SIADH Flashcards
(18 cards)
Which of the following may be used to treat hyponatraemia caused by SIADH? (2)
- Fluid restriction
- Hydrocortisone
- Demeclocycline
- Hypertonic sodium chloride 1.8% IV
Fluid restriction - in mild cases
Hypertonic NaCl 1.8% IV in severe cases.
What are the symptoms of hyponatraemia?
- Confusion
- Seizures
- Anorexia
- Nausea
- Muscle weakness
A 76-year-old lady presents to the ED with nausea, generalised weakness and dizziness. She has no significant PMH and takes no medications. She is a life long smoker of 60 cigarettes per day. She is thin. Urine dip shows protein +. She has Na of 122mmol/L.
What is the most likely cause of her hyponatraemia?
- Cardiac failure
- Nephrotic syndrome
- Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
- Addison’s disease
SIADH caused by malignancy - she is a heavy smoker and has weight loss. All others cause hyponatraemia but..
Cardiac failure - she has no signs of left or right ventricular failure (oedema).
Nephrotic syndrome - mild proteinuria and no peripheral oedema
Addison’s disease - no hypotension or postural drop
What are the two diagnostic findings for hyponatraemia in SIADH?
- Urine osmolality > 100 mOsmol/Kg (not maximally dilute)
- Plasma osmolality < 270 mosmol/Kg
Other:
- Urine sodium - elevated - >40mmol/L
- Hyponatraemia - Na<125mmol/L
- Should also check normal renal, adrenal and thyroid function
How do diuretics cause hyponatraemia?
Loop diuretics prevent reabsorption in the ascending limb of the loop of Henle
How do you manage SIADH?
Mild cases:
- Fluid restriction
Severe cases require to raise plasma sodium concentration to avoid pontine and extra-pontine myelinolysis
- Hypertonic sodium chloride 1.8% IV -
- Demeclocycline - in resistant forms; blocks renal tubular effect of ADH
Define SIADH.
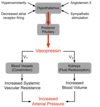
Syndrome of inappropriate antidiuretic hormone (SIADH) is defined as euvolaemic, hypotonic hyponatraemia secondary to impaired free water excretion, usually from excessive arginine vasopressin (AVP)/ADH release
What would the urine osmolality be in SIADH?
Concentrated
>100 mmol/kg H2O (>100 mOsm/kg H2O)
How common is SIADH?
Hyponatraemia is common (N <135) in hospital setting - affects 15-20%
Overhydration (21%), mainly iatrogenic, is the leading cause of hyponatraemia, while SIADH accounts for 8%
In 21% of people the condition was of acute duration and in 79% it was of chronic duration
What is the aetiology of SIADH?

What are the main mechanisms for AVP release?
Osmotic pressure sensed by osmoreceptors in the hypothalamus. Osmotic pressure is greatly influenced by sodium concentration.Decrease in osmolality of 1-2% suppresses AVP release and induces free water diuresis
Arterial pressure reduction (10-20%) can stimulate AVP release, sensed by baroreceptors in the left atrium and aorta. This lowers set point of the osmoregulatory system causing AVP release.
Non-osmotic stimuli for AVP release - stress, nausea, pain, vasovagal stimulation.
Inappropriate release of AVP occurs with malignancy, pulmonary processes, central nervous system disorders, and certain drugs.
How is SIADH classified?
Type A -unregulated release of AVP (30%).
Type B - slow leak of AVP (30%).
Type C - reset osmostat (30%). AVP levels rise inappropriately during hypertonic saline infusion before hyponatraemia is corrected.
Type D: pseudo-SIADH (10%). Low or undetectable AVP. Low levels of AVP during hyponatraemic state + apparent normal osmoregulation of AVP. Antidiuresis occurs through an alternative mechanism, through nephrogenic syndrome of inappropriate diuresis (SIAD), a genetic disorder w/ mutation of V2 receptor.
What are the risk factors for SIADH?
- age >50yrs
- Pulmonary conditions
- Nursing home - 18% of nursing home residents have been found to have serum sodium levels ≤135 mmol/L
- Malignancy - small cell lung cancer, GI, genito-urinary, lymphoma, sarcoma.
- Medicine with SIADH induction - SSRIs, amiodarone, carbamazepine, chlorpromazine, amitriptyline, NSAIDs, and chemotherapeutic agents
- CNS disorder - CNS infection, brain masses, cerebral trauma, or CVA
- Postoperative state - causing non-osmotic AVP release
- Endurance exercise - causing excess fluid intake.

What are the signs and symptoms of SIADH?
- Euvolaemia
- Linked to brain oedema:
- Nausea
- Vomiting
- Altered mental status
- Headache
- Seizure
- Coma
Findings of hyper/hypovolaemia suggest a different cause. Must also exclude hypothyroidism and adrenal insufficiency as they can cause euvolaemic hyponatraemia.
What investigations would you do for SIADH?
- Serum sodium - <135mmol/L
- Serum osmolality - low <280mmol/kg
- Urine sodium - high >40mmol/L
- Urine osmolality - >100mmol/kg
- Serum urea - <3.6mmol/L
- Urea - low
- Serum uric levels - low
- TSH - normal
- Cortisol - normal
- Normal saline infusion trial (only in those with suspected volume depletion) - serum sodium does not improve with 1-2L normal saline in SIADH. May even decrease serum Na.
- Plasma ADH/AVP - >2.5picograms/mL
- Serum cortisol level - morning level >138 nanomol/L
- Fractional excretion of sodium and urea - >1% and >55% respectively
How do you manage SIADH? (asymptomatic, mil/moderate, severe symptoms)
Asymptomatic - fluid restriction and treat underlying cause e.g. infection, stress, medication.
Mild/moderate symptoms -
- Acute onset - treat cause and fluid restrict
- Chronic onset (>48hrs) - treat cause and give vasopressor receptor antagonists e.g. tolvaptan
Severe symptoms -
- Acute onset - IV hypertonic saline (start w/ 50 mL 3% saline, followed by 200 mL infusion over 4 to 6 hrs) and fluid restriction. Treat cause and give furosemide if at risk of volume overload.
- Chronic onset - IV hypertonic saline and Na checked every 1-2hrs (start w/ 200 mL 3% saline over 4 to 6 hrs). Give tolvaptan once Na corrected. Treat cause and give furosemide.
What is a serious complication of SIADH?
Central pontine myelinolysis (CPM or osmotic demyelination syndrome) - Occurs in people with longstanding SIADH who undergo overaggressive treatment of hyponatraemia. CPM is characterised by demyelination of pontine, basal ganglion, and cerebellar regions.

This patient has hyponatraemia. What is shown?

Right paratracheal mass. This is likely to be malignant – it may represent adenopathy or a paratracheal mass lesion (look at the image below – arrows show mass).



