Therapeutics Flashcards
Explain the MoA of Loop Diuretics
- Inhibits Na-K-Cl Co-Transporter (NKCC) in the Thick Ascending limb of the Loop of Henle reducing absorption of NaCl.
- This causes an increase in tubular reabsoprtion of Na+ (leading to diuresis and natriuesis)
- Downstream, Na-K+ of prinicipal cells of collecting duct respond to increased Na+ by reabsorption of Na+

Explain the MoA of Thiazide Diuretics
- Inhibits the thiazide-sensitive Na-Cl symporter in the DCT of the Loop of Henle
- Resultant increased Na+ in tubule, which stimulates Aldosterone-sensitive Na+ pump to increase Na+ reabsorption in exchange for K+ and H+ ions
- K+ loss can lead to Hypokalaemia
- Activation of RAAS due to reduced blood volume and arterial pressure
- Most commonly used diuretic.

Explain the MoA of K+ Sparing Diuretics
- 2 Types: Epithelial Sodium Channel (ENaC) Antagonists (Act on the DCT) OR Aldosterone Antagonists (Act on the Cortical Collecting Duct)
- Aldosterone Receptor Antagonists (distal segment of the tubule) act on Aldosterone-Sensitive Na+ Pump
- Resultant Na+ (and water) passes into the collecting duct and is excreted into urine
- ENaC antagonists - similar effect to MoA above.
- Less K+ is exchanged and therefore ‘K+ sparing’
- Often used in conjuction with Loop/Thiazides to prevent Hypokalaemia
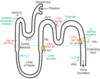
Explain the MoA of Carbonic Anhydrase Inhibitors
- Inhibit the transport of bicarbonate out of the PCT into the interstitium
- Resultant less Na+ reabsorption
- Greater Na+ (Natiuresis), HCO3 (Bicarb) and Water loss (Diuresis) in the urine
- Similar to Loop/Thiazide Diuretics, can lead to hypokalaemia
- Weak Diuretic. Used mainly for treatment of Glaucoma

Give 2 Indications for Loop Diuretics, with examples of Diuretics
- Heart failure: both acute (usually intravenously) and chronic (usually orally)
- Resistant hypertension, particularly in patients with renal impairment
- Furosemide/Bumetanide
Give 2 Indications for Thiazide Diuretics, with examples of Diuretics
- Step 2 and 3 for NICE Management of Hypertension
- Treatment of Mild HF
- Bendroflumethiazide/Indapamide

