to participate in inflammation through phagocytosis, degranulation, and inflammatory mediator release.

What are the two main types of inflammation?
Acute inflammation is associated with what immune system?
What about chronic?
What is granuloma?
There are 2 main types of inflammation
-Acute and chronic
Acute is mostly associated with the INNATE immune system which is fairly non-specific but very FAST
Chronic is mostly associated with the ADAPTIVE immune system; much SLOWER, but quite specific
Acute: Neutrophil, eosinophil, and antibody mediated. Acute inflammation is rapid onset (seconds to minutes), lasts minutes to days. Outcomes include complete resolution, abscess formation, and progression to chronic inflammation.
Chronic: Mononuclear cell mediated: characterized by persistent destruction and repair. Associated with blood vessel proliferation, fibrosis.
Granuloma: nodular collections of epithelioid macrophages and giant cells. Outcomes include scarring and amyloidosis.

What happens to blood vessels during an inflammatory reaction?
What happens to endothelium cell that line blood vessels?
The typical inflammatory reaction develops through a series of sequential steps:
- The offending agent, which is located in extravascular tissues, is recognized by host cells and molecules.
- Leukocytes and plasma proteins are recruited from the circulation to the site where the offending agent is located.
major participants in the inflammatory reaction in tissues are blood vessels and leukocytes.
Blood vessels:
- dilate to slow down blood flow
- increase their permeability
- Enable selected circulating proteins to enter the site of infection or tissue damage.
Endothelium (cells) lining blood vessels become leaky:
White blood cells (leukocytes)
- circulating WBCs come to a stop
- then migrate into the tissues –> become activated
- WBCs in tissues acquire the ability to ingest and destroy microbes, dead cells, foreign bodies and other unwanted materials….

The vascular response:
What is a blister? What is transudate?
What is edema?
The vascular reactions of acute inflammation consist of changes in the flow of blood and the permeability of vessels, both designed to ____1______ the movement of plasma proteins and leukocytes out of the circulation and into the site of infection or injury

Blisters: a transudate is a fluid with _low protein conten_t (most of which is albumin), little or no cellular material, and low specific gravity. It is essentially an ultrafiltrate of blood plasma that is produced as a result of osmotic or hydrostatic imbalance across the vessel wall without an increase in vascular permeability
-Figure 3-13: Serous inflammation. Low-power view of a cross-section of a skin blister showing the epidermis separated from the dermis by a focal collection of serous effusion.
Edema: an excess of fluid in the interstitial tissue or serous cavities; it can be either an exudate or a transudate.
1- Maximize

The Vascular Response
What are its three components?
Describe the components of vasodilation?
Where does vasodilation slows the blood flow?
What do cellular components of blood due when vasodilation happens? What is this called?
What hormone/citokine is the predominant chemical released by inflammation?
What open first, arterioles or capillary beds?
1-Vasodilation
2- Increased Vascular permeability
3- Blood stasis
Vasodilation slows the blood flow at the POST CAPILLARY VENULE.
–>When vasodilation occurs, the larger (cellular) components of blood will move towards the periphery of the blood vessel (MARGINATION)
–>Vasodilation is predominantly mediated by HISTAMINE which acts on the vascular smooth muscle cells.
–>Arterioles are acted upon first and then capillary beds are opened
Vasodilation causes an increase in blood flow to that area which will produce redness and heat (we visualize this externally as ERYTHEMA)
–>The main result of changes to the blood vessels is delivery of necessary cells and blood proteins to the threatened area of the body.
–>This is accomplished by dilating the vessels that serve that area and making them more permeable (or “leaky”).
–>The result of these vascular changes is an exudate that swells (i.e. tumor) the affected tissues.

Vascular permeability:
Vasodilation is followed by what?
What caused vascular permeability?
When protein-rich fluids leave the blood vessels and enter into the tissues, this is see from the outside as?
Endothelial cell contraction is in immediate responses is caused by?What about in long-ter (hours)?
Vasodilation is quickly followed by increased permeability of the microvasculature, with the outpouring of protein-rich fluid into the extravascular tissues.
blood vessels become leaky (increase in VASCULAR PERMEABILITY)—this is mediated by HISTAMINE and KININS (any of a group of substances formed in body tissue in response to injury. They are polypeptides and cause vasodilation and smooth muscle contraction)
–protein-rich fluids leave the blood vessel and enter into the tissues (we see this externally as EDEMA or swelling)
As the blood slows, WBCs towards the periphery of the blood vessels are able to extravasate (or leave the blood vessel) and move into the affected tissue
1) Endothelial cell contraction
- Immediate (minutes): initiated by histamine
- Longer-term (hours): initiated by cytokines (IL-1, TNF)
2) Direct
- Toxic compounds/events injure endothelial cells
e. g. thermal burn, some bacterial toxins - Cells die or detach, leaving incomplete endothelium
3) Transcytosis
Vesicles transport material from vessel lumen to the extravascular tissues