Give 2 Indications for K+ Sparing Diuretics, with examples of Diuretics (Aldosterone and ENaC Antagonists)
- Amiloride - given alongside Loop/Thiazide Diuretics as an alternative to K+ supplementation
- Spironolactone - Ascites, HF, Nephrotic Syndrome or Conn’s Syndrome
Describe the common adverse effects of Loop Diuretics
- hypotension
- hyponatraemia
- hypokalaemia, hypomagnesaemia
- hypochloraemic alkalosis
- ototoxicity
- hypocalcaemia
- renal impairment (from dehydration + direct toxic effect)
- hyperglycaemia (less common than with thiazides)
- gout
Describe the common adverse effects of Thiazide Diuretics
- dehydration
- postural hypotension
- hyponatraemia, hypokalaemia, hypercalcaemia*
- gout
- impaired glucose tolerance
- impotence
Describe the common adverse effects of K+ Sparing Diuretics
- Main risk is Hyperkalaemia - must be used with caution in patients on ACE-Inhibitors
Describe the Management of Chronic Heart Failure, include drug examples (1st and 2nd Line)
- ACE-Inhibitor (1st Line) - Ramipril, Lisinopril and Enalapril etc.
- Beta-Blocker (1st Line) - Bisoprolol, Carvedilol and Nebivolol
- Aldosterone/Mineralocorticoid Antagonists (2nd Line) - Spironolactone and Eplerenone: Offer in HFrEF if they continue to have symptoms of HF. Contraindicated in Renal Impairment.
- Diuretics - Loop Diuretics to relieve SOB/Oedema - Furosemide/Bumetanide
NB: When initiating ACE inhibitors, ARBs and aldosterone antagonists Check:
- U&Es, Renal function & BP prior to starting treatment, 1-2 weeks after starting treatment, and at each dose increment.
- Once the target, or maximum tolerated dose is achieved, treatment should be monitored monthly for 3 months and then at least every 6 months, and if the patient becomes acutely unwell.
- When initiating beta blockers, heart rate, blood pressure and symptom control should be assessed at the start of treatment and after each dose change.
- In patients with chronic kidney disease, lower doses and slower dose titrations of ACE inhibitors, ARBs, aldosterone antagonists and digoxin should be considered.
https://bnf.nice.org.uk/treatment-summary/chronic-heart-failure.html
Give some examples of 3rd Line Treatments for Chronic HF
Third-line treatment should be initiated by a specialist. Options include ivabradine, sacubitril-valsartan, hydralazine in combination with nitrate, digoxin and cardiac resynchronisation therapy
- Ivabradine - criteria: sinus rhythm > 75/min and a left ventricular fraction < 35%
- Sacubitril-valsartan - criteria: left ventricular fraction < 35%. Considered in HFrEF who are symptomatic on ACE inhibitors or ARBs. Should be initiated following ACEi or ARB wash-out period.
- Digoxin - digoxin has also not been proven to reduce mortality in patients with heart failure. It may however improve symptoms due to its inotropic properties. It is strongly indicated if there is coexistent atrial fibrillation.
- Hydralazine in combination with nitrate - this may be particularly indicated in Afro-Caribbean patients
- Cardiac resynchronisation therapy (CRT) - indications include a widened QRS (e.g. left bundle branch block) complex on ECG
https://bnf.nice.org.uk/treatment-summary/chronic-heart-failure.html
Give some examples of non-drug treatments for Chronic Heart Failure
- Lifestyle changes: Smoking cessation, reducing alcohol consumption, increasing physical exercise if appropriate, weight control, and dietary changes such as increasing fruit and vegetable consumption and reducing saturated fat intake.
- Patients should be encouraged to weigh themselves daily at a set time of day and to report any weight gain of more than 1.5–2.0 kg in 2 days to their GP or heart failure specialist.
- Salt and fluid intake should only be restricted if these are high, and a salt intake of less than 6 g per day is advised. Patients with dilutional hyponatraemia should only restrict their fluid intake. Salt substitutes containing potassium should be avoided to reduce the risk of hyperkalaemia.
- Contraception and pregnancy should be discussed with women of childbearing potential and heart failure. Advice from a heart failure specialist and an obstetrician should be sought if pregnancy occurs or is being considered.
- Patients should be given the opportunity to join a personalised rehabilitation programme including education, psychological support, and exercise when appropriate.
- Implantable cardioverter defibrillators (ICDs) and cardiac resynchronisation therapy (CRT) are treatment options recommended in patients with heart failure and a reduced ejection fraction <35%. If symptoms remain severe and unresponsive despite optimal drug treatment, specialist referral should be considered.
https://bnf.nice.org.uk/treatment-summary/chronic-heart-failure.html
Which vaccines should be offered in HF?
- offer annual influenza vaccine
- offer one-off pneumococcal vaccine
- adults usually require just one dose but those with asplenia, splenic dysfunction or chronic kidney disease need a booster every 5 years
Which Drugs should be avoided in HF?
- Rate-Limiting Calcium Channel Blockers - Avoid verapamil, diltiazem and short-acting dihydropyridine agents in HFrEF
- Short-Acting Dihydropyridines - nifedipine, or nicardipine hydrochloride
Give an example of Alternative Treatments for HF if ACE-Is are not tolerated
- Consider an ARB licensed for heart failure as an alternative to an ACE inhibitor for people who have HFrEF and intolerable side effects with ACE inhibitors
- Examples: Candesartan cilexetil, Losartan potassium, or Valsartan
- Measure U&Es, Renal Function and BP before and after starting an ARB and after dose increments.
- Once target or maximum dose is reached, monitor treatment monthly for 3m then at least every 6m and at anytime the individual becomes acutely unwell.
- If neither ACE inhibitors nor ARBs are tolerated, seek specialist advice and consider hydralazine in combination with nitrate for people who have heart failure with reduced ejection fracti
- https://www.nice.org.uk/guidance/ng106/chapter/recommendations#treating_hfref
Describe the treatment of HFrEF in individuals with CKD
HFrEF and CKD with an eGFR of 30 ml/min/1.73 m2 or above:
- Offer 1st Line treatment
- If eGFR is 45 ml/min/1.73 m2 or below, consider lower doses and/or slower titration of dose of ACE inhibitors or ARBs, MRAs and digoxin.
- If eGFR below 30 ml/min/1.73 m2, the specialist heart failure MDT should consider liaising with a renal physician.
- Monitor the response to titration of medicines closely, taking into account the increased risk of hyperkalaemia.
https://www.nice.org.uk/guidance/ng106/chapter/recommendations#treating_hfref
Describe the indications for Ivabradine in HF according to NICE
- New York Heart Association (NYHA) class II to IV stable chronic heart failure with systolic dysfunction and
- who are in sinus rhythm with a heart rate of 75 bpm or more and
- who are given ivabradine in combination with standard therapy including beta-blocker therapy, ACE-inhibitors and aldosterone antagonists, or when beta-blocker therapy is contraindicated or not tolerated and
- LVEF 35% or less.
- Ivabradine should only be initiated after a stabilisation period of 4 weeks on optimised standard therapy with ACE inhibitors, beta-blockers and aldosterone antagonists.
- Ivabradine should be initiated by a HF specialist with access to a MDT HF team. Dose titration and monitoring should be carried out by a heart failure specialist, or in primary care by either a GP with a special interest in heart failure or a heart failure specialist nurse.
Condition
Epidemiology
Aetiology
Clinical Features
Investigations
Management
Condition
Epidemiology
Aetiology
Clinical Features
Investigations
Management
Condition
Epidemiology
Aetiology
Clinical Features
Investigations
Management
Condition
Epidemiology
Aetiology
Clinical Features
Investigations
Management
Condition
Epidemiology
Aetiology
Clinical Features
Investigations
Management
Condition
Epidemiology
Aetiology
Clinical Features
Investigations
Management