Blood stasis:
What is stasis?
What does stasis allows?
The loss of fluid and increased vessel diameter lead to slower blood flow, concentration of red cells in small vessels, and increased viscosity of the blood.
STASIS is seen as vascular congestion and localized redness of the involved tissue.
As stasis develops, WBCs (neutrophils) accumulate along the vascular endothelium.
At the same time endothelial cells are activated by mediators produced at sites of infection and tissue damage, and express increased levels of adhesion molecules.
WBCs then adhere to the endothelium, and soon afterward they migrate through the vascular wall into the interstitial tissue
Slowing of the blood (or STASIS) allows WBCs to accumulate
- Endothelial cells are activated by _____and begin expressing greater numbers of adhesion molecules
- WBCs adhere to endothelium and eventually exit the vessel and enter the tissues

Transudate vs. Exudate


Why does our skin becomes red? What mediates this?
Why do we blister? What kind of fluid composes blisters?

The Cellular component

What triggers the cellular response?
- Triggered by tissue damage or pathogens
- Influx of inflammatory cells
–->Increased vascular permeability = WBC extravasation
Rolling
P- selectin, where is it stored? Who makes it be released?
E-Selectin, it’s induced by? In what type cells is it located?

Adhesion

Integrins are expressed in ______ affinity state and are upregulated by ______ and ________.
•Integrin ligands (VCAM1, ICAM1) are on endothelial cells, and are Induced by____ and _____.

Transmigration

Platelet endothelial cell adhesion molecule-1 (PECAM-1) is expressed on all cells within the vascular compartment.
expressed to different degrees on most leukocyte sub-types, platelets, and on endothelial cells
Endothelial cells = its expression is largely concentrated at junctions between adjacent cells.
PECAM-1 can respond to various stimuli.
very little is known about regulation of expression of PECAM-1

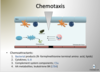
Chemotaxis
What is it?
What are some of the chemoattractants?

Chemotaxis is the movement of an organism in response to a chemical stimulus. Somatic cells, bacteria, and other single-cell or multicellular organisms direct their movements according to certain chemicals in their environment
Summary of migration of neutrophils to the outside of blood vessels?

Recognition
Toll-Like Receptors
What are they?
What transcription factors do they activate?

Recognition
NOD-like receptors (NLRs)
Where are they located?
Signal via what protein complex?
What is an inflammasone?

Inflammasone us a cytoplasmic protein complex that recognizes products of dead cells, microbial products, and crystals (uric acid)–> activation of IL-1 and inflammation response.

Ways to eliminte microbes?

Examples of phagocytosis

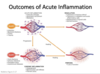
Outcomes of acute inflammation:
BUT, in general, three possible outcomes
1.Resolution
2.Chronic inflammation
3.Scarring
- Complete resolution. In a perfect world, all inflammatory reactions, once they have succeeded in eliminating the offending agent, should end with restoration of the site of acute inflammation to normal. This is called resolution and is the usual outcome when the injury is limited or short-lived or when there has been little tissue destruction and the damaged parenchymal cells can regenerate. Resolution involves removal of cellular debris and microbes by macrophages, and resorption of edema fluid by lymphatics.
- Healing by connective tissue replacement (scarring, or fibrosis). This occurs after substantial tissue destruction, when the inflammatory injury involves tissues that are incapable of regeneration, or when there is abundant fibrin exudation in tissue or in serous cavities (pleura, peritoneum) that cannot be adequately cleared. In all these situations, connective tissue grows into the area of damage or exudate, converting it into a mass of fibrous tissue, a process also called organization.
- Progression of the response to chronic inflammation (discussed later). Acute to chronic transition occurs when the acute inflammatory response cannot be resolved, as a result of either the persistence of the injurious agent or some interference with the normal process of healing.
Leukocyte Adhesion deficiency:

There is lack of ____ in bacterial infections.
- Autosomal recessive defect of INTEGRINS
- Increased circulating PMNs (leukocytosis, neutrophilia)
–Normal: ~50% PMNs in marginated pool (adhesion to BV)
–Defective adhesion = no significant marginated pool
•Inability to extravasate
•Recurrent bacterial infections that lack pus formation
–>PMNs can’t get out into the tissues
•Delayed separation of the umbilical cord
–Normal: decreased blood flow –> necrosis
•PMNs follow necrosis (“janitors”)
–No extravascular PMNs = difficultly in separation

Chédiak-Higashi Syndrome
Pyogenic means full of pus
Why is neutropenia see?

Autosomal recessive LYST gene mutation-defect in lysosomal trafficking regulator gene.
- Protein trafficking defect
- microtubule disfunction in phagosome-lysosome fusion.
•Neutropenia (can’t divide properly due to microtubule defects) + impaired phagolysosome formation
–Increased risk of pyogenic infections
•Defective primary hemostasis
–Dependant on platelets, and platelet granules
•Peripheral neuropathy
–Unable to get information from spinal nerve to the peripheral nerve



